Infection Prevention and Control/Surface Decontamination: Difference between revisions
m →Sampling and Validation: This sections requires expansion |
|||
| (67 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
[[Infection Prevention and Control/Air Disinfection| Return to Air Disinfection]] | |||
==== | ==Decontamination== | ||
Decontamination is the process of making an area safe by removing, neutralising or destroying any harmful substances. Decontamination can be achieved by applying physical agents, chemical agents or mechanical removal through any combination of cleaning, disinfection or sterilisation. Physical agents could include heat, radiation and chemical agents include a myriad gasses and liquids. | |||
===Cleaning=== | |||
Cleaning is the process of achieving a state where an area is visually free of contaminating debris. Cleaning is generally achieved by the application of mechanical removal and liquid chemical agents. Cleaning is often an initial decontamination process which removes organic matter from an area. Such organic matter can promote microbial growth and protect microorganisms during further decontamination stages such as disinfection or sterilisation. Cleaning is also frequently applied as the final decontamination stage during which inactivated microorganisms or residual toxins are removed from an area. | |||
===Disinfection=== | |||
Disinfection is the decontamination process of reducing the number of infectious agents to the level where they no longer cause disease. Disinfection typically does not remove bacterial spores. | |||
===Sterilisation=== | |||
Sterilisation is any decontamination process which removes or kills all forms of life in an area. This includes viruses, bacteria, funguses and spores forming organisms. | |||
==Surface Decontamination by Cleaning== | |||
Before cleaning, a strategy must be available which identifies target organisms, areas, processes, tools and chemical agents appropriate to the area. A review of the high touch areas in the space will inform the strategy. The selection of chemical agents should be based on their intended function (rates of cleaning or disinfection) and the resistance of the target surfaces to potentially corrosive agents. A final cleaning should be done with chemical agents and tools that remove residues from other processes leave no additional unwanted residues. | |||
==Surface Decontamination by Heat== | |||
Decontamination by heat is typically a sterilisation process with some measure of cleaning beforehand. Surface decontamination by heat is not a common practice and the temperature/time dose function typically requires long exposure times due to the low heat tolerance of surfaces.<br> | |||
Two heat sterilisation processes are available, wet and dry heat. <br> | |||
'''Wet heat''' is considered the most dependable method of sterilisation. Steam sterilisers or autoclaves apply heat and humidity under pressure (using saturated steam at 121 °C and 104 kPa) to sterilise laboratory and medical equipment. The application of steam allows for better penetration of heat through permeable insulating layers on any surface than dry heat alone. Autoclaves are occasionally used to sterilise infectious waste.<br> | |||
'''Dry heat''' sterilisation is less dependable than wet heat as layers of debris on a surface can insulate organic materials from the process. Dry heat sterilisation is appropriate for impermeable surfaces like glass, but higher temperatures and exposure times are required (160 – 170 °C for periods of 120 to 240 minutes). | |||
==Surface Decontamination by Chemicals== | |||
{{stub}} | |||
==Surface Decontamination by Irradiation== | |||
Ionising and non-ionising irradiation are both able to decontaminate surfaces. Ionising radiation is not considered generally safe and practical for surface decontamination in a clinical or laboratory setting. Non-ionising radiation such as ultraviolet light in the UV-C band effectively inactivates most microorganisms on surfaces and in the air. | |||
=== | ===Surface Decontamination by Ultraviolet Germicidal Irradiation=== | ||
The disinfection effect of ultraviolet light has been described for over 100 years<ref> Downes, Arthur; Blunt, Thomas P. (19 December 1878). https://royalsocietypublishing.org/doi/pdf/10.1098/rspl.1878.0109</ref>. It is effective against a variety of microorganisms and has been successfully deployed for the purpose of disinfection of water, air and surfaces. Effectiveness depends on a range of variables related to the microorganism of interest, environment and application. Ultraviolet radiation in the UV-C range has been used for its germicidal properties specifically for infection prevention and control - have been demonstrated to work at laboratory scale, in ducts, as upper room irradiation and as portable devices. Safety guidelines have been established (ACGIH)<ref name="cite" | The disinfection effect of ultraviolet light has been described for over 100 years<ref> Downes, Arthur; Blunt, Thomas P. (19 December 1878). https://royalsocietypublishing.org/doi/pdf/10.1098/rspl.1878.0109</ref>. It is effective against a variety of microorganisms and has been successfully deployed for the purpose of disinfection of water, air and surfaces. Effectiveness depends on a range of variables related to the microorganism of interest, environment and application. Ultraviolet radiation in the UV-C range has been used for its germicidal properties specifically for infection prevention and control - have been demonstrated to work at laboratory scale, in ducts, as upper room irradiation and as portable devices. Safety guidelines have been established (ACGIH)<ref name="cite">Citation Needed</ref>.<br> | ||
UVGI surface disinfection has advantages over chemical disinfection because: | |||
*There is no off-gassing of chemicals or residual chemical contamination frequently associated with chemical-based disinfection methods. Therefore, vehicles or spaces can be occupied immediately after UVGI disinfection<ref name="Kowalski 2009">Wladyslaw Kowalski, 2009. Ultraviolet Germicidal Irradiation Handbook: UVGI for Air and Surface Disinfection. New York. Springer. [https://www.springer.com/gp/book/9783642019982]</ref>; | |||
*There is no off-gassing of chemicals or residual chemical contamination frequently associated with chemical-based disinfection methods. Therefore, vehicles or spaces can be occupied immediately after UVGI disinfection<ref name="Kowalski 2009">Wladyslaw Kowalski, 2009. Ultraviolet Germicidal Irradiation Handbook: UVGI for Air and Surface Disinfection. New York. Springer. [https://www.springer.com/gp/book/9783642019982]</ref>; | *It has high pathogen reduction rates when compared to chemical cleaning; and | ||
*It has high pathogen reduction rates when compared to chemical cleaning; and | |||
*Chemical disinfection methods are time-consuming <ref name="Kostyuchenko 2009">Sergey Kostyuchenko, Anna Khan, Sergey Volkov, Henk Giller, 2009. UV Disinfection in Moscow Metro Public Transport Systems. IUVA News / Vol. 11 No. 1 [https://iuvanews.com/stories/pdf/archives/110101KostyuchenkoEtAl_Article.pdf]</ref>. | *Chemical disinfection methods are time-consuming <ref name="Kostyuchenko 2009">Sergey Kostyuchenko, Anna Khan, Sergey Volkov, Henk Giller, 2009. UV Disinfection in Moscow Metro Public Transport Systems. IUVA News / Vol. 11 No. 1 [https://iuvanews.com/stories/pdf/archives/110101KostyuchenkoEtAl_Article.pdf]</ref>. | ||
A guideline on hospital infection control <ref name="Brown 1996">Brown IW Jr et al (1996) Toward further reducing wound infections in cardiac operations. Ann Thorac Surg 62(6):1783–1789.[https://www.ncbi.nlm.nih.gov/pubmed/8957387]</ref><ref name="Shamim 2017">Shamim, I. A. ed., 2017. Ultraviolet Light in Human Health, Diseases and Environment. Cham, Switzerland: Springer International Publishing AG.[https://www.springer.com/gp/book/9783319560168]</ref> recommends the use of both UVGI and chemical disinfection since UVGI has no penetrating power on dust, dirt and grease, which may harbour microbial contamination. Exposure to UV-C may degrade some materials.<br> | A guideline on hospital infection control <ref name="Brown 1996">Brown IW Jr et al (1996) Toward further reducing wound infections in cardiac operations. Ann Thorac Surg 62(6):1783–1789.[https://www.ncbi.nlm.nih.gov/pubmed/8957387]</ref><ref name="Shamim 2017">Shamim, I. A. ed., 2017. Ultraviolet Light in Human Health, Diseases and Environment. Cham, Switzerland: Springer International Publishing AG.[https://www.springer.com/gp/book/9783319560168]</ref> recommends the use of both UVGI and chemical disinfection since UVGI has no penetrating power on dust, dirt and grease, which may harbour microbial contamination. Exposure to UV-C may degrade some materials.<br> | ||
For UVGI surface disinfection for SARC-CoV-2, refer to [[Infrastructure_Guidance_for_COVID-19/COVID-19_Infection_Prevention_and_Control#Ultraviolet_Surface_Disinfection_for_SARS-CoV-2|COVID-19 infection control guidance]] | |||
The effective band of germicidal ultraviolet (GUV) radiation is between wavelengths of 250-270 nm with 265 nm the optimum efficiency. Ultraviolet Germicidal Irradiation effectively destroys most microorganisms on surfaces. Dirt, dust, and shadows can shield organisms which must be directly exposed to the GUV light. This and safety concerns are limiting factors for its general application.<br> | |||
The application of UVGI for surface disinfection usually involves the use of bare UVGI lamps. Two main approaches to surface disinfection systems are via permanently installed disinfection systems and portable disinfection systems. Permanently installed systems generally consist of bare UVGI lamp fixtures mounted on ceilings or walls. Portable UVGI systems are moved into a place temporarily to decontaminate surfaces <ref name="Kowalski 2009" />. | |||
The application of UVGI for surface disinfection usually involves the use of bare UVGI lamps. Two main approaches to surface disinfection systems are via permanently installed disinfection systems and portable disinfection systems. Permanently installed systems generally consist of bare UVGI lamp fixtures mounted on ceilings or walls. Portable UVGI systems are moved into a place temporarily to decontaminate surfaces <ref name="Kowalski 2009"/>. | |||
Efficacy is dependent on the intensity of irradiation emitted from the device, proximity of the device to the surface being disinfected and exposure time. The reflectivity of the materials in the vicinity of exposure can increase or decrease efficacy. Shaded items not directly exposed to UV-C irradiation may not effectively be disinfected | Efficacy is dependent on the intensity of irradiation emitted from the device, proximity of the device to the surface being disinfected and exposure time. The reflectivity of the materials in the vicinity of exposure can increase or decrease efficacy. Shaded items not directly exposed to UV-C irradiation may not effectively be disinfected | ||
---- | |||
====UVGI Efficacy==== | |||
:'''UVGI dose''' | |||
= | The UV-C dose required to achieve a particular pathogen reduction rate is calculated from the single-stage decay equation: | ||
S=e<sup>-kD</sup> | |||
where:<br> | |||
;*S is the Survival fractional [%]<br> | |||
;*k is the UVGI rate constant [m2/J]<br> | |||
;*D is the UVGI exposure dose [J/m2]<br> | |||
==== | The required UVGI dose for a 4 log reduction (99.99% pathogen reduction rate) is calculated by expressing the single-stage decay equation as follows: | ||
ln(''S'')=-''k''·''D''·ln(''e'') | |||
∴''D'' = (ln (0.0001))/(-k) '' mJ/cm<sup>2</sup>'' ''(J/cm<sup>2</sup>)'' | |||
---- | |||
====UVGI Validation==== | |||
Validation testing for UVGI surface disinfecting systems is required to ensure that the UV dose for ≥99.99% level of pathogen inactivation is achieved. As the dose rate is a function of the UV sources output and its distance to the target, the manufacturer for non-static UVGI surface disinfecting systems should specify the design minimum distance away from a surface, the UVGI intensity on the surface and the time required to achieve ≥99.99% pathogen reduction.<br> | |||
For disinfection that has either dynamic source or target components, repeatability and confidence studies are required to ensure that the range of variability expected does not exceed acceptable limits for efficacy and safety | |||
=== | ====UVGI Safety==== | ||
=== | Studies of personnel practising proper UVGI exposure control measures have shown no harmful effects<ref name="Brown 1996" />, <ref name="Shamim 2017" /> . Noncompliance with safety precautions can lead to injuries <ref name="Shamim 2017" />. The following safety issues are associated with the handling of UV equipment.<br> | ||
UV radiation exposure present hazards to the skin and the eyes <ref name="Kowalski 2009" /> <ref name="Myung 2005">Myung C. J., 2005. Ultraviolet (UV) Radiation Safety. Environmental Health and Safety University of Nevada Reno. [https://www.unr.edu/ehs/program-areas/radiation-safety/ultraviolet]</ref>. | |||
The | =====UVGI Exposure Guidelines===== | ||
The ability of UV radiation to penetrate the eyes and skin depends on the wavelength, therefore the UV radiation exposure Threshold Limit Values (TLV) for the eyes and skin published by the American Conference of Governmental Industrial Hygienists (ACGIH) <ref name="ACGIH" /> also varies according to the UV wavelength. For UVGI at 254 nm, a cumulative exposure dose greater than 6mJ/cm2 <ref name="ACGIH" /> is considered harmful to eyes and skin. Since UVGI surface disinfection systems use bare lamps with dose requirements exceeding 6 mJ/cm<sup>2</sup>, adherence to PPE is highly recommended to avoid harm. | |||
=====Eye Safety===== | |||
The UV wavelength is the determining factor as to which part(s) of the eye may absorb the radiation and suffer biological effects.<br> | |||
The table below shows the absorption of different UV wavelengths by the human eye.<br> | |||
=== | |||
The UV | |||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+Absorption of UV wavelengths in the Human Eye <ref name="Myung 2005" /> | ||
!Wavelength {nm}!!Cornea!!Aqueous!!Lens!!Vitreous | |||
! | |||
|- | |- | ||
| | |100-280||100%||0%||0%||0% | ||
|- | |- | ||
| | |300||92%||6%||2%||0% | ||
|- | |- | ||
| | |320||45%||16%||36%||1% | ||
|- | |- | ||
| | |340||37%||14%||48%||1% | ||
|- | |- | ||
|360||34%||12%||52%||2% | |||
|} | |} | ||
UVGI (UV wavelengths 200 to 280nm) cumulative exposure dose greater than 6mJ/cm2 <ref name="ACGIH">American Conference of Governmental Industrial Hygienists (ACGIH), 2019. Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. ACGIH: USA [https://www.acgih.org/forms/store/ProductFormPublic/2019-tlvs-and-beis-with-7th-edition-documentation-cd-rom-single-user-version]</ref> can cause temporary corneal injuries (photokeratitis and conjunctivitis <ref name="Kowalski 2009" />). Symptoms of corneal injuries (extreme pain in the eyes) present after 6 -12 hours of exposure and lasts for a few days during which corneal cells will recuperate <ref name="Kowalski 2009" /><ref name="Shamim 2017" />. | |||
=====Skin Safety===== | |||
Because of poor penetration and absorption capability <ref name="Brown 1996" />, UVGI cannot penetrate or cause permanent harm to human skin <ref name="Myung 2005" />. Some skin irritation or [https://en.wikipedia.org/wiki/Erythema erythema] may be experienced but this will generally clear up with proper care. | |||
====UV control measures==== | |||
=====Administrative controls===== | |||
Prevent unauthorized personnel from entering the UV radiation area. | |||
=====Personal protective equipment (PPE)===== | |||
Personal protective equipment (PPE) protects the wearer from harm due to UV radiation exposure. The following PPE should be worn when operating UVGI surface disinfection systems: | |||
:#Plastic goggles with side shields; | |||
:#Head, neck and face covering opaque to UV radiation; | |||
:#Soft cotton gloves and. | |||
:#Long-sleeved, tightly woven fabrics with SPF 15 or greater. | |||
====Burn safety==== | |||
UV lamps, depending on the lamp technology, may operate at up to 900°C. The UV lamps and sleeves should be allowed to properly cool down before maintenance to minimize the risk of burns. The electrical equipment (e.g., ballasts) may also become hot during operation and should be evaluated prior to maintenance <ref name="Bolton 2008">Bolton, J.R., Cotton, C.A., 2008. The Ultraviolet Disinfection Handbook. Springer 2008. [https://link.springer.com/book/10.1007%2F978-3-642-01999-9]</ref>. | |||
====Lamp breakage issues and mercury exposure==== | |||
UV lamps pose two safety hazards if broken; the lamps and sleeves are constructed of quartz that, when broken, can pose a risk of serious cuts, and UV lamps contain mercury that can create an inhalation or contact hazard <ref name="Bolton 2008" />. | |||
====UV-C effects on materials==== | |||
UV radiation that is incident upon a surface can be transmitted, reflected or absorbed <ref name="Shamim 2017" />. Absorption of UV causes photodegradation that result in an alteration to the colour, texture or mechanical properties of the materials <ref name="Shamim 2017" />. Materials with high UV absorption indicate greater potential for photodegradation while those with high reflectivity indicate protective effects <ref name="Kowalski 2009" />. All metals do not experience damage under UV exposure <ref name="Kowalski 2009" />. Some of the materials that experience photodegradation are wood, plastic, Polyvinyl chloride (PVC), fabrics, paint and glass <ref name="Kowalski 2009" />. | |||
Because UV-C is absorbed in the ozone layer in the atmosphere and is material exposure is uncommon, published data on degradation by UV-C is minimal<ref name="UV Solutions"> https://uvsolutionsmag.com/articles/2019/uv-degradation-effects-in-materials-an-elementary-overview/ (Accessed 2020 May 12)</ref>. Nonetheless, UV light is linked with possible material degradation; degrade paint, yellow plastics, and destroy air filters. | |||
Metals are almost entirely unaffected by UV, ceramics are completely unaffected by UV exposure but most polymers are susceptible to degradation by UV-C exposure<ref name="UV Solutions" />. The degradation of polymers can in-turn deteriorate the aesthetic properties such as colour and texture and release by-products into the surrounding environment (outgassing) which may raise additional concern on human health. | |||
=== | ===Maintenance and monitoring=== | ||
Proper maintenance and monitoring of UVGI surface disinfection systems ensure continued efficacy. Maintenance tasks and their frequencies are shown in the table below. | |||
{| class="wikitable" | |||
|+Maintenance tasks for UVGI surface disinfection system | |||
{|class = "wikitable" | |||
|+ | |||
|- | |- | ||
!Task!!Frequency!!Action | |||
|- | |- | ||
| | |Check lamp run time values||Monthly||Change lamps if operating hours exceeded design life of 9–10 thousand hours <ref name="Kowalski 2009" /> | ||
|- | |- | ||
| | |Check intensity of UV lamps||Bimonthly||Replace lamps when UVGI dose is equal to or less than the validated UVGI dose after verifying that this condition is caused by low lamp output. | ||
|- | |- | ||
| | |Visually inspect bulbs to ensure all bulbs are operational.||Weekly||If the bulbs show visual dust accumulation, they should be cleaned. Lamps can be wiped clean with a cloth dampened with water or a cleaning agent like dilute alcohol <ref name="Kowalski 2009" /> | ||
|} | |} | ||
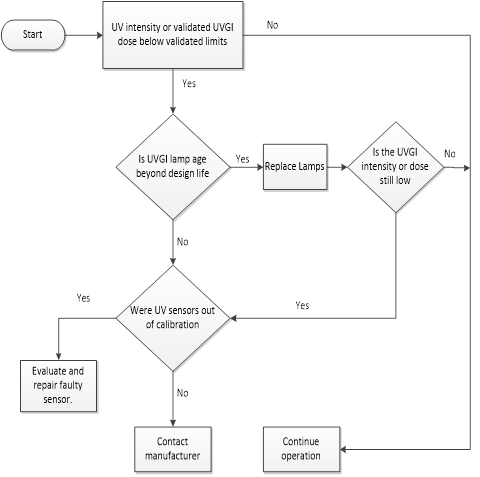
UVGI | The surface UVGI system should be equipped with sensors that automatically monitor UV intensity, validated UV dose and lamps status. A decision chart for UVGI surface disinfection system monitoring is shown below. | ||
===== | [[File:Decision chart for UVGI surface disinfection system monitoring.png|600px|thumb|none|Decision chart for UVGI surface disinfection system monitoring]] | ||
===UVGI lamps disposal=== | |||
LPMV lamp contains mercury which is a toxic heavy metal which cycles through the soil, water and atmosphere in the environment. | |||
Send spent lamps to a mercury recycling facility or back to the manufacturer to prevent personal or environmental exposure. | |||
===Training=== | |||
Operators designated to care for the UVGI systems should receive adequate training in both UV system theory, operation, maintenance and safety. | |||
---- | |||
===Case Studies=== | |||
====Moscow trains==== | |||
In Moscow, Russia, Kostyuchenko, et. al., <ref name="Kostyuchenko 2009" />, investigated the potential of UVGI disinfection on internal surfaces of train carriages and on escalator handrails. They found that the required UV doses for effective disinfection are higher than the theoretically calculated doses.<br> | |||
====Ambulance decontamination <ref name="cite" />==== | |||
====Respiratory Protective Equipment decontamination <ref name="cite" />==== | |||
===Elements of a successful UVGI Disinfection Program=== | |||
====Messaging==== | |||
It is important for messaging around a UVGI Disinfection Program to detail that UVGI can be safe and effective when applied according to a defined and validated protocol<br> | |||
The messaging program should include the following safety aspects: | |||
*UVGI is a form of actinic radiation which does not cause skin cancer | |||
*UVGI/UVC is not the same as UV found in outdoor sunlight | |||
*UVGI can cause reversible skin and eye irritation | |||
*Skin and eye protection should be worn when the possibility of irradiation is present<br> | |||
*UV Lamps should not be used for skin or hand sterilisation | |||
The messaging program should include the following efficacy aspects: | |||
*UVGI is a supplemental surface disinfection technology | |||
*UVGI can be used to kill the new coronavirus as well as a number of other common pathogens | |||
==Sampling and Validation== | |||
{{Expand}} | |||
==Notes and References== | |||
<references /> | |||
[[Category: Infection Prevention and Control]] | |||
[[Category: Decontamination]] | |||
[[Category:Crosscutting Issues]] | |||
Latest revision as of 11:40, 22 February 2021
Decontamination
Decontamination is the process of making an area safe by removing, neutralising or destroying any harmful substances. Decontamination can be achieved by applying physical agents, chemical agents or mechanical removal through any combination of cleaning, disinfection or sterilisation. Physical agents could include heat, radiation and chemical agents include a myriad gasses and liquids.
Cleaning
Cleaning is the process of achieving a state where an area is visually free of contaminating debris. Cleaning is generally achieved by the application of mechanical removal and liquid chemical agents. Cleaning is often an initial decontamination process which removes organic matter from an area. Such organic matter can promote microbial growth and protect microorganisms during further decontamination stages such as disinfection or sterilisation. Cleaning is also frequently applied as the final decontamination stage during which inactivated microorganisms or residual toxins are removed from an area.
Disinfection
Disinfection is the decontamination process of reducing the number of infectious agents to the level where they no longer cause disease. Disinfection typically does not remove bacterial spores.
Sterilisation
Sterilisation is any decontamination process which removes or kills all forms of life in an area. This includes viruses, bacteria, funguses and spores forming organisms.
Surface Decontamination by Cleaning
Before cleaning, a strategy must be available which identifies target organisms, areas, processes, tools and chemical agents appropriate to the area. A review of the high touch areas in the space will inform the strategy. The selection of chemical agents should be based on their intended function (rates of cleaning or disinfection) and the resistance of the target surfaces to potentially corrosive agents. A final cleaning should be done with chemical agents and tools that remove residues from other processes leave no additional unwanted residues.
Surface Decontamination by Heat
Decontamination by heat is typically a sterilisation process with some measure of cleaning beforehand. Surface decontamination by heat is not a common practice and the temperature/time dose function typically requires long exposure times due to the low heat tolerance of surfaces.
Two heat sterilisation processes are available, wet and dry heat.
Wet heat is considered the most dependable method of sterilisation. Steam sterilisers or autoclaves apply heat and humidity under pressure (using saturated steam at 121 °C and 104 kPa) to sterilise laboratory and medical equipment. The application of steam allows for better penetration of heat through permeable insulating layers on any surface than dry heat alone. Autoclaves are occasionally used to sterilise infectious waste.
Dry heat sterilisation is less dependable than wet heat as layers of debris on a surface can insulate organic materials from the process. Dry heat sterilisation is appropriate for impermeable surfaces like glass, but higher temperatures and exposure times are required (160 – 170 °C for periods of 120 to 240 minutes).
Surface Decontamination by Chemicals
Surface Decontamination by Irradiation
Ionising and non-ionising irradiation are both able to decontaminate surfaces. Ionising radiation is not considered generally safe and practical for surface decontamination in a clinical or laboratory setting. Non-ionising radiation such as ultraviolet light in the UV-C band effectively inactivates most microorganisms on surfaces and in the air.
Surface Decontamination by Ultraviolet Germicidal Irradiation
The disinfection effect of ultraviolet light has been described for over 100 years[1]. It is effective against a variety of microorganisms and has been successfully deployed for the purpose of disinfection of water, air and surfaces. Effectiveness depends on a range of variables related to the microorganism of interest, environment and application. Ultraviolet radiation in the UV-C range has been used for its germicidal properties specifically for infection prevention and control - have been demonstrated to work at laboratory scale, in ducts, as upper room irradiation and as portable devices. Safety guidelines have been established (ACGIH)[2].
UVGI surface disinfection has advantages over chemical disinfection because:
- There is no off-gassing of chemicals or residual chemical contamination frequently associated with chemical-based disinfection methods. Therefore, vehicles or spaces can be occupied immediately after UVGI disinfection[3];
- It has high pathogen reduction rates when compared to chemical cleaning; and
- Chemical disinfection methods are time-consuming [4].
A guideline on hospital infection control [5][6] recommends the use of both UVGI and chemical disinfection since UVGI has no penetrating power on dust, dirt and grease, which may harbour microbial contamination. Exposure to UV-C may degrade some materials.
For UVGI surface disinfection for SARC-CoV-2, refer to COVID-19 infection control guidance
The effective band of germicidal ultraviolet (GUV) radiation is between wavelengths of 250-270 nm with 265 nm the optimum efficiency. Ultraviolet Germicidal Irradiation effectively destroys most microorganisms on surfaces. Dirt, dust, and shadows can shield organisms which must be directly exposed to the GUV light. This and safety concerns are limiting factors for its general application.
The application of UVGI for surface disinfection usually involves the use of bare UVGI lamps. Two main approaches to surface disinfection systems are via permanently installed disinfection systems and portable disinfection systems. Permanently installed systems generally consist of bare UVGI lamp fixtures mounted on ceilings or walls. Portable UVGI systems are moved into a place temporarily to decontaminate surfaces [3]. Efficacy is dependent on the intensity of irradiation emitted from the device, proximity of the device to the surface being disinfected and exposure time. The reflectivity of the materials in the vicinity of exposure can increase or decrease efficacy. Shaded items not directly exposed to UV-C irradiation may not effectively be disinfected
UVGI Efficacy
- UVGI dose
The UV-C dose required to achieve a particular pathogen reduction rate is calculated from the single-stage decay equation:
S=e-kD
where:
- S is the Survival fractional [%]
- k is the UVGI rate constant [m2/J]
- D is the UVGI exposure dose [J/m2]
- S is the Survival fractional [%]
The required UVGI dose for a 4 log reduction (99.99% pathogen reduction rate) is calculated by expressing the single-stage decay equation as follows:
ln(S)=-k·D·ln(e) ∴D = (ln (0.0001))/(-k) mJ/cm2 (J/cm2)
UVGI Validation
Validation testing for UVGI surface disinfecting systems is required to ensure that the UV dose for ≥99.99% level of pathogen inactivation is achieved. As the dose rate is a function of the UV sources output and its distance to the target, the manufacturer for non-static UVGI surface disinfecting systems should specify the design minimum distance away from a surface, the UVGI intensity on the surface and the time required to achieve ≥99.99% pathogen reduction.
For disinfection that has either dynamic source or target components, repeatability and confidence studies are required to ensure that the range of variability expected does not exceed acceptable limits for efficacy and safety
UVGI Safety
Studies of personnel practising proper UVGI exposure control measures have shown no harmful effects[5], [6] . Noncompliance with safety precautions can lead to injuries [6]. The following safety issues are associated with the handling of UV equipment.
UV radiation exposure present hazards to the skin and the eyes [3] [7].
UVGI Exposure Guidelines
The ability of UV radiation to penetrate the eyes and skin depends on the wavelength, therefore the UV radiation exposure Threshold Limit Values (TLV) for the eyes and skin published by the American Conference of Governmental Industrial Hygienists (ACGIH) [8] also varies according to the UV wavelength. For UVGI at 254 nm, a cumulative exposure dose greater than 6mJ/cm2 [8] is considered harmful to eyes and skin. Since UVGI surface disinfection systems use bare lamps with dose requirements exceeding 6 mJ/cm2, adherence to PPE is highly recommended to avoid harm.
Eye Safety
The UV wavelength is the determining factor as to which part(s) of the eye may absorb the radiation and suffer biological effects.
The table below shows the absorption of different UV wavelengths by the human eye.
| Wavelength {nm} | Cornea | Aqueous | Lens | Vitreous |
|---|---|---|---|---|
| 100-280 | 100% | 0% | 0% | 0% |
| 300 | 92% | 6% | 2% | 0% |
| 320 | 45% | 16% | 36% | 1% |
| 340 | 37% | 14% | 48% | 1% |
| 360 | 34% | 12% | 52% | 2% |
UVGI (UV wavelengths 200 to 280nm) cumulative exposure dose greater than 6mJ/cm2 [8] can cause temporary corneal injuries (photokeratitis and conjunctivitis [3]). Symptoms of corneal injuries (extreme pain in the eyes) present after 6 -12 hours of exposure and lasts for a few days during which corneal cells will recuperate [3][6].
Skin Safety
Because of poor penetration and absorption capability [5], UVGI cannot penetrate or cause permanent harm to human skin [7]. Some skin irritation or erythema may be experienced but this will generally clear up with proper care.
UV control measures
Administrative controls
Prevent unauthorized personnel from entering the UV radiation area.
Personal protective equipment (PPE)
Personal protective equipment (PPE) protects the wearer from harm due to UV radiation exposure. The following PPE should be worn when operating UVGI surface disinfection systems:
- Plastic goggles with side shields;
- Head, neck and face covering opaque to UV radiation;
- Soft cotton gloves and.
- Long-sleeved, tightly woven fabrics with SPF 15 or greater.
Burn safety
UV lamps, depending on the lamp technology, may operate at up to 900°C. The UV lamps and sleeves should be allowed to properly cool down before maintenance to minimize the risk of burns. The electrical equipment (e.g., ballasts) may also become hot during operation and should be evaluated prior to maintenance [9].
Lamp breakage issues and mercury exposure
UV lamps pose two safety hazards if broken; the lamps and sleeves are constructed of quartz that, when broken, can pose a risk of serious cuts, and UV lamps contain mercury that can create an inhalation or contact hazard [9].
UV-C effects on materials
UV radiation that is incident upon a surface can be transmitted, reflected or absorbed [6]. Absorption of UV causes photodegradation that result in an alteration to the colour, texture or mechanical properties of the materials [6]. Materials with high UV absorption indicate greater potential for photodegradation while those with high reflectivity indicate protective effects [3]. All metals do not experience damage under UV exposure [3]. Some of the materials that experience photodegradation are wood, plastic, Polyvinyl chloride (PVC), fabrics, paint and glass [3].
Because UV-C is absorbed in the ozone layer in the atmosphere and is material exposure is uncommon, published data on degradation by UV-C is minimal[10]. Nonetheless, UV light is linked with possible material degradation; degrade paint, yellow plastics, and destroy air filters. Metals are almost entirely unaffected by UV, ceramics are completely unaffected by UV exposure but most polymers are susceptible to degradation by UV-C exposure[10]. The degradation of polymers can in-turn deteriorate the aesthetic properties such as colour and texture and release by-products into the surrounding environment (outgassing) which may raise additional concern on human health.
Maintenance and monitoring
Proper maintenance and monitoring of UVGI surface disinfection systems ensure continued efficacy. Maintenance tasks and their frequencies are shown in the table below.
| Task | Frequency | Action |
|---|---|---|
| Check lamp run time values | Monthly | Change lamps if operating hours exceeded design life of 9–10 thousand hours [3] |
| Check intensity of UV lamps | Bimonthly | Replace lamps when UVGI dose is equal to or less than the validated UVGI dose after verifying that this condition is caused by low lamp output. |
| Visually inspect bulbs to ensure all bulbs are operational. | Weekly | If the bulbs show visual dust accumulation, they should be cleaned. Lamps can be wiped clean with a cloth dampened with water or a cleaning agent like dilute alcohol [3] |
The surface UVGI system should be equipped with sensors that automatically monitor UV intensity, validated UV dose and lamps status. A decision chart for UVGI surface disinfection system monitoring is shown below.
UVGI lamps disposal
LPMV lamp contains mercury which is a toxic heavy metal which cycles through the soil, water and atmosphere in the environment. Send spent lamps to a mercury recycling facility or back to the manufacturer to prevent personal or environmental exposure.
Training
Operators designated to care for the UVGI systems should receive adequate training in both UV system theory, operation, maintenance and safety.
Case Studies
Moscow trains
In Moscow, Russia, Kostyuchenko, et. al., [4], investigated the potential of UVGI disinfection on internal surfaces of train carriages and on escalator handrails. They found that the required UV doses for effective disinfection are higher than the theoretically calculated doses.
Ambulance decontamination [2]
Respiratory Protective Equipment decontamination [2]
Elements of a successful UVGI Disinfection Program
Messaging
It is important for messaging around a UVGI Disinfection Program to detail that UVGI can be safe and effective when applied according to a defined and validated protocol
The messaging program should include the following safety aspects:
- UVGI is a form of actinic radiation which does not cause skin cancer
- UVGI/UVC is not the same as UV found in outdoor sunlight
- UVGI can cause reversible skin and eye irritation
- Skin and eye protection should be worn when the possibility of irradiation is present
- UV Lamps should not be used for skin or hand sterilisation
The messaging program should include the following efficacy aspects:
- UVGI is a supplemental surface disinfection technology
- UVGI can be used to kill the new coronavirus as well as a number of other common pathogens
Sampling and Validation
Please help to expand this page. |
Notes and References
- ↑ Downes, Arthur; Blunt, Thomas P. (19 December 1878). https://royalsocietypublishing.org/doi/pdf/10.1098/rspl.1878.0109
- ↑ 2.0 2.1 2.2 Citation Needed
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 Wladyslaw Kowalski, 2009. Ultraviolet Germicidal Irradiation Handbook: UVGI for Air and Surface Disinfection. New York. Springer. [1]
- ↑ 4.0 4.1 Sergey Kostyuchenko, Anna Khan, Sergey Volkov, Henk Giller, 2009. UV Disinfection in Moscow Metro Public Transport Systems. IUVA News / Vol. 11 No. 1 [2]
- ↑ 5.0 5.1 5.2 Brown IW Jr et al (1996) Toward further reducing wound infections in cardiac operations. Ann Thorac Surg 62(6):1783–1789.[3]
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Shamim, I. A. ed., 2017. Ultraviolet Light in Human Health, Diseases and Environment. Cham, Switzerland: Springer International Publishing AG.[4]
- ↑ 7.0 7.1 7.2 Myung C. J., 2005. Ultraviolet (UV) Radiation Safety. Environmental Health and Safety University of Nevada Reno. [5]
- ↑ 8.0 8.1 8.2 American Conference of Governmental Industrial Hygienists (ACGIH), 2019. Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. ACGIH: USA [6]
- ↑ 9.0 9.1 Bolton, J.R., Cotton, C.A., 2008. The Ultraviolet Disinfection Handbook. Springer 2008. [7]
- ↑ 10.0 10.1 https://uvsolutionsmag.com/articles/2019/uv-degradation-effects-in-materials-an-elementary-overview/ (Accessed 2020 May 12)