Difference between revisions of "Facilities for Surgical Procedures"
| (33 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{expand}} | {{expand}} | ||
| − | == | + | ==Policy and Service Context== |
===Introduction=== | ===Introduction=== | ||
| Line 9: | Line 9: | ||
===Surgical procedures=== | ===Surgical procedures=== | ||
| − | Medical and surgical procedures are categorised according to their urgency, body system involved, department they are conducted in (e.g. dedicated operating rooms for specialised procedures such as orthopaedic, cardiac surgery, neurosurgery for which different equipment is used), type of procedure, degree of invasiveness and any special instrumentation that may be used (e.g. an endoscopic suite or catheterisation laboratory) | + | Medical and surgical procedures are categorised according to their urgency, body system involved, department they are conducted in (e.g. dedicated operating rooms for specialised procedures such as orthopaedic, cardiac surgery, neurosurgery for which different equipment is used), type of procedure, degree of invasiveness and any special instrumentation that may be used (e.g. an endoscopic suite or catheterisation laboratory). |
Surgical procedures are performed by a surgical team in a dedicated operating room and may be: | Surgical procedures are performed by a surgical team in a dedicated operating room and may be: | ||
| Line 39: | Line 39: | ||
*CSSD staff. | *CSSD staff. | ||
| − | ===Patient care=== | + | ===Patient care<ref name="G.McDonald and D Sheard">G.McDonald and D Sheard “ A Practical Guide to Decontamination in Healthcare”</ref>=== |
The surgical team has the responsibility of caring for the patient during the perioperative period, which includes the pre-, intra- and post-operative management of the patient - i.e. care given to the patient before, during and after surgery. | The surgical team has the responsibility of caring for the patient during the perioperative period, which includes the pre-, intra- and post-operative management of the patient - i.e. care given to the patient before, during and after surgery. | ||
| Line 46: | Line 46: | ||
*Post-operative care is the management of the patient after the procedure until discharge and includes care in the recovery area in the operating theatre unit and the inpatient facility. | *Post-operative care is the management of the patient after the procedure until discharge and includes care in the recovery area in the operating theatre unit and the inpatient facility. | ||
| − | ===Surgical disciplines<ref name=" | + | ===Surgical disciplines<ref name="G.McDonald and D Sheard" />=== |
<u>The most common surgical disciplines include:</u> | <u>The most common surgical disciplines include:</u> | ||
| Line 66: | Line 66: | ||
*Orthopaedic surgery - this involves surgical treatment related to the musculoskeletal system. | *Orthopaedic surgery - this involves surgical treatment related to the musculoskeletal system. | ||
| − | ===Surgical techniques<ref name=" | + | ===Surgical techniques<ref name="G.McDonald and D Sheard" />=== |
<u>These include the following:</u> | <u>These include the following:</u> | ||
| Line 94: | Line 94: | ||
===Hospital categories of service=== | ===Hospital categories of service=== | ||
| − | The business case and the health brief define the correct package of service and the operating theatre number per facility based on the [http://www.health.gov.za/index.php/2014-03-17-09-09-38/legislation/joomla-split-menu/category/84-2012r?download=138:regulations-relating-to-categories-of-hospitals-r185-2012 Provincial Strategic Transformation Plan and the government policy document: Government Notice - R.185, 2nd March 2012, National Health Act 61/2003] | + | The business case and the health brief define the correct package of service and the operating theatre number per facility based on the [http://www.health.gov.za/index.php/2014-03-17-09-09-38/legislation/joomla-split-menu/category/84-2012r?download=138:regulations-relating-to-categories-of-hospitals-r185-2012 Provincial Strategic Transformation Plan and the government policy document: Government Notice - R.185, 2nd March 2012, National Health Act 61/2003]. |
{| class="wikitable" | {| class="wikitable" | ||
|+{{Anchor|Surgical facilities per facility category}}Surgical facilities per facility category | |+{{Anchor|Surgical facilities per facility category}}Surgical facilities per facility category | ||
| Line 148: | Line 148: | ||
'''1 OT per 25 surgical beds.''' | '''1 OT per 25 surgical beds.''' | ||
| − | The '''[https://apps.who.int/iris/handle/10665/39548 WHO Planning & Design Guide]''' | + | The '''[https://apps.who.int/iris/handle/10665/39548 WHO Planning & Design Guide]''' proposes the following calculation method: |
Multiply no of surgical beds (160) by no of operating days/year (260) | Multiply no of surgical beds (160) by no of operating days/year (260) | ||
| Line 187: | Line 187: | ||
e.g. <math display="inline">E = 20 * 75% = 15 </math> theatres | e.g. <math display="inline">E = 20 * 75% = 15 </math> theatres | ||
| − | Refer to: 2004 HBN 26-Vol 1 Surgical procedures: Appendix 3 – Capacity Planning | + | Refer to: 2004 HBN 26-Vol 1 Surgical procedures: Appendix 3 – Capacity Planning |
<br /> | <br /> | ||
| Line 265: | Line 265: | ||
*the cleaning and disinfection of the physical space. | *the cleaning and disinfection of the physical space. | ||
| − | “A clean operating room environment with sterile (or correctly decontaminated) equipment with restricted access and appropriately attired staff can go a long way to reducing the risks of surgical site infections" | + | “A clean operating room environment with sterile (or correctly decontaminated) equipment with restricted access and appropriately attired staff can go a long way to reducing the risks of surgical site infections" |
| − | ====Healing environments | + | ====Healing environments==== |
Historically, operating theatre units have concentrated on designs that address only the technical aspects and the need for an uncontaminated, sterile or clean environment, with slim regard for the need to make patient and staff spaces pleasant and appealing. Today, a number of patients undergo surgery without a general anaesthetic, remaining conscious throughout the procedure. It is therefore important that the environment created within the OTU is soothing and encourages a healing environment. Design of the OTU environment needs to consider the needs of the theatre staff, potentially traumatised patients, guardians of minors and care for minors themselves. The evidence-based considerations and recommendations are discussed below. | Historically, operating theatre units have concentrated on designs that address only the technical aspects and the need for an uncontaminated, sterile or clean environment, with slim regard for the need to make patient and staff spaces pleasant and appealing. Today, a number of patients undergo surgery without a general anaesthetic, remaining conscious throughout the procedure. It is therefore important that the environment created within the OTU is soothing and encourages a healing environment. Design of the OTU environment needs to consider the needs of the theatre staff, potentially traumatised patients, guardians of minors and care for minors themselves. The evidence-based considerations and recommendations are discussed below. | ||
| Line 357: | Line 357: | ||
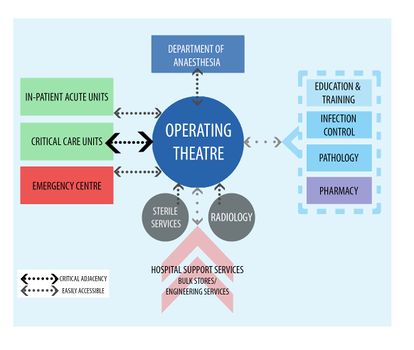
*controlled access from an external corridor is highly desirable. | *controlled access from an external corridor is highly desirable. | ||
| − | [[File:Departmental relationships and critical adjacencies.jpg|alt=Departmental relationships and critical adjacencies|none|thumb| | + | [[File:Departmental relationships and critical adjacencies.jpg|alt=Departmental relationships and critical adjacencies|none|thumb|414x414px|Departmental relationships and critical adjacencies]] |
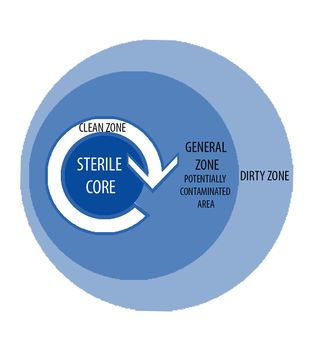
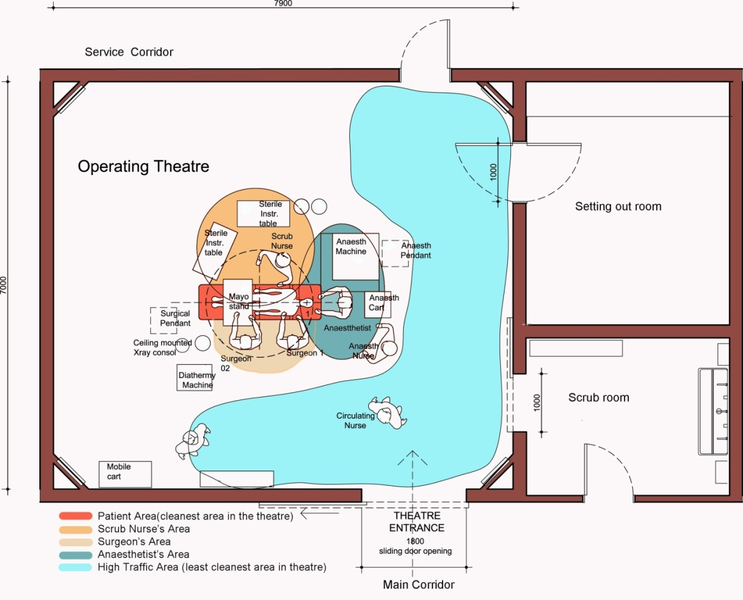
===Sterile Core Principle=== | ===Sterile Core Principle=== | ||
| Line 412: | Line 412: | ||
|} | |} | ||
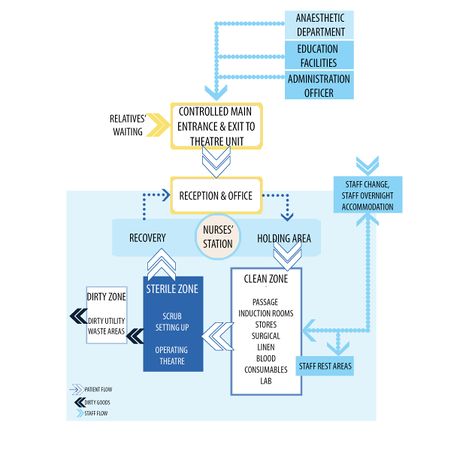
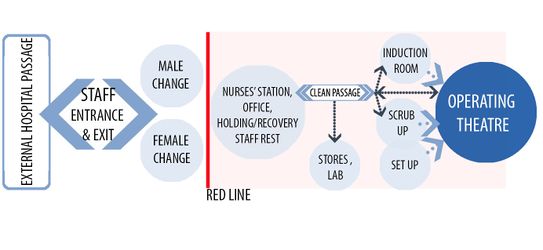
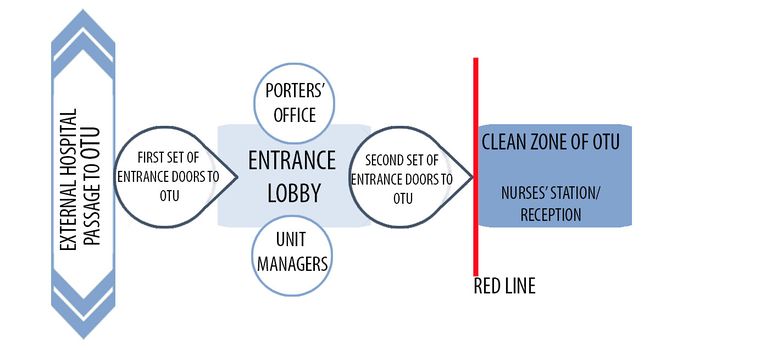
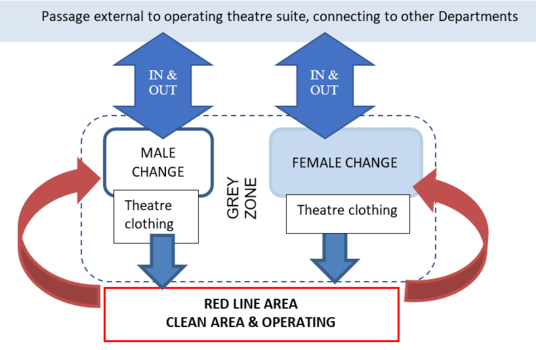
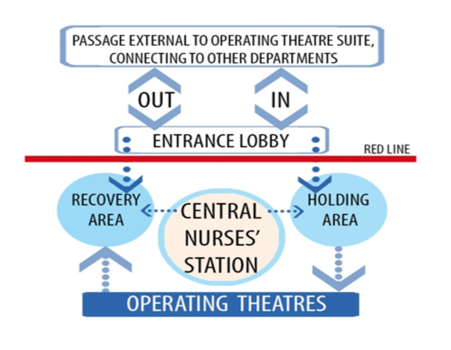
[[File:Relationships within the Operating Theatre Unit.jpg|alt=Relationships within the Operating Theatre Unit|none|thumb|466x466px|Relationships within the Operating Theatre Unit (OTU)]] | [[File:Relationships within the Operating Theatre Unit.jpg|alt=Relationships within the Operating Theatre Unit|none|thumb|466x466px|Relationships within the Operating Theatre Unit (OTU)]] | ||
| − | |||
| − | |||
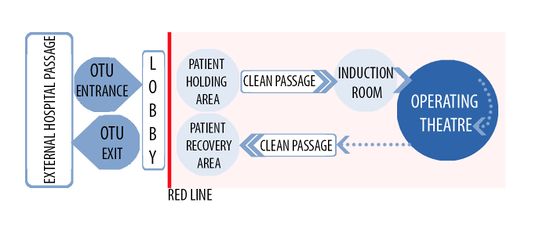
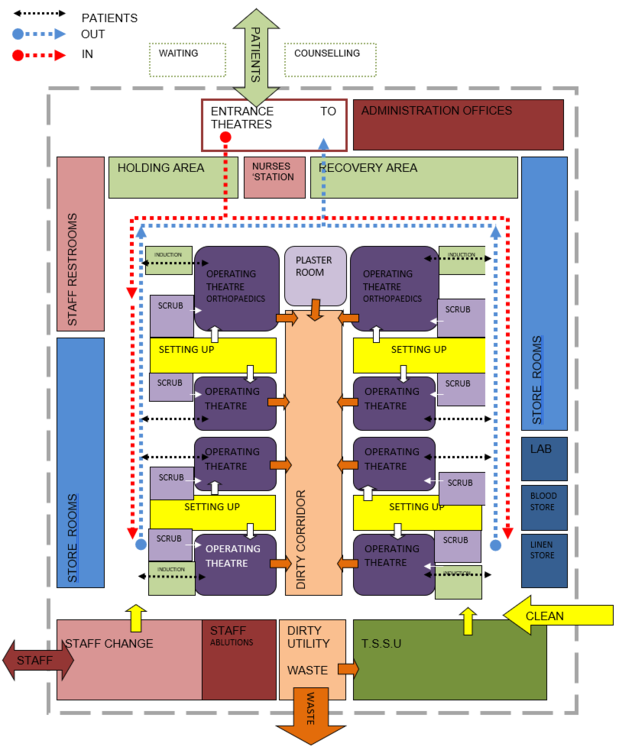
===Traffic Flow Paths=== | ===Traffic Flow Paths=== | ||
The OTU design must prevent cross-traffic of staff and supplies from the decontaminated/soiled areas to the sterile/clean areas. The use of facilities external to the operating theatre for soiled/decontaminated processing, clean assembly and sterile processing must be designed to move the flow of goods and personnel without compromising universal precautions or aseptic techniques in both departments. | The OTU design must prevent cross-traffic of staff and supplies from the decontaminated/soiled areas to the sterile/clean areas. The use of facilities external to the operating theatre for soiled/decontaminated processing, clean assembly and sterile processing must be designed to move the flow of goods and personnel without compromising universal precautions or aseptic techniques in both departments. | ||
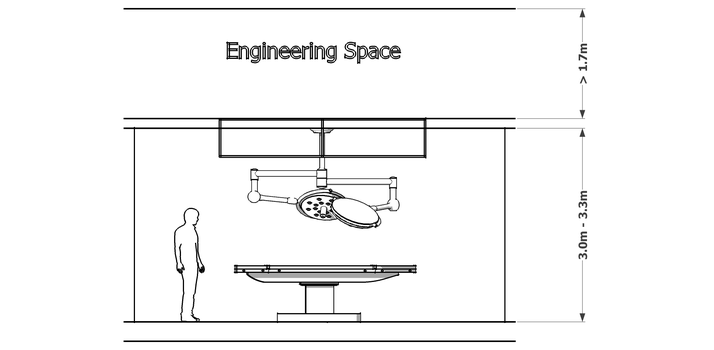
| Line 884: | Line 882: | ||
*Minimum wall length -3,45m | *Minimum wall length -3,45m | ||
| − | ''The recommended distance to the recovery area is a maximum of 65m from the operating theatres to a stage-1 recovery bay. This distance equates to a minute of travel time for the patient from the operating room to recovery, and is considered the maximum time a patient can be off fixed monitoring post-surgery'' | + | ''The recommended distance to the recovery area is a maximum of 65m from the operating theatres to a stage-1 recovery bay. This distance equates to a minute of travel time for the patient from the operating room to recovery, and is considered the maximum time a patient can be off fixed monitoring post-surgery'' |
<u>Services include:</u> | <u>Services include:</u> | ||
| Line 944: | Line 942: | ||
====Anaesthetic induction room (optional)==== | ====Anaesthetic induction room (optional)==== | ||
| − | <blockquote>''"The provision of anaesthetic rooms immediately adjacent to the operating room has also become a source of controversy. In many European hospitals the provision of the anaesthetic room has been removed in favour of holding areas. This is in response to the modern-day provision of better-equipped day-surgery suites, which have removed many of the minor procedural and short theatre-time cases from the inpatient theatre suite. The anaesthetic room therefore is no longer required as a holding area and, if the premedication can be delivered at ward level, the dwell time outside the operating room can be completed elsewhere. In a patient-focused environment, however, the anaesthetic room provides a soothing environment where carers can wait with the frail elderly or the very young and provide comfort right up to the point of intubation."''<ref name=" | + | <blockquote>''"The provision of anaesthetic rooms immediately adjacent to the operating room has also become a source of controversy. In many European hospitals the provision of the anaesthetic room has been removed in favour of holding areas. This is in response to the modern-day provision of better-equipped day-surgery suites, which have removed many of the minor procedural and short theatre-time cases from the inpatient theatre suite. The anaesthetic room therefore is no longer required as a holding area and, if the premedication can be delivered at ward level, the dwell time outside the operating room can be completed elsewhere. In a patient-focused environment, however, the anaesthetic room provides a soothing environment where carers can wait with the frail elderly or the very young and provide comfort right up to the point of intubation."''<ref name="Ron Bridgefoot">Ron Bridgefoot Principal of HASSELL</ref></blockquote>The provision of anaesthetic rooms (induction rooms) immediately adjacent to the operating room depends on the facility and procedure type. |
The anaesthetic induction room is for holding patients on mobile beds or trolleys prior to operative procedures at times when the operating theatre is not available. Local, regional or general anaesthetics can be administered in this area. | The anaesthetic induction room is for holding patients on mobile beds or trolleys prior to operative procedures at times when the operating theatre is not available. Local, regional or general anaesthetics can be administered in this area. | ||
| Line 1,054: | Line 1,052: | ||
</gallery> | </gallery> | ||
| − | ==== Anaesthetic workroom ==== | + | ====Anaesthetic workroom==== |
An Anaesthetic workroom may be provided for cleaning, testing and storing of anaesthesia equipment and should be located with direct access to circulation corridors and ready access to the operating theatres. | An Anaesthetic workroom may be provided for cleaning, testing and storing of anaesthesia equipment and should be located with direct access to circulation corridors and ready access to the operating theatres. | ||
| − | Services include: | + | <u>Services include:</u> |
| − | + | *Sufficient power and data outlets and a medical gas panel for testing of equipment. | |
| + | *A clinical hand-wash basin shall be provided within the room. | ||
| + | *Stainless steel wash trough with hand shower. | ||
| + | *Hands-free clinical wash hand basin. | ||
| − | + | <u>Considerations:</u> | |
| − | + | *The anaesthetic workroom shall contain workbenches, sink(s) and racks for cylinders. | |
| + | *Provisions shall be made for separate storage of clean and soiled items. | ||
| + | *Work top area – stainless steel. | ||
| + | *Provide space for anaesthetic trolleys and other anaesthesia equipment. | ||
| − | - | + | ====Scope cleaning====<ref name="HBN 26">Facilities for surgical procedures in acute general hospitals (HBN 26)[https://www.gov.uk/government/publications/facilities-guidance-for-surgical-procedures-in-acute-general-hospitals]</ref> |
| + | This space is utilised for the cleaning, disinfection, sterilisation and storage of endoscopes and accessories. | ||
| − | + | The area is divided internally into a dirty area for the cleaning of used equipment and a clean area for the storage of cleaned, reprocessed equipment. | |
| − | - | + | It is good practice for scope-cleaning and sterilisation to be performed in the CSSD and not in the OTU. |
| − | - | + | <u>The dirty-area requirements include:</u>[[File:Scope cleaning room in operating theatre suite (Courtesy of Red Cross Hospital).png|thumb|401x401px|Scope cleaning room in operating theatre suite (Courtesy of Red Cross Hospital)]] |
| − | - | + | *The dirty area to be equipped with automated endoscope re-processors, with the required electrical supply and three water supplies – hot, cold and demineralised water. |
| − | - | + | *A deep-bowl stainless steel sink that is large enough to rinse and wash the endoscopes. |
| + | *A stainless steel work surface to be provided. | ||
| + | *Storage cupboards for special chemicals required (these are hazardous and must be handled and stored accordingly). | ||
| + | *Suction. | ||
| + | *Clinical hand-wash basin with elbow taps, soap dispenser and hand-towel dispenser with disposal bin mounted on the wall. | ||
| + | *Signage to be mounted in a clearly visible spot, warning of any hazardous substances and processes and detailing procedures in the event of contamination. | ||
| + | *Extract ventilation at bench level is required to remove toxic vapours. | ||
| − | + | <u>The clean area requirements include:</u> | |
| − | + | *Storage of personal protective equipment such as nitrate gloves, goggles, impermeable aprons and respiratory-protection equipment suitable for use when decontaminating endoscopes or mixing chemicals. | |
| − | The | + | ===Sterile Zone=== |
| + | [[File:Relationship diagram - sterile zone.png|alt=Relationship diagram - sterile zone|thumb|477x477px|'''Relationship diagram - sterile zone''']] | ||
| + | <u>The sterile zone comprises:</u> | ||
| − | + | *The scrub-up/gowning room | |
| + | *The set-up room | ||
| + | *The operating theatre (OT). | ||
| − | + | These rooms are directly adjacent to each other. | |
| − | + | ====Scrub-up/gowning room==== | |
| + | Each theatre should have a scrub room. The scrub-up/gowning room provides an enclosed, dedicated area for pre-operative scrubbing, gowning and gloving prior to entering the operating theatre. It is required that all entering the operating theatre should wear surgical scrubs and surgical masks | ||
| − | + | The scrub-up/gowning room should be a minimum of 11m² per operating room (to allow sufficient space for a minimum of three people). The scrub room should be large enough to allow staff to scrub up, gown and circulate without risk of contaminating each other or contamination from the surrounding fittings. | |
| − | + | The scrub area should be situated off the clean passage, in a separate room adjacent to, and in front of, the theatre entrance - i.e. the scrub-up area should be directly accessible from the OTU corridor and from the associated operating or procedure room. | |
| + | [[File:Scrub area example 1.jpg|thumb|Scrub area example 1]] | ||
| + | [[File:Scrub area example 2.jpg|alt=Scrub area example 2|thumb|Scrub area example 2]] | ||
| + | <u>Services include:</u> | ||
| − | + | *The scrub area to be equipped with a double stainless steel scrub sink with elbow taps. | |
| + | *Splash-limiting stainless steel basins or drainage trough. | ||
| + | *Hot and cold water. | ||
| + | *Wall-mounted clock. | ||
| − | + | <u>Considerations:</u> | |
| − | + | *The activities of scrubbing and gowning/gloving should be separate within the space. | |
| + | *Taps should be non-touch – automatically operated or foot operated. | ||
| + | *Taps should be high enough so that hands and elbows can be washed and rinsed under the taps. | ||
| + | *Taps must be able to be operated with elbow action. | ||
| + | *Provide shelves for replacement gowns, gloves, head cover and foot covers. | ||
| + | *Provide adequate space to gown. | ||
| + | *Antiseptic hand-washing liquid dispensers should be fixed to the wall above the scrub sinks. These should be elbow-action dispensers. | ||
| + | *The scrub sink and taps should be at a height that facilitates hand- and arm-washing. | ||
| + | *The design of the drainage must ensure that the floor does not become wet during scrub-up procedures. | ||
| + | *The floors must be anti-slip. | ||
| + | *Wall-mounted paper towels to be provided. | ||
| + | *Wall-mounted glove dispensers to be provided. | ||
| + | *Space for floor disposal bins that are foot-operated. | ||
| + | *The door between the scrub and theatre should be an automatic self-closing door (however, a door is not essential between the theatre and the scrub room unless the scrub is shared between two theatres). | ||
| + | *Splash-back to the sink to be a solid waterproof panel. | ||
| − | + | [[File:Scrub area in clean corridor.jpg|alt=Scrub area in clean corridor|none|thumb|{{Anchor|Scrub area in clean corridor}}Scrub area in clean corridor|466x466px]] | |
| + | [[Facilities for Surgical Procedures#Scrub area in clean corridor|<u>The example image above</u>]] shows an installation where the scrub area is included in the common-use theatre passage. While this appears to be an appealing and economical design, it presents a potential infection-control risk. The common-use passage is not normally served by the same class of ventilation, does not enjoy the same hygienic finishes as the theatre, and is not validated as an aseptic area. This arrangement also removes the clean transition zone between common-use areas and the aseptic theatre environment. Staff are forced to enter and leave the theatre through the main theatre door during surgical cases, thus disrupting the aseptic environment established in theatre while in operation. | ||
| − | + | ====Set up/Setting out/Preparation==== | |
| + | The set-up room is the clean workroom in the OTU where clean or sterile materials are held and arranged prior to use in the operating theatres. Instrument packs and other sterile packs required for the day surgery are delivered to the set-up room from CSSD. Here the scrub nurse will set up for a procedure, before the full surgical team are present, opening sterile items and instrument packs on trolleys to check that all the required equipment is present and sterile. | ||
| − | + | Each theatre should have a set-up room which is outside but adjacent to the operating theatre, and which has direct access to the operating theatre. Sharing of one set-up room between two operating theatres is acceptable, provided the layout and size of the room facilitates such sharing. | |
| − | + | Set-up rooms may be combined with the sterile stock store with direct access to the operating theatre. | |
| − | + | A minimum of 12m² per operating room (or 20m² where one set-up room is shared between two operating rooms) should be provided. Larger set-up rooms are required for operating rooms where organ-transplant surgery and orthopaedic surgery take place (more trolleys are required to be set up prior to operating). | |
| − | + | <u>The main functions for which facilities shall be provided are:</u> | |
| − | + | *Setting up of instruments and packs on trolleys prior to a procedure. | |
| + | *Storage of sterile packs, instruments and materials to be used in the operating theatre. | ||
| + | *Holding of sterile supplies and packs. | ||
| + | *Storage of lotions in a special-purpose warming cabinet. | ||
| + | *Preparation of dressing and instrument trolleys. | ||
| + | *Storage of drugs, including scheduled drugs. | ||
| − | + | <u>Considerations:</u> | |
| − | . | + | *This is a sterile area and should not be accessed by people not in full theatre attire. |
| + | *Space is required for assembly of trolleys prior to delivery to the operating room. | ||
| + | *The set-up room shall be positively pressured relative to adjoining rooms. | ||
| + | *Any worktop areas should be stainless steel. | ||
| + | *Doors into the theatre must be automated. | ||
| + | *Storage and suitable work surfaces. | ||
| + | *Doors in and out of the set-up room must be large enough to allow instrument trolleys fully set out to pass through without being contaminated. | ||
| + | *Work surfaces to be high enough to store 870mm-high trolleys beneath. | ||
| − | + | ====Operating Theatres (Sterile Zone)==== | |
| + | The operating theatre (OT) is central to the operating-theatre unit. | ||
| − | The | + | =====Essential principles of design for operating theatres===== |
| + | The OT is a specialised facility within the hospital where lifesaving or life-improving procedures are carried out on the human body by invasive or minimally invasive methods under strict aseptic conditions in a controlled environment, by specially trained personnel, to promote healing and cure with maximum safety, comfort and economy. It is imperative that OTs are designed scientifically to ensure sterility, easy maintenance and effective utilisation | ||
| − | + | All aspects of the theatre must be focused on maintaining the concentration of the operating surgeon and team during the operation. | |
| − | + | The standardisation of theatre layouts within an OTU will offer great value to the performance and efficiency of the theatre staff. Mirroring theatre layouts in order to economise on space usage is therefore not recommended. | |
| − | + | =====Infection prevention and control within the theatre===== | |
| + | This section serves to outline a few critical aspects of infection prevention and control as they pertain to surgery facilities. For a more detailed review of IPC measures and practices, the reader is urged to refer to the IUSS Health Facility Guide: Infection Prevention and Control. | ||
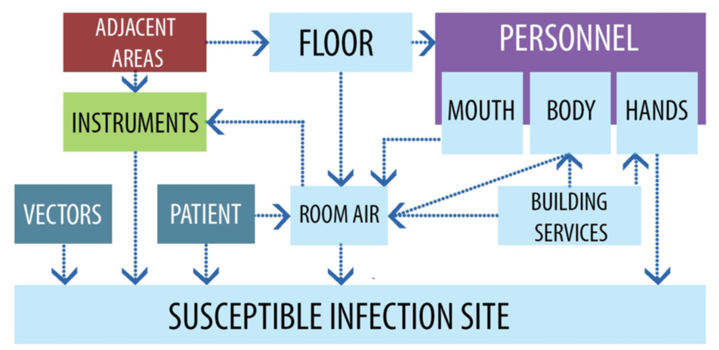
| + | [[File:Routes for surgical site infection in the OT.png|alt=Routes for surgical site infection in the OT|thumb|719x719px|Routes for surgical site infection in the OT]] | ||
| + | <u>The following direct contact routes for surgical-site infection are identified as:</u> | ||
| − | These | + | *'''Instruments''' |
| + | **Surgical Instruments are at risk of being contaminated prior to or during procedures by both contact and airborne routes. These contaminated instruments are considered to be a primary source of contact infection. | ||
| − | + | *'''Consumables''' | |
| + | **Consumables are similarly at risk of becoming themselves contaminated, before being the agent by which contact contamination occurs. | ||
| + | *'''Utilities''' | ||
| + | **Utilities which are re-usable between procedures, and which may even be shared during simultaneous procedures, can harbour or transmit infection. | ||
| − | + | *'''Fixed room and equipment surfaces''' | |
| + | **These surfaces shall be able to withstand the rigors of the regular cleaning and disinfection regimen prior to each invasive procedure. | ||
| − | + | *'''Theatre staff''' | |
| + | **Theatre staff are a major source of infectious particles and for this reason theatre practice, gowning and etiquette is of critical importance in reducing incidences of surgical-site infections. | ||
| − | + | <u>Airborne contamination can have the following sources:</u> | |
| − | + | *'''Theatre staff''' | |
| + | **It is estimated that a person walking can liberate as many as 5 000 bacteria per minute (Kowalski & Bahnfleth, 1998). Many of these particles can remain suspended in the air currents for extended periods and therefore have a great potential for surgical-site infection. | ||
| + | *'''Ventilation systems''' | ||
| + | **Inadequately designed or maintained ventilation systems can harbour, generate, liberate and distribute airborne contaminants widely. Well-designed ventilation systems can suppress, control and dilute airborne contaminants. | ||
| + | *'''Environmental''' | ||
| + | **Airborne environmental contaminants are generally kept out of the surgery facility by the ventilation system. Where ventilation systems fail or are inadequate, viable and non-viable contaminants can enter the surgery facility and contaminate staff, equipment and the wound site directly. | ||
| + | *'''Surgical-site infections''' | ||
| + | **Surgical-site infections result in a higher healthcare burden. It is estimated that surgical-site infections (SSI) double the cost of treatment through length of stay (LOS) alone. This estimate excludes re-admissions | ||
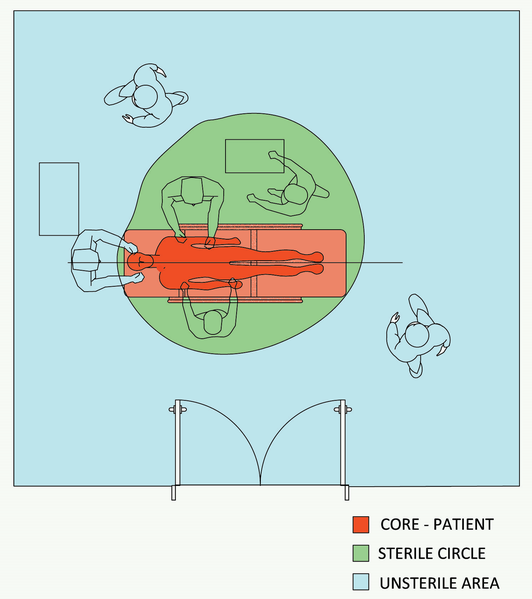
| − | + | =====Space separation and differentiation within the operating theatre:<ref name="G.McDonald and D Sheard" />===== | |
| + | Surgical procedures pose a risk of infection to the patient, necessitating that the space to perform these procedures be carefully planned accordingly. These procedures should occur in areas which must provide adequate space to accommodate the patient, the surgical team while performing the procedure, and the equipment required for the procedure. The set-up of an operating theatre is primarily influenced by the aseptic principles that have to be applied. | ||
| − | + | <u>In order to maintain good aseptic principles it is essential to divide the areas in and around the operating theatre into three working areas:</u> | |
| − | + | *The core or centre of the operating theatre/room is where the patient is situated and where the procedure is performed. | |
| − | + | *The “sterile” circle is the area directly around the patient where the scrub nurses and surgeon(s) performing the procedure, using sterile instruments, stand and work. It includes any theatre staff directly involved in the procedure who are wearing sterile surgical attire, the operating table, other accessory equipment and any furniture that is covered with sterile drapes, such as trolleys and stands. | |
| − | + | *The unsterile area is where associated support staff (i.e. the anaesthetist, circulating nurse and students, etc.) are performing their duties within the operating theatre. While assisting “sterile” personnel, unsterile personnel must remain in the unsterile area and avoid crossing into or between sterile areas. They supply items to the scrub team attending the patient, move equipment around the theatre into place and monitor patient progress. | |
| − | + | Generally, equipment, trolleys and members of the surgical team are on either side of the table, while the anaesthetic team and anaesthesia equipment is at the head of the table. | |
| + | <gallery mode="packed" heights="400px" caption="Space separation and differentiation within the operating theatre"> | ||
| + | File:Working areas within the operating theatre.png|alt=Working areas within the operating theatre|'''Working areas within the operating theatre''' | ||
| + | File:Zones within the operating theatre.png|'''Zones within the operating theatre''' | ||
| + | </gallery> | ||
| + | The equipment, supplies and people working within the immediate surgical field around the patient on the operating table (a 4m x4m envelope) are the area of greatest concern for infection control in the surgical environment. A carefully orchestrated workflow in, out of and within the operating theatre, is key to minimising the risk of contamination in this cleanest of patient-care environments. Anything that moves in and out of operating rooms, as well as the surgical suite as a whole, should be subject to rigorous control. | ||
| + | =====Size and space allocation in operating theatres===== | ||
| + | [[File:Anaesthetist trolley in theatre.png|alt=Anaesthetist trolley in theatre|thumb|300x300px|Anaesthetist trolley in theatre]] | ||
| − | + | *The shape of the room should be rectangular and as close to square as possible. | |
| − | + | *The shorter side of the room should be a minimum of 80% of the longer side. | |
| + | *The room should have splayed corners for ease of cleaning. The ventilation return/extraction duct is commonly placed behind the splayed corner. | ||
| + | *Space allocation must be large enough for correct techniques and small enough to minimise unnecessary movements of personnel, patients and supplies. | ||
| + | *The speed of the development of technology has had, and will have in future, significant implications for the design of OTs. “The challenge for planners and architects is to design surgical facilities that are not only functional but have sufficient flexibility to adapt to the changes and rapid developments in surgical technology“ <ref name="HBN 26" /> | ||
| + | *Size is very dependent on the equipment to be utilised within the OT. Anaesthetic machines, for example, have increased in size due to the number and complexity of the integral patient-monitoring systems. | ||
| − | - | + | ====Operating theatre sizes==== |
| + | {| class="wikitable" | ||
| + | | '''THEATRE''' | ||
| + | |'''AREA''' | ||
| + | |'''COMMENT''' | ||
| + | |- | ||
| + | |'''Minor procedure''' | ||
| + | |'''20- 36 m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''General surgery''' | ||
| + | |'''40 m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''Ophthalmology''' | ||
| + | |'''40 m²''' | ||
| + | |May need to accommodate a ceiling fixed or mobile microscope. | ||
| + | |- | ||
| + | |'''Burns''' | ||
| + | |'''40 m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''Cath lab''' | ||
| + | |'''49m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''Digital theatre''' | ||
| + | |'''49 m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''ENT and scopes''' | ||
| + | |'''49 m²''' | ||
| + | |May need to accommodate a ceiling-fixed or mobile microscope | ||
| + | |- | ||
| + | |'''General endoscopy''' | ||
| + | |'''55 m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''Urology & plastics''' | ||
| + | |'''55 m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''Cardiothoracic''' | ||
| + | |'''55 m²''' | ||
| + | |May have to accommodate extra equipment like the heart-lung machine. | ||
| + | |- | ||
| + | |'''Orthopaedic''' | ||
| + | |'''60 m²''' | ||
| + | |Needs to accommodate x-ray image intensifier, different tables - e.g. fracture tables | ||
| + | |- | ||
| + | |'''Trauma''' | ||
| + | |'''49 m²''' | ||
| + | | | ||
| + | |- | ||
| + | |'''Neurosurgery & spinal''' | ||
| + | |'''60 m²''' | ||
| + | |May need to accommodate a ceiling-fixed or mobile microscope. | ||
| + | |} | ||
| + | The provision of multipurpose operating rooms can be considered to give flexibility in booking cases to any operating room. This generally means operating rooms of around 55m² to cater for a variety of equipment that now accompanies many of the general procedures. | ||
| − | + | <u>Advantages of a standard theatre size include the following:</u><ref name="HBN 26" /> | |
| − | + | *Flexibility, as a variety of surgical procedures can be performed in the same size of theatre, which leads to better utilisation of the theatre and less downtime. | |
| + | *Both minimal and open surgery can be undertaken in the same theatre space. | ||
| + | *Orthopaedic surgery requires as many as seven trolleys for different sets of instruments during surgery, and requires a larger space to accommodate the additional items. | ||
| + | *In a number of facilities, patients are transferred from the theatre table to their beds. Beds are larger than the traditional trolleys and require more space to manoeuvre within the operating theatre. | ||
| − | + | =====Finishes and fixtures===== | |
| − | - | + | ======Ceilings====== |
| + | Ceilings in the operating theatres should be smooth and monolithic. The surface finish must be washable and completely sealed. While a solid concrete slab is preferred, with services directly above the slab, this is not always possible - which results in a suspended ceiling with a ceiling void above. This requires access panels to be fitted to the ceiling and should be the sealable type. The ceiling void must be deep enough to allow maintenance to be carried out on equipment above the ceiling. | ||
| − | + | While acoustically absorbent ceiling finishes reduce noise, it is essential that infection risks are minimised and only smooth, easily washable surface finishes are applied to the ceiling soffit. | |
| − | + | ======Walls====== | |
| + | Walls in the operating theatre must be smooth, impervious, durable, washable and easily cleanable. Added protection needs to be applied in areas where damage to the surface of the wall is more likely. | ||
| − | + | ======Floors====== | |
| + | <u>Floors in the operating theatre have to be particularly hardwearing and durable, as they are subject to:</u> | ||
| − | - | + | *machinery loads as equipment is pushed back and forth throughout the unit and stored or utilised in the theatres; |
| + | *Frequent washing and scrubbing, as cleanliness is critical and decontaminating the theatres after each operation is critical for infection-control purposes; and | ||
| + | *spillages, which occur during most operations; consequently floor finishes must be easily washable, stain-resistant and sustainable. | ||
| − | + | <u>It is therefore important that floors finishes are:</u> | |
| − | - | + | *Slip-resistant |
| + | *Continuous with sealed joints at junctions | ||
| + | *Smooth | ||
| + | *Impervious | ||
| + | *Easily washable | ||
| + | *Wear resistant | ||
| + | *Hygienic. | ||
| − | + | Skirtings should be coved and should rise 100mm up the wall. Best practice is to have a continuous floor finish that continues up the wall with no joint between the floor and the skirting. This allows for easy cleaning and discourages microbial colonisation. | |
| − | + | The fixing of the floor finish to the underlying screed must be carefully carried out to the manufacturer’s specification to ensure good adhesion and so that the floor will withstand the heavy loads anticipated. | |
| − | + | Where the theatre is under “''laminar flow''”, the floor directly below the airflow hood should be a different colour, so that staff can differentiate the area covered by the hood within which the sterile trolleys must be kept, and where key staff should remain during the operation. | |
| − | + | It is useful to also demarcate with different colours floor areas where essential equipment needs to be always placed - e.g. the emergency trolley. | |
| − | + | ======Doors and door frames====== | |
| + | Doors and frames need to be durable and able to withstand frequent impact from mobile equipment. Solid-core doors must be used. | ||
| − | + | Where glazed panels are fitted to the theatre doors, these should be opaque to protect patient privacy. | |
| − | + | Automatic door openers that are foot- or elbow-operated should be fitted to the entrance doors to the theatre. | |
| − | + | Since the main entrance to theatres isn’t through an anteroom, the operation of this door during operations can severely affect the integrity of the clean zone established in the theatre. While the presence of sliding doors in theatres presents a concealed mechanism which is virtually un-cleanable, and does not provide an adequate seal to assist with contamination control, swing doors also present a plethora of additional problems. The surge of air from swinging doors in theatres could disrupt the ultra-clean zone around the operating table, and the use of swinging doors in theatres with unidirectional airflow (UDAF) or laminar flow should be applied with caution. Sliding doors, when used, should be installed such that the door mechanism is not within the operating-theatre room. | |
| − | + | ======Windows====== | |
| + | Windows in the OTU should be weather-tight, durable, washable, and easily accessible for cleaning and maintenance. | ||
| − | + | Windows should have blinds installed which enable the OTU to be darkened as appropriate. These must be washable and easily maintained and of a material that does not encourage microbial colonisation. The positioning of windows is critical within the OTU, and should prevent glare, ensure maximum user comfort, provide views out while protecting internal privacy. See paragraph 5.4.3 “Views” for more information. | |
| − | + | ======Music====== | |
| + | Many theatre staff insist on music in theatres. For this reason it is advisable to install a CD player or AV receiver in the theatre panel, or at a similar discreet location. Where music players are permanently installed in theatres, their controls should be flush with the panel. AV receivers should not be limited to propriety hardware interfaces, but should accept multiple device types. A suitable consideration would be a wireless Bluetooth receiver supporting easy pairing with universal remote audio and volume controls. This would permit staff to bring their own portable media players and playlists for use with the system. | ||
| − | + | ======Lighting====== | |
| + | Good lighting levels and quality are essential in operating theatres. In addition to irradiance, colour rendering and evenness are important factors. For details of lighting requirements for surgeries the reader is referred to [[Building Engineering Services|building engineering services]] | ||
| − | + | ======Computer equipment====== | |
| + | Digital display of imaging results should be available to the surgeon at the operating table. For this purpose a display panel should be provided on a movable or retractable pendant. The inclusion of a conventional keyboard and mouse is not recommended. Should the imaging display system require a user interface, a de-contaminable touch interface is recommended. | ||
| + | [[File:Swab Count Board.png|alt=Swab Count Board|thumb|300x300px|[http://medicalinnovations.co.za/wp-content/uploads/2013/07/59-00-00.jpg Swab Count Board]]] | ||
| − | - | + | ======Swab-count board====== |
| + | Theatre policy requires safe checking and counting of swabs, needles and instruments before, periodically during, and after each case. This process requires the use of containers for used or contaminated swabs, and a count board and swabs will remain in the theatre throughout the case. | ||
| − | - | + | For this reason, a swab-count board should be accommodated in the theatre-layout planning. The swab-count board could include the stand with bins and racks to facilitate the counting and control of swabs and instruments. |
| − | - | + | ======Theatre warning light====== |
| + | A visual alarm panel should be included in the theatre. This panel should give an indication of any critical engineering system failure, such as ventilation or medical gases. Alarms to this panel should also be relayed to the nurses’ station and engineering office. Non-critical alarms should be relayed only to the engineering office and nurses’ station as necessary. The theatre alarm panel should also give a visual indication of the theatre temperature. For information the reader is referred to the [[Building Engineering Services|Building engineering services]] | ||
| − | + | ====Theatre types==== | |
| − | - | + | ====='''The general-surgery operating theatre'''===== |
| + | This operating theatre provides an aseptic environment in which to carry out surgical procedures under local, regional, general anaesthetic or sedation. | ||
| − | - | + | *The general-surgery operating theatre is located within the operating unit and away from through-traffic. |
| + | *Direct access is required to the holding bay/anaesthetic room, scrub room, exit bay/circulation corridor. | ||
| + | *Ready access is required to recovery, clean-up areas, sterilising bay, sterile store and CSSD. | ||
| − | + | ======Staff Contingent And Locations====== | |
| + | The surgeon normally stands on the patient’s right-hand side if it is open surgery; however, in the case of laparoscopic surgery the position varies. The surgeon may stand at the foot end of the table. | ||
| − | + | The scrub person stands opposite the surgeon, with the assistant surgeon. | |
| − | + | The anaesthetist and assistant will be at the head of the theatre table. | |
| − | + | The circulating person will be at any area that makes it easy to work in close proximity to the scrub team. | |
| − | - | + | ======Overhead Services====== |
| + | Overhead services should include one central ceiling-mounted, dual-luminaire theatre light that should be securely fixed above the operating table. | ||
| − | + | Also, two services pendants, one for surgical and one for anaesthetic use, are to be securely fixed to the ceiling. These pendants shall be positioned such that they are readily accessible to either the surgeon or the anaesthetist, as appropriate. Retractable pendants shall be designed such that they accommodate the ergonomics of even the most diminutive nursing staff. | |
| − | + | {| class="wikitable" | |
| − | - | + | |'''''General theatre services''''' |
| − | + | |'''''Anaesthetic pendant''''' | |
| − | - | + | |'''''Surgical pendant''''' |
| − | + | |- | |
| − | - | + | |'''230V socket outlets and connection to the UPS systems''' |
| + | |6 | ||
| + | |6 | ||
| + | |- | ||
| + | |'''Oxygen''' | ||
| + | |2 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''Medical vacuum points''' | ||
| + | |2 | ||
| + | |2 | ||
| + | |- | ||
| + | |'''Low-pressure medical air''' | ||
| + | |1 | ||
| + | |1 | ||
| + | |- | ||
| + | |'''Nitrous oxide''' | ||
| + | |1 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''Anaesthetic gas-scavenging points''' | ||
| + | |1 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''High-pressure medical air''' | ||
| + | |<nowiki>-</nowiki> | ||
| + | |2 | ||
| + | |} | ||
| − | + | ======Wall-Mounted Services====== | |
| + | <u>A wall-mounted control panel is commonly provided and should include the following services:</u> | ||
| − | The | + | *Radio or AV receiver |
| + | *Clock and stop-clock | ||
| + | *Telephone | ||
| + | *Sterile touch-screen-controlled computer | ||
| + | *Temperature controller | ||
| + | *The control panel could have a conventional x-ray viewing box or a 42” LCD screen (this may be on a fixture suspended from the ceiling. | ||
| − | + | A swab board shall be mounted on one wall. | |
| − | + | An indicator light is required outside the entrance of the theatre to indicate whether the theatre is occupied. | |
| − | + | It is essential that at least one wall be free from door openings and services that require frequent attention. This provides a quiet area for sterile equipment and scrubbed personnel, which is not compromised by frequent traffic. It is preferable for the adjacent wall to be free, or impinged upon only for exit from the operating room. | |
| − | The | + | ======Anaesthetic Equipment====== |
| + | <u>The following anaesthetic equipment should be accommodated:</u> | ||
| − | + | *Anaesthetic machine, with cardiac monitor | |
| + | *Two or three drip stands | ||
| + | *Equipment positioning for endoscopic surgery | ||
| + | *Trolley with the anaesthetic-induction and -reversal drugs | ||
| + | *Trolley for the anaesthetist to work on | ||
| + | *Suction apparatus - may or may not be part of anaesthetic machine | ||
| + | *Records / computer to record patient data | ||
| + | *Waste-sharps container | ||
| + | *Chair. | ||
| − | + | ======Surgical Equipment====== | |
| + | <u>The following surgical equipment should be accommodated:</u> | ||
| + | *Digital display and recording system for patient’s records | ||
| + | *Two infusion pumps | ||
| + | *Three syringe pumps | ||
| + | *Blood warmer | ||
| + | *Feeding pump | ||
| + | *Operating table | ||
| + | *Suction apparatus | ||
| + | *Two kick-abouts | ||
| + | *Three to four instrument trolleys | ||
| + | *Three basin stands | ||
| + | *Mayo stand or table | ||
| + | *Diathermy machine | ||
| + | *Two small trolleys | ||
| + | *1 for the catheter | ||
| + | *1 for the telescope warmer | ||
| + | *Two endoscopy carts with the camera system, video, light source and insufflators | ||
| + | *Equipment monitors for specialised equipment | ||
| + | *Writing worktop, with drawers for nursing staff | ||
| + | *Four chairs | ||
| + | *Sharps container | ||
| + | *Emergency call system. | ||
| − | + | ======<u>Additional Considerations</u>====== | |
| − | The | + | *The scrub area and setting-up area may be shared by two adjacent theatres. |
| + | *The use of automatic, foot-operated, sliding doors for all theatre entrances is recommended. | ||
| + | *Passive infrared proximity sensors are not appropriate for activating theatre doors. | ||
| + | *An emergency call button linked to the sister’s office should be accessible from within the theatres. | ||
| + | *All theatre electrical services should be on emergency backup supply. This includes a UPS and generator. | ||
| − | + | ====='''The Obstetrics Operating Theatre'''===== | |
| + | This theatre is principally the same as a general theatre, save for the wall panel which includes services for two new-borns. | ||
| − | + | <u>This should include two separate sets in the panel, each with:</u> | |
| − | + | *Oxygen | |
| + | *Vacuum | ||
| + | *Medical air | ||
| + | *Six plugs. | ||
| − | + | Two baby-resuscitation stations are to be located permanently adjacent to the theatre’s wall service panel. | |
| − | + | ====='''The Orthopaedics Operating Theatre: – Ultraclean / Laminar-flow'''===== | |
| + | This theatre is principally the same as a general theatre, but orthopaedic units generally have a higher demand for space for personnel, storage and set up. | ||
| − | + | '''Personnel Required In the Theatre''' | |
| − | + | *Surgeon | |
| + | *One or two assistant surgeons | ||
| + | *Scrub person - can be one or sometimes two | ||
| + | *The circulating person | ||
| + | *Anaesthetist | ||
| + | *Anaesthetic nurse or assistant | ||
| + | *Possible additions: | ||
| + | **students | ||
| + | **medical reps | ||
| − | + | The surgeon normally stands on the patient’s left-hand side or, depending on the type of surgery he will be doing, in another position. If it is surgery of the extremities, he will stand on the side to be operated on. | |
| − | + | The assistant surgeon stands opposite the surgeon, next to the scrub person. | |
| − | + | The circulating person is at the bottom and side of the table, and looks after the scrub team. | |
| − | + | The scrub person stands opposite the surgeon, with the assistant surgeon. | |
| − | + | The anaesthetist and assistant will be at the head of the theatre table. | |
| − | + | '''Overhead Services''' | |
| − | + | Overhead services should include one central ceiling-mounted, dual-luminaire theatre light that should be securely fixed above the operating table. | |
| − | + | Also, two services pendants, one for surgical and one for anaesthetic use, are to be securely fixed to the ceiling. These pendants shall be positioned such that they are readily accessible to either the surgeon or the anaesthetist, as appropriate. Retractable pendants shall be designed such that they accommodate the ergonomics of even the most diminutive nursing staff. | |
| − | + | {| class="wikitable" | |
| − | + | |'''''General theatre services''''' | |
| + | |'''''Anaesthetic pendant''''' | ||
| + | |'''''Surgical pendant''''' | ||
| + | |- | ||
| + | |'''230V socket outlets and connection to the UPS systems''' | ||
| + | |6 | ||
| + | |8 | ||
| + | |- | ||
| + | |'''Oxygen''' | ||
| + | |2 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''Medical vacuum points''' | ||
| + | |2 | ||
| + | |2 | ||
| + | |- | ||
| + | |'''Low-pressure medical air''' | ||
| + | |1 | ||
| + | |1 | ||
| + | |- | ||
| + | |'''Nitrous oxide''' | ||
| + | |1 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''Anaesthetic-gas scavenging points''' | ||
| + | |1 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''High-pressure medical air''' | ||
| + | |<nowiki>-</nowiki> | ||
| + | |2 | ||
| + | |} | ||
| + | Anaesthetic, wall-mounted and surgical equipment accommodation considerations are principally the same as for general theatres. | ||
| − | + | '''Unidirectional Airflow/ Laminar-Flow Plenums''' | |
| − | + | *The plenum shall be fitted to the ceiling in the middle of the theatre. | |
| + | *All metal work on the laminar flow unit shall be stainless steel or baked epoxy-coated mild steel. | ||
| + | *HEPA filters shall be terminally mounted at the unidirectional-airflow (UDAF) plenum. | ||
| + | *The UDAF screen shall be hinged such that the lighting and HEPA filters are serviceable from within the theatre. | ||
| + | *HEPA filters shall be removable into the theatre for testing and replacement. This protects the theatre from being directly exposed to the service-space environment during HEPA filter changes. | ||
| + | *The UDAF plenum shall include sealable upstream sampling ports for in situ filter-efficiency testing. | ||
| + | *The UDAF plenum shall include concealed lighting to achieve the required background lighting levels and quality. | ||
| − | + | ======Equipment====== | |
| + | The equipment required in an orthopaedic theatre is similar to that of a general theatre, although the equipment trolleys are larger and more numerous to accommodate the specialist equipment. There may be as many as seven equipment trolleys for certain procedures. | ||
| − | + | ======Additional Considerations====== | |
| + | The “Plaster of Paris” or POP store room should be adjacent to the theatre and should include a stainless steel sink with hot and cold water and storage space for materials. | ||
| − | + | =====The cardiothoracic operating theatre===== | |
| + | This theatre is principally the same as a general theatre, with the following considerations: | ||
| − | In | + | '''Personnel Required In the Theatre''' |
| − | + | *Surgeon | |
| + | *One or two assistant surgeons | ||
| + | *One or two scrub persons | ||
| + | *One or two anaesthetists | ||
| + | *One or two anaesthetic assistants or nurses | ||
| + | *One circulating person | ||
| + | *Perfusionist. | ||
| − | + | The surgeon stands on the patient’s right-hand side during the procedure. | |
| − | + | The assistant stands opposite the surgeon. | |
| − | + | If there are two assistants, the other one will stand on the surgeon’s side, opposite the scrub person. | |
| − | + | The scrub person stands next to the assistant surgeon, opposite the surgeon. | |
| + | The anaesthetist is always at the top end of the operating table. | ||
| − | + | The anaesthetic nurse or assistant will be in close proximity to the anaesthetist at all times. | |
| + | The perfusionist sits behind the surgeon, next to the heart-lung machine. | ||
| − | The | + | ======Overhead Services====== |
| + | The overhead services required are similar to that of a general theatre. | ||
| − | + | '''Anaesthetic Equipment''' | |
| − | + | The following anaesthetic equipment should be accommodated: | |
| − | + | *Anaesthetic machine, with cardiac monitor | |
| + | *Two or three drip stands | ||
| + | *Small trolley for insertion of lines like the CVP, arterial line (ideal in induction room) | ||
| + | *Trolley with the anaesthetic induction and reversal drugs | ||
| + | *Trolley for the anaesthetist to work on | ||
| + | *Suction apparatus-may or may not be part of anaesthetic machine | ||
| + | *Records / computer to record patient data | ||
| + | *Monitors | ||
| + | *Infusion pumps | ||
| + | *Waste-sharps container | ||
| + | *Chair. | ||
| − | + | '''Surgical Equipment''' | |
| − | + | The following surgical equipment should be accommodated: | |
| − | + | *Operating table | |
| − | + | *Three to four surgical instrument trolleys | |
| + | *Small trolleys for insertion of a urinary catheter | ||
| + | *Basin stands - two or three | ||
| + | *Two kick-abouts | ||
| + | *Mayo stand or table | ||
| + | *Suction apparatus | ||
| + | *Three basin stands | ||
| + | *Mayo stand or table | ||
| + | *Diathermy machine | ||
| + | *Two small trolleys | ||
| + | **1 for the catheter | ||
| + | **1 for the telescope warmer | ||
| − | + | *Defibrillator machine | |
| + | *Drip stand with sternal saw motor | ||
| + | *Special operating table which can be adjusted to any position needed | ||
| + | *More than one suction apparatus | ||
| + | *Four chairs | ||
| + | *Sharps container | ||
| + | *Emergency call system. | ||
| + | ======Perfusionist Equipment====== | ||
| + | The following perfusionist equipment should be accommodated: | ||
| − | + | *Heart-lung machine | |
| + | *Heater/cooler machine | ||
| + | *Intra-aortic balloon pump | ||
| + | *Arterial blood gas machine | ||
| + | *Ice machine (outside OR) | ||
| − | + | The heat load of the perfusionist’s equipment (heart-lung machine, inter alia) must be considered. | |
| − | + | ====='''The Neurosurgery Operating Theatre'''===== | |
| + | This theatre is principally the same as a general theatre, save for the following considerations: | ||
| − | + | '''Personnel Required in the Theatre''' | |
| − | + | *Surgeon | |
| + | *One or two assistant surgeons | ||
| + | *One scrub person | ||
| + | *One anaesthetist | ||
| + | *One anaesthetic assistant or nurse | ||
| + | *One circulating person. | ||
| − | + | The surgeon and assistant stand at the head of the table. | |
| − | + | The anaesthetist and anaesthetic machine will be at the side or at the foot end of the table. | |
| − | + | The scrub person stands either between the surgeon and assistant, or on the right-hand side of the patient. | |
| − | + | The circulating person is next to the sterile team, at the head end of the table. | |
| − | + | The anaesthetic nurse or assistant will be in close proximity to the anaesthetist. | |
| − | + | ======Overhead Services====== | |
| + | Overhead services should include one central ceiling-mounted, dual-luminaire theatre light that should be securely fixed above the operating table. | ||
| − | + | Also, two services pendants, one for surgical and one for anaesthetic use, are to be securely fixed to the ceiling. These pendants shall be positioned such that they are readily accessible to either the surgeon or the anaesthetist, as appropriate. Retractable pendants shall be designed such that they accommodate the ergonomics of even the most diminutive nursing staff. | |
| + | {| class="wikitable" | ||
| + | |'''''General theatre services''''' | ||
| + | |'''''Anaesthetic pendant''''' | ||
| + | |'''''Surgical pendant''''' | ||
| + | |- | ||
| + | |'''230V socket outlets and connection to the UPS systems''' | ||
| + | |6 | ||
| + | |8 | ||
| + | |- | ||
| + | |'''Oxygen''' | ||
| + | |2 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''Medical vacuum points''' | ||
| + | |2 | ||
| + | |2 | ||
| + | |- | ||
| + | |'''Low-pressure medical air''' | ||
| + | |1 | ||
| + | |1 | ||
| + | |- | ||
| + | |'''Nitrous oxide''' | ||
| + | |1 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''Anaesthetic-gas scavenging points''' | ||
| + | |1 | ||
| + | |<nowiki>-</nowiki> | ||
| + | |- | ||
| + | |'''High-pressure medical air''' | ||
| + | |<nowiki>-</nowiki> | ||
| + | |2 | ||
| + | |} | ||
| + | Consider that since the surgeon is at the head of the patient and the anaesthetist moves to the side of the patient, the anaesthetic pendant should be located to the side (side of the patient’s head). | ||
| − | + | ======Wall-Mounted Services====== | |
| + | The wall-mounted services required for this type of theatre are principally the same as for a general theatre. | ||
| − | + | ======Anaesthetic Equipment====== | |
| + | The aesthetic equipment space requirements are principally the same as for a general theatre. | ||
| − | + | ======Surgical Equipment====== | |
| + | The following surgical equipment should be accommodated: | ||
| − | + | *Operating table | |
| + | *Two or three surgical instrument trolleys | ||
| + | *Suction apparatus | ||
| + | *Two or three basin stands | ||
| + | *Small trolley with shaving equipment | ||
| + | *Small trolley for inserting the urinary catheter | ||
| + | *Mayo stand or table | ||
| + | *Operating microscope | ||
| + | *Ultrasonic surgical aspirator-for tumours | ||
| + | *Head rests like the Mayfield and the horseshoe | ||
| + | *Special operating table that can be adjusted to suit the particular procedure | ||
| + | *Two suction machines or apparatus | ||
| + | *Diathermy machine with both bipolar and monopolar settings. | ||
| − | The | + | ======Additional Considerations====== |
| + | The surgical equipment utilised in this type of theatre can be highly sensitive to vibration. The theatre should therefore be appropriately isolated from vibration. Refer to the equipment installation requirements for acceptable limits. | ||
| − | + | ====='''The Ophthalmology Theatre'''===== | |
| + | This theatre is principally the same as a general theatre, save for the following considerations: | ||
| − | + | ======Staffing Requirements====== | |
| + | Consider that the surgeon is at the head and the anaesthetist moves to the side of the patient; therefore the anaesthetic pendant is to the side (side of patient’s head). | ||
| − | + | ======Overhead Services====== | |
| + | This theatre requires ceiling-mounted scopes. This demands that the ceiling structure be sufficiently supported to carry the additional load. | ||
| − | + | ======Additional Considerations====== | |
| + | The surgical equipment utilised in this type of theatre can be highly sensitive to vibration. The theatre should therefore be appropriately isolated from vibration. Refer to the equipment installation requirements for acceptable limits. | ||
| − | + | The following additional features need to be accommodated in the setting-up room: | |
| − | + | *Washing and cleaning area for instruments. | |
| + | *Storage space. | ||
| + | *Flash sterilisers are often requested for emergency sterilising of dropped utensils. This solution is not recommended, as these can create an additional maintenance and operational burden and risk. In addition, the responsibility of equipment sterilisation then shifts away from the CSSD to the theatre staff. It is recommended that the capacity for emergency sterilising is incorporated into the CSSD to ensure proper sterilisation processes are followed. The implementation of flash sterilisers as a convenience to supplant good operational planning is therefore not acceptable. | ||
| − | + | ====='''The Urology Theatre'''===== | |
| + | This theatre is principally the same as a general theatre, save for the following considerations: | ||
| − | + | ======Additional Considerations====== | |
| + | The surgical equipment utilised in this type of theatre can be highly sensitive to vibration. The theatre should therefore be appropriately isolated from vibration. Refer to the equipment installation requirements for acceptable limits. | ||
| − | + | Urology theatres usually function as a set of two theatres in tandem: | |
| − | + | *The first theatre is a standard theatre. | |
| + | *The adjacent theatre is used for imaging, and has a scope and x-ray table with x-ray – therefore it needs a water supply and drain to the table. | ||
| + | *The imaging room may require lead-lined doors for radiation protection. The hinges or sliding mechanism and closers of these doors should be designed to reliably manage the additional weight of these doors. | ||
| − | + | Where separate imaging rooms are not implemented and integrated imaging bays are used instead, the theatre architecture should incorporate ionising radiation-protective measures. | |
| − | + | ====='''The Bronchoscopy Theatre'''===== | |
| + | This theatre is principally the same as a general theatre, save for the following considerations: | ||
| − | + | A scope-cleaning room is required near or attached to the theatre. This is detailed further on in this document. | |
| − | + | *Flash autoclaves are often requested but are not recommended, as these can create an additional maintenance and operational burden. In addition, the responsibility of equipment sterilisation then shifts away from the CSSD to the theatre staff. | |
| − | + | *A clean, ventilated storage cupboard is required for the drying and storing of scopes. | |
| − | + | Since bronchoscopy theatres present a very high risk for airborne infection, these theatres should be maintained at a relative negative pressure with high ventilation rates. Recirculation ventilation is not recommended for these theatres; instead full fresh-air exhausted ventilation systems are recommended with special consideration for the control of contaminated exhaust discharge. The three elements of control are direction, dilution, and disinfection. | |
| − | + | ====='''The Paediatric Operating Theatre'''===== | |
| − | + | *This theatre is principally the same as a general theatre, save for the following considerations: | |
| + | *Consideration should be given to creating a warm welcoming environment for paediatric theatres. | ||
| + | *Waiting areas should be provided for mothers and family. | ||
| + | *OT tables shall not be fixed. | ||
| + | *Independent temperature control is required to reduce the risk of mortality in paediatric care. | ||
| + | **The temperature range for paediatric theatres and induction rooms should be between 18°C and 28°C. | ||
| − | + | ======Context Consideration====== | |
| − | + | *Paediatric theatre caseloads will vary from institution to institution and may be as high as 20-25%. | |
| + | *Paediatric theatre cases treated within district hospitals should be limited to children over four years of age or 10kg. | ||
| − | + | ====='''The Burns Theatre'''===== | |
| + | This theatre is principally the same as a general theatre, save for the following considerations: | ||
| − | + | *The operating table should facilitate waste-water management during patient washing. | |
| + | *Floor drains are not recommended within theatres as these can present a conduit for cross-infection between procedures and theatres. | ||
| + | *Two hoses should be available for patient wash. | ||
| + | *Temperature range = 22-28°C. | ||
| + | *Humidity range = 45-60% RH. | ||
| + | *Temperature and humidity display is required at the theatre control panel. | ||
| − | + | ====='''Digital Operating Theatres'''===== | |
| + | Most modern theatres can be termed digital theatres as they now use digital imagery during surgery. An effective implementation of digital technology in theatres requires consideration of the following questions in planning: | ||
| − | + | *Which surgical team member needs to see what, and at what stage? | |
| + | *Where are the images being recorded from, and where do they get recorded to? | ||
| + | *Is imaging equipment constantly used in the theatre for procedures? | ||
| + | **If not, then mobile units could be considered. | ||
| + | **Fixed or ceiling-mounted equipment could become an obstruction if it is not continuously utilised in the theatre in question. | ||
| − | + | ===='''Day-surgery unit'''==== | |
| + | <blockquote>"Day-surgery units are defined as “self-contained, dedicated units, suitable for carrying out surgical procedures and treatments on adult and child patients whose discharge is planned for the same day as their admission"<ref>NHS Scotland, SHPN52 Accommodation for Day Care, 2002 </ref> </blockquote>Day-care services mainly include day surgery, endoscopy, and medical investigation and treatment. Provision of a large theatre size is preferable to accommodate a variety of surgical procedures. The infrastructural requirements for a day-surgery unit theatre are principally the same as that of a general theatre. | ||
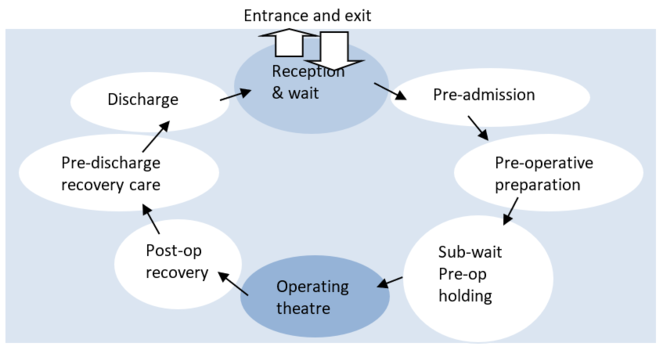
| + | [[File:One-way patient flow through day unit.png|alt=One-way patient flow through day unit|thumb|663x663px|One-way patient flow through day unit]] | ||
| − | + | =====Planning considerations===== | |
| + | Design of the facility should accommodate the sequence outlined below, such that the patient progresses in one direction through the unit. Principal routes should be designed to minimise clashes between patients and services. | ||
| − | + | Patient-related activities occur in the following sequence: | |
| − | + | *entering the unit | |
| + | *reception and waiting | ||
| + | *pre-admission and assessment | ||
| + | *pre-operative preparation | ||
| + | *operation/procedure | ||
| + | *post-anaesthesia recovery | ||
| + | *pre-discharge recovery and care | ||
| + | *discharge and exit of the unit | ||
| + | *transfer to a larger theatre to accommodate scopes.. | ||
| − | + | Privacy is essential. Men and women should be attended to in separate areas, and children must be kept separate from adult patients. Continuous observation by the nursing staff is crucial. | |
| − | + | =====Location===== | |
| + | Day-theatre units should preferably be close to the OPD or adjacent to the theatres where the day theatre can share services with the main theatre unit. | ||
| − | + | =====Accommodation Requirements:===== | |
| − | + | {| class="wikitable" | |
| − | + | |+{{Anchor|Day-surgery Unit: Accommodation requirements}}Day-surgery Unit: Accommodation Requirements | |
| − | + | |'''Room''' | |
| − | + | |'''Standard''' | |
| − | + | |'''Non-standard''' | |
| − | + | |'''Comments''' | |
| − | + | |'''Location''' | |
| − | + | |- | |
| − | + | | colspan="5" |'''Entrance to day unit''' | |
| − | + | |- | |
| − | + | |Entrance | |
| − | + | | | |
| − | + | |x | |
| − | + | | rowspan="3" |Refer to Item 9.1 | |
| − | + | | rowspan="3" |Entrance | |
| − | + | |- | |
| − | + | |Waiting area with play area | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Reception | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | | colspan="5" |'''Pre-operative area''' | |
| − | + | |- | |
| − | + | |Pre-admission assessment room | |
| − | + | | | |
| − | + | |x | |
| − | + | |Consulting room configuration | |
| − | + | |Adjacent to waiting area | |
| − | + | |- | |
| − | + | |Change rooms for male patients | |
| − | + | | | |
| − | + | |x | |
| − | + | | rowspan="5" |Change room area | |
| − | + | | rowspan="2" |Adjacent to assessment room | |
| − | + | |- | |
| − | + | |Change rooms for female patients | |
| − | + | | | |
| − | + | |X | |
| − | + | |- | |
| − | + | |Patient locker area | |
| − | + | | | |
| − | + | |x | |
| − | + | | rowspan="4" |Adjacent to change areas | |
| − | + | |- | |
| − | + | |Male patient toilets and shower | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Female patient toilet and shower | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Admissions room | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Nurses’ station | |
| − | + | |x | |
| − | + | | | |
| − | + | |Focal point within the pre-operative area | |
| − | + | |Adjacent to patient changing rooms, admissions rooms and patient sub-waiting areas. | |
| − | + | |- | |
| − | + | | colspan="5" |'''Operating Theatre suite''' | |
| − | + | |- | |
| − | + | |Pre-operative nurses base | |
| − | + | |x | |
| − | + | | | |
| − | + | | rowspan="2" |Pre-operative area in theatre | |
| − | + | | rowspan="19" |Theatre area which may be separate to the main theatre block or attached to the main theatre block in the hospital. This should also be adjacent to the day ward area - pre- and post-op. | |
| − | + | |- | |
| − | + | |Pre-operative holding area | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Anaesthesia room | |
| − | + | | | |
| − | + | |x | |
| − | + | | rowspan="4" |Theatre unit (''refer to IUSS document re operating theatres'') | |
| − | + | |- | |
| − | + | |Scrub-up and gowning | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Operating room | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Set-up room | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Mobile x-ray equipment bay | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Post-operative recovery room | |
| − | + | | | |
| − | + | |x | |
| − | + | | rowspan="2" |Post-operative area | |
| − | + | |- | |
| − | + | |Post-operative nurses’ station | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Sluice room | |
| − | + | |x | |
| − | + | | | |
| − | + | | rowspan="10" |Support services off theatre passage | |
| − | + | |- | |
| − | + | |Scope cleaning room | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| + | |Equipment store | ||
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | |Dirty utility | ||
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | |Surgical store | ||
| + | | | ||
| + | |x | ||
| + | |- | ||
| + | |Medicine cupboard | ||
| + | | | ||
| + | |x | ||
| + | |- | ||
| + | |Equipment service room | ||
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | |Medical gas cylinder store | ||
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | |Wheelchair/trolley park bays | ||
| + | | | ||
| + | |x | ||
| + | |- | ||
| + | |Anaesthetic-gas scavenging | ||
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | | colspan="5" |'''Post-operative recovery area''' | ||
| + | |- | ||
| + | |Pre-discharge recovery area - trolleys | ||
| + | | | ||
| + | | | ||
| + | | | ||
| + | | rowspan="2" |Adjacent to the nurses’ station | ||
| + | |- | ||
| + | |Pre-discharge recovery area - chairs | ||
| + | | | ||
| + | | | ||
| + | | | ||
| + | |- | ||
| + | |Pre-discharge recovery area – nurses’ base | ||
| + | |x | ||
| + | | | ||
| + | | | ||
| + | | rowspan="3" |Adjacent to | ||
| − | + | pre-discharge recovery area | |
| − | + | |- | |
| − | + | |Patient toilet (to accommodate a patient in a wheelchair) | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Clean utility | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | | colspan="5" |'''Shared support areas''' | |
| − | + | |- | |
| − | + | |Dirty utility | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | | rowspan="9" |Located between pre-op, post-operative recovery and pre-discharge areas | |
| − | + | |- | |
| − | + | |Sluice | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Cleaners’ room | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Sterile pack store | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Equipment store | |
| − | - | + | |x |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Clean linen store | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |*Or central store | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Crutches and splint store | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Switch room | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | | colspan="5" |'''Staff facilities''' | |
| − | + | |- | |
| − | + | |Staff change for theatre - female | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | | rowspan="7" |A separate staff area closely situated to the theatres | |
| − | + | |- | |
| − | + | |Staff change for theatre - male | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Staff toilet female | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Staff toilet male | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Staff locker area | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Staff room | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Seminar room | |
| − | + | |x | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | | colspan="5" |'''Administration''' | |
| − | + | |- | |
| − | + | |Unit manager’s office | |
| − | + | |x | |
| − | - | + | | |
| − | + | | | |
| − | + | | rowspan="2" |Adjacent to the theatres | |
| − | + | |- | |
| − | + | |Sister’s office | |
| − | + | |x | |
| − | + | | | |
| + | | | ||
| + | |} | ||
| − | + | ====IT Requirements==== | |
| + | It is important that the design team understand the intra-dependencies of all the services within the OTU early during the design process. This includes collating and analysing the extensive information regarding the following equipment and services: | ||
| − | + | *medical gases | |
| + | *oxygen and air | ||
| + | *suction | ||
| + | *data cables and data equipment | ||
| + | *surgical equipment. | ||
| − | + | [[File:Digital imaging in theatre.png|thumb|Digital imaging in theatre]] | |
| + | These interdependencies will inform the IT requirements that need to be planned for. This is especially relevant in theatres where ready access to diagnostic imagery is used to assist in, and assess, procedural progress. | ||
| − | + | The incorporation of real-time imaging provided by MRI or CT-scanning during neurosurgical, cardiovascular or orthopaedic surgery demands larger operating rooms. In many tertiary hospitals specialised operating rooms of 65-80m2 are in evidence. | |
| − | + | Imaging equipment capable of performing 3D rotational angiography, CT-scanning and intravascular ultrasound enable open surgery and endovascular techniques to be employed simultaneously. | |
| − | + | The challenge to the design team exists in understanding where and how this technology is to be located and to anticipate possible clashes between this and other services and circulation that may result. | |
| − | + | The equipment that is installed in the specialised or hybrid theatres should not impede their use in more standard cases. | |
| − | + | Communication between operating rooms and pathology and radiology can be implemented, enabling real-time consultation with other medical experts to provide a seamless and integrated delivery of care to the patient.<ref name="Ron Bridgefoot" /> | |
| − | + | The use of IT and communications may now include voice-activated control of equipment and the room environment, robotic surgery, electronic patient records and CCTV for training and consultation. | |
| − | + | ===Dirty Zone=== | |
| + | The dirty zone includes the following areas: | ||
| − | + | <u>The dirty zone includes the following areas:</u> | |
| − | + | *Dirty utility | |
| + | *Sluice | ||
| + | *Wash-up areas (scopes) | ||
| + | *TSSU/CSSD | ||
| + | *Cleaner’s room | ||
| + | *Scope-cleaning room. | ||
| − | + | ====Scope-cleaning room==== | |
| + | Washing and hanging provision is required for scopes and equipment. | ||
| − | + | ====Sluice==== | |
| + | This is a standard room of a minimum of 9m² and its documentation should be read in conjunction with the IUSS generic room documentation. | ||
| − | + | The sluice in the administration zone should be adjacent to the recovery area. | |
| − | + | <u>The sluice provides for:</u> | |
| − | + | *Cleaning and holding of used equipment for collection and sterilisation elsewhere | |
| + | *Disposal of clinical and other waste and soiled linen | ||
| + | *Testing and disposing of patient specimens | ||
| + | *Decontamination and storage of patient utensils such as pans, urinals and bowls. | ||
| − | + | <u>The sluice should include the following services:</u> | |
| − | + | *Hand-wash basin with elbow taps and gooseneck outlet in each room with splash-back, soap dispenser and paper-towel dispenser | |
| + | *Automatic bed-pan washer, in all sluices | ||
| + | *Stainless steel sluice sink | ||
| + | *Two 230V socket outlets. | ||
| − | + | Storage space for the following should be accommodated: | |
| − | + | *Clean bed pan and urinal drying racks | |
| + | *Built-in cupboard | ||
| + | *Two run-abouts, two-bucket system | ||
| + | *Soiled linen area | ||
| + | *Bumper rails to prevent bins marking walls | ||
| + | *Storage for used CSSD supplies, urine testing, detergents, urinal covers | ||
| + | *Space for large bins | ||
| + | *Shelves for wash basins and buckets. | ||
| − | + | ===Structure=== | |
| + | [[File:OT Ceiling Void Clearance.png|thumb|714x714px|Ceiling Void Clearance]] | ||
| − | + | =====Ceiling Void / Engineering Space===== | |
| + | When planning the OTU, the construction of the operating room’s ceiling detail bears some consideration. The ceiling structure above the operating theatre should be safely trafficable, without interrupting the operation below. | ||
| − | + | The designer has the option of creating a reinforced concrete slab and finishing the soffit to serve as the OT ceiling. This solution offers the advantage of providing a structural component to which the lights and pendants can be fixed directly. Unfortunately this solution requires very careful detailing and planning, as larger penetrations need to be created during the construction of the slab and they consume precious vertical space. | |
| − | + | Sufficient space should be provided for uncompromised routing of services above the operating theatre. The interstitial engineering space should provide enough room for installing and maintaining services. It is therefore helpful to allow for sufficient headroom for maintenance staff. | |
| − | . | + | Alternatively, a trafficable, flush-finished, monolithic and impervious ceiling constructed below the slab offers a more efficient solution. This solution requires that special structures need to be installed to support the lights, plenums and pendants. |
| − | + | Where ceiling void access is to be through the ceiling itself, access through removable lights is not recommended as these inevitably become damaged. Dedicated trapdoors should be installed outside of the clean zone so that maintenance staff do not need to re-enter the clean zone after being in the ceiling. | |
| − | + | Smooth cornice details are recommended to aid cleaning. Floated ceilings are not recommended. No effluent or waste pipes should be routed in the space directly above any theatre. | |
| − | + | ==Accommodation Plans== | |
| + | The flexibility of this theatre design permits natural light into the operating room by the removal of the dirty corridor, which previously ran around the perimeter. Grouping operational rooms together into effective clusters enables stores and set-ups to become tailored to case types, and helps staff identify with their location. This is particularly important for large theatre floors to reduce travel times between stores and where there is little reference/orientation to outside views. | ||
| + | [[File:Operating unit - relationship of components.png|center|thumb|750x750px|'''Operating Unit - Relationship of Components''']] | ||
| + | At the Gold Coast Hospital the operating rooms are positioned around a central sterile support area in clusters of eight. The operating rooms in turn were encircled by a peripheral patient transport corridor which enabled patients to see out. It is noted that in the Mackay Hospital Redevelopment the use of Case Carts enabled flexibility in the use of corridors because of the containment of used materials within the carts | ||
| − | + | ||
| − | + | ==User Room Requirements== | |
| − | + | Table 6: Room list for surgical facility | |
| − | + | {| class="wikitable" | |
| − | + | |+{{Anchor|Room List for Surgical facilities}}Room List for Surgical facilities | |
| − | + | | | |
| − | + | |'''''<big>ROOM</big>''''' | |
| − | + | |'''''<big>COMMENTS</big>''''' | |
| − | + | |'''''<big>STANDARD</big>''''' | |
| − | + | |'''''<big>NON-STANDARD</big>''''' | |
| − | + | |- | |
| − | + | | colspan="5" |'''GENERAL AREAS''' | |
| − | + | |- | |
| − | + | | rowspan="29" |GENERAL AREAS | |
| − | + | |'''Administrative offices''' | |
| − | + | |Outside of OTU | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |IT Switch room and UPS | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Meeting room - large | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Office – Chief anaesthetist | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Office - Chief surgeon | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Office – Doctors | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Office – Unit manager | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Office – Sister | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Doctors on call rooms with en suite ablution | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Staff toilet | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |'''Education and training''' | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Seminar room | |
| − | + | |20-30 places | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Library | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Study area | |
| − | + | |5 places | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |'''Pre-entrance to operating theatre unit''' | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Public waiting area | |
| − | + | |Allow at least 4 chairs | |
| − | - | + | |x |
| − | + | | | |
| − | - | + | |- |
| − | + | |Wheelchair accessible toilet | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Counselling room | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |'''Entrance area''' | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Lobby | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Porters’ base | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Trolley park | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Unit manager’s office | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Reception | |
| − | + | | | |
| − | + | |x | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Bay – Personal protective equipment | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |'''Restricted access area''' | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |'''Staff area''' | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Female change room with toilet & showers | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Male change room with toilet & showers | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | | colspan="5" |'''OPERATING THEATRE SUITE''' | |
| − | + | |- | |
| − | + | | rowspan="14" |CLEAN AREA | |
| − | + | |Office | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Patient holding bays | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Nurses’ station | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Patient-recovery bays | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Clean utility for recovery | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Clean passage to operating theatres | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Stores | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Clean linen | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |<nowiki>- Equipment</nowiki> | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |<nowiki>- Instruments</nowiki> | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |<nowiki>- Pharmaceutical supplies</nowiki> | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |<nowiki>- Surgical supplies</nowiki> | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |<nowiki>- Anaesthetic supplies</nowiki> | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |CLEAN AREA | |
| − | + | |Blood store | |
| − | + | |Or blood storage refrigerator bay | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | | rowspan="13" |CLEAN AREA | |
| − | + | <br /> | |
| − | + | |Equipment cleaning | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Mobile equipment bays | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |Emergency trolley | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Trolley | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Anaesthetic trolley | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Bay for mobile x-ray | |
| − | + | | | |
| − | + | | | |
| − | + | | | |
| − | + | |- | |
| − | + | |X-ray | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Ultrasound | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Laboratory area | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Medical gas store | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Anaesthetic workroom | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Induction room | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Staff rest area | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | | rowspan="3" | | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | STERILE AREAS | |
| − | + | |Staff quiet rest area | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| + | |- | ||
| + | |Staff toilet | ||
| + | | | ||
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | | | ||
| + | | | ||
| + | | | ||
| + | | | ||
| + | |- | ||
| + | | rowspan="5" |STERILE ARAES | ||
| − | + | DIRTY AREAS | |
| − | + | |Minor operating theatre | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Major operating theatres | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Scrub room | |
| − | + | |Allow 3 people minimum | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Set-up room | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Sluice for theatres | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | | rowspan="6" |DIRTY AREAS | |
| − | + | |Disposable corridor | |
| − | + | | | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Scope-cleaning room | |
| − | + | |Flexible endoscope cleaning room and store | |
| − | + | | | |
| − | + | |x | |
| − | + | |- | |
| − | + | |Sluice for recovery | |
| − | + | | | |
| − | + | |x | |
| − | + | | | |
| − | + | |- | |
| − | + | |Dirty utility | |
| − | + | | | |
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | |Cleaners’ room | ||
| + | | | ||
| + | |x | ||
| + | | | ||
| + | |- | ||
| + | | | ||
| + | | | ||
| + | | | ||
| + | | | ||
| + | |} | ||
| − | + | ==Case Studies== | |
| + | [[File:Theatre and CSSD plan (Courtesy of Mitchells Plain (District) Hospital).png|alt=Theatre and CSSD plan (Courtesy of Mitchells Plain [District] Hospital)|none|thumb|750x750px|Theatre and CSSD plan (Courtesy of Mitchells Plain [District] Hospital)<ref>MPDH Architects in Association</ref>]] | ||
| − | |||
| − | + | ||
| + | [[File:Theatre and CSSD layout (Courtesy of King George V (District) Hospital).png|none|thumb|1478x1478px|Theatre and CSSD layout (Courtesy of King George V [District] Hospital)<ref>Osmond Lange Architects</ref>]] | ||
| + | <br /> | ||
| + | [[File:Theatre layout (Courtesy of Edendale (Regional) Hospital).png|none|thumb|1168x1168px|Theatre Layout (Courtesy of Inkhozi Albert Luthuli Central Hospital)<ref>FGG Architects</ref>]] | ||
| − | + | ==Regulations== | |
| − | + | *All local Municipal laws and regulations. | |
| + | *Any other applicable Laws or Regulations. | ||
| + | *International Organisation for Standardisation (ISO), 2005. ISO 14644-3 Cleanrooms and associated controlled environments - Part 3: Test methods. Switzerland: ISO. | ||
| + | *National Health Act 2003. (c.61). Cape Town South Africa: Government Gazette. | ||
| + | *Regulations of the local Electricity Authority. | ||
| + | *South African Bureau of Standards (SABS), 1990. SANS 10400:1990 Code of practice for the application of the national building regulations. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 1993. SABS 0252-2 Code of practice Water supply and drainage for buildings Part 2: Drainage installations for buildings.Pretoria South Africa: SABS Standards Division | ||
| + | *South African Bureau of Standards (SABS), 1999. SANS 10313:1999 Protection of structures against lightning. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 1999. SANS 14644-1:1999 Cleanrooms and associated controlled environments Part 1: Classification of air cleanliness. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 1999. SANS 14644-1:1999 Cleanrooms and associated controlled environments - part 1: Classification of air cleanliness. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2003. SANS 10173:2003 The installation, testing and balancing of air-conditioning ductwork. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2003. SANS 14644-2:2003 Cleanrooms and associated controlled environments - part 2: Specifications for testing and monitoring to prove continued compliance with ISO 14644-1. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2003. SANS 14644-4:2003 Cleanrooms and associated controlled environments - part 4: Design, construction and start-up. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2005. SANS 10114-1:2005 Interior lighting Part 1: Artificial lighting of interiors. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2005. SANS 1238:2005 Air-conditioning ductwork. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2008. SANS 1424:2008 Filters for use in air-conditioning and general ventilation. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2008. SANS 7396-2:2008 Medical gas pipeline systems Part 2: Anaesthetic gas scavenging disposal systems. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2009. SANS 10114-2:2009 Interior lighting Part 2: Emergency lighting. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2009. SANS 10142-1:2008 The wiring of premises part 1: Low-voltage installations. Pretoria South Africa: SABS Standards Division | ||
| + | *South African Bureau of Standards (SABS), 2009. SANS 7396-1:2009 Medical gas pipeline systems Part 1: Pipeline systems for compressed medical gases and vacuum. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2011. SANS 1453:2011 Copper tubes for medical gas and vacuum services. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2012. SANS 10142-1:2012 The wiring of premises Part 1: Low-voltage installations. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2012. SANS 10252-1:2012 Water supply and drainage for buildings part 1: Water supply installations for buildings. Pretoria South Africa: SABS Standards Division | ||
| + | *South African Bureau of Standards (SABS), 2012. SANS 1091:2012 National colour standard. Pretoria South Africa: SABS Standards Division. | ||
| + | *South African Bureau of Standards (SABS), 2013. SANS 62040-1:2013 Uninterruptible power systems (UPS) Part 1: General and safety requirements for UPS. Pretoria South Africa: SABS Standards Division. | ||
| + | *The Occupational Health and Safety Act 1993. (c.85). Cape Town South Africa: Government Gazette. | ||
| − | + | ==List of Abbreviations== | |
| − | + | {| | |
| − | + | |'''A & E ''' | |
| − | + | |Accident and Emergency Department | |
| − | + | |- | |
| − | + | |'''AHU ''' | |
| − | + | |Air- handling Unit | |
| − | + | |- | |
| − | + | |'''CSSD ''' | |
| − | + | |Central Sterile Supply Department | |
| − | + | |- | |
| + | |'''EMS ''' | ||
| + | |Emergency Medical Services | ||
| + | |- | ||
| + | |'''HCW ''' | ||
| + | |High Care Ward | ||
| + | |- | ||
| + | |'''HEPA ''' | ||
| + | |High Efficiency Particulate Air (filter) | ||
| + | |- | ||
| + | |'''ICU ''' | ||
| + | |Intensive Care Unit | ||
| + | |- | ||
| + | |'''NBR ''' | ||
| + | |National Building Regulations SABS 0400 | ||
| + | |- | ||
| + | |'''NICU ''' | ||
| + | |Neonatal Intensive Care Unit | ||
| + | |- | ||
| + | |'''OT ''' | ||
| + | |Operating Theatre | ||
| + | |- | ||
| + | |'''OTU ''' | ||
| + | |Operating Theatre Unit | ||
| + | |- | ||
| + | |'''SABS ''' | ||
| + | |South African Bureau of Standards | ||
| + | |- | ||
| + | |'''SANS ''' | ||
| + | |South African National Standards | ||
| + | |- | ||
| + | |'''SSO ''' | ||
| + | |Switched Socket Outlet | ||
| + | |- | ||
| + | |'''UDAF ''' | ||
| + | |directional Air Flow | ||
| + | |- | ||
| + | |'''UPS ''' | ||
| + | |Uninterrupted Power Supply | ||
| + | |- | ||
| + | |'''URS ''' | ||
| + | |User Requirement Specification | ||
| + | |} | ||
| − | + | ==List of Definitions== | |
| − | + | {| class="sortable" | |
| − | + | |'''central hospital''' | |
| − | + | |means a public hospital designated by the Minister of Health to provide health services to users from more than one province. | |
| − | + | |- | |
| − | + | |'''health establishment''' | |
| − | + | |means the whole or part of a public or private institution, facility, building or place, whether for profit or not, that is operated or designed to provide inpatient or outpatient treatment, diagnostic or therapeutic interventions, nursing, rehabilitative, palliative, convalescent, preventative or other health services. | |
| − | + | |- | |
| − | + | |'''hospital''' | |
| − | + | |means a health establishment which is classified as a hospital by the Minister in terms of section 35 of the National Health Act. | |
| − | + | |- | |
| − | + | |'''operating room''' | |
| − | + | |is a room within the operating suite in which surgical or other invasive procedures can be carried out. | |
| − | + | |- | |
| − | + | |'''operating suite''' | |
| − | + | |refers to a suite of rooms within the demarcated area where surgical and other invasive procedures are carried out or where support to these procedures is provided. | |
| − | + | |- | |
| − | + | |'''barrier isolator''' | |
| − | + | |refers to a device comprising a physical film separating an operator or clinician from a work process; The work process is maintained within an isolated environment which may be held at a positive or negative pressure. | |
| − | + | |- | |
| − | + | |'''Central Sterile Supply Department (CSSD)''' | |
| − | + | |means a facility for the receiving, decontamination, preparation, packing, sterilising, storing and issuing of sterile and disinfected instruments and other reusable materials. This facility is also known as the "sterilisation and disinfection unit" (SDU). | |
| − | + | |- | |
| − | + | |'''cleaners' room''' | |
| − | pre- | + | |means a room for the storage of cleaning equipment, the drawing of clean water and the disposal of dirty water, and the washing and drying of cleaning equipment. This room may be combined with the dirty utility room. |
| − | + | |- | |
| − | + | |'''clean air''' | |
| − | + | |means air that does not contain a considered contaminant. | |
| − | + | |- | |
| − | + | |'''clean utility room''' | |
| − | + | |means a room for the storage of sterilised packs, dressings, sterile equipment and pharmaceutical supplies respectively; this area may also be used for a set-up area for ward procedures. | |
| − | + | |- | |
| − | + | |'''considered contaminant''' | |
| − | + | |means any actual contaminant, surface or airborne, that may have a certain impact for which avoidance measures are taken. | |
| − | + | |- | |
| − | + | |'''cross-contamination''' | |
| − | + | |refers to the contamination of any zone or surface by fomites, considered particulates aerosols, biological agents, fumes or gases originating from another zone or surface. | |
| − | + | |- | |
| − | + | |'''cross-infection''' | |
| − | + | |refers to the spreading of an infection from one organism to another by cross-contamination. | |
| − | + | |- | |
| − | + | |'''department''' | |
| − | + | |means a grouping of accommodation which has a specific function within a hospital; its area includes the associated internal or departmental circulation space. | |
| − | + | |- | |
| − | + | |'''dirty utility room''' | |
| + | |means a room used for the collection and temporary storage of used equipment and general ward material; it can combine the activities of the sluice room, the soiled linen and waste room and the cleaners' room. | ||
| + | |- | ||
| + | |'''emergency trolley/crash cart''' | ||
| + | |means a mobile cart used for the storage of all appropriate resuscitation equipment and pharmaceuticals. | ||
| + | |- | ||
| + | |'''equipment store''' | ||
| + | |means a room used for the storing of monkey chains, traction kits and other general equipment. | ||
| + | |- | ||
| + | |'''fresh air''' | ||
| + | |means air drawn from the outside air of a building and contamination sources. | ||
| + | |- | ||
| + | |'''high-care ward''' | ||
| + | |refers to a ward for the care and management of specific types of patients requiring a minimum of eight hours of nursing care per patient day. | ||
| + | |- | ||
| + | |'''holding area''' | ||
| + | |means an area or room where pre-operative patients in transit to a procedure room/theatre are identified and continuously monitored by nursing personnel. | ||
| + | |- | ||
| + | |'''induction room''' | ||
| + | |means an area where patients are prepared for surgery/invasive procedures prior to being transferred to the operating theatre. | ||
| + | |- | ||
| + | |'''intensive care unit''' | ||
| + | |means a unit designed, staffed and equipped for the care and management of specific patients (e.g. medical, cardiac or post-operative) requiring a minimum of twelve hours of nursing care per patient day, or for the care of a patient who requires ventilation, continuous invasive monitoring, invasive care, or who is clinically unstable and whose life is at risk. | ||
| + | |- | ||
| + | |'''main kitchen.''' | ||
| + | |means a facility suitably finished and equipped for the receipt, storage and preparation of meals, special diets and beverages | ||
| + | |- | ||
| + | |'''maternity unit''' | ||
| + | |means a unit where antenatal care is provided, babies are delivered and postnatal care is given to mothers and infants. | ||
| + | |- | ||
| + | |'''midwife obstetric unit (MOU)''' | ||
| + | |means a maternity unit usually attached to a clinic or a community health centre (CHC), which is staffed by nursing sisters or midwives. | ||
| + | |- | ||
| + | |'''milk kitchen''' | ||
| + | |means an area for the preparation of feeds for babies which must be separate from the hospital kitchen or ward kitchen; it must contain a clinical-wash hand basin. | ||
| + | |- | ||
| + | |'''mortuary''' | ||
| + | |means a facility that receives, holds and allows for the identification of bodies of patients who died in the wards, theatre or casualty department, or who were dead on arrival at the facility. | ||
| + | |- | ||
| + | |'''neonatal unit''' | ||
| + | |means a facility for premature and new-born babies requiring incubation, specific care and monitoring | ||
| + | |- | ||
| + | |'''nurse station''' | ||
| + | |means the control point for all activities in the patient-care areas. | ||
| + | |- | ||
| + | |'''nursing unit or ward''' | ||
| + | |means a unit with the facilities to accommodate patients as specified in this regulation. | ||
| + | |- | ||
| + | |'''operating room''' | ||
| + | |means a room within an operating-theatre suite in which surgical or other invasive procedures are carried out. | ||
| + | |- | ||
| + | |'''operating suite''' | ||
| + | |refers to rooms within the demarcated area where surgical interventions are performed or support is provided to these surgical activities; | ||
| + | |- | ||
| + | |'''patient room''' | ||
| + | |means a room where the patient can be accommodated. | ||
| + | |- | ||
| + | |'''procedure room''' | ||
| + | |means a room in which certain restricted procedures generally taking less than one hour can be performed without making use of general anaesthetic - e.g. endoscopies, procedures under local anaesthetic, such as suturing of lacerations, removal of skin lesions, biopsies, closed reductions and other similar procedures; may be situated outside the operating suite. | ||
| + | |- | ||
| + | |'''recovery room/area''' | ||
| + | |means the section of the operating suite specially set aside for the immediate post-operative recovery, resuscitation, nursing and special care of patients, until such time as such patients are considered to have recovered sufficiently to be safely removed from the operating suite. | ||
| + | |- | ||
| + | |'''sluice room''' | ||
| + | |means a room used for the emptying, cleaning and storage of bedpans and urine bottles; it can be combined with the activities of the soiled-linen and cleaners' rooms in the dirty utility room. | ||
| + | |- | ||
| + | |'''specialised area''' | ||
| + | |means any clinical area rendering specialised services such as intensive care, high care, or rehabilitation, for which additional space around the patient is required. | ||
| + | |- | ||
| + | |'''soiled linen and waste room''' | ||
| + | |means a room used for the collection and temporary storage of soiled linen and waste; may be combined with the dirty utility room. | ||
| + | |- | ||
| + | |'''treatment room''' | ||
| + | |means a room used for the treatment of patients in the wards, containing a clinical hand-wash basin. | ||
| + | |- | ||
| + | |'''ventilation''' | ||
| + | |means The process of supplying air to or removing air from a space for the purpose of controlling air contaminant levels, humidity or temperature within the space (ASHRAE Standard 62.1-2007, Section 3). | ||
| + | |- | ||
| + | |'''validation''' | ||
| + | |means the method of proving and documenting that an installed system or process performs reliably as intended and required. | ||
| + | |- | ||
| + | |'''natural ventilation''' | ||
| + | |means Ventilation provided by thermal, wind, or diffusion effects through doors windows or other intentional openings in the building (ASHRAE Standard 62.1-2007, Section 3). | ||
| + | |- | ||
| + | |'''ward kitchen''' | ||
| + | |means the room that forms an integral part of a nursing unit or units for the preparation of snacks and beverages; it also includes the area for the heating, storage and refrigeration of meals. | ||
| + | |- | ||
| + | |'''uninterrupted power supply''' | ||
| + | |means a battery system, which in the event of a normal mains supply failure will immediately provide the electrical supply for essential equipment and lighting. | ||
| + | |- | ||
| + | |'''surgical''' | ||
| + | |refers to a speciality in medicine that investigates or treats disease or injury by an operative procedure. Surgical procedures involve entering the body or body cavities by incision (breaking through the skin or other areas of the body) . This may be to treat a disease or injury or to enhance body appearance or function. | ||
| + | |- | ||
| + | |'''diagnostic''' | ||
| + | |refers to a variety of observations and/or tests that can be performed in order to identify a particular disease or medical problem, and to providing the supporting evidence such as the cause - e.g. various types of endoscopy, cardiac stress tests, blood tests, x-rays etc.1 | ||
| + | |} | ||
| − | + | ==Acknowledgements== | |
| − | + | '''Documents of particular reference''' | |
| − | + | 1. NHS Estates, 2004. HBN 26, Facilities for Surgical Procedures: Volume 1<ref name="HBN 26" /> | |
| − | + | '''IUSS N&S task team''' A:15: Tobias van Reenen, Edwina Fleming, Magda Coetzer, Zane Farina, Denise Sheard, Mirinda Coertzen | |
| − | + | Contributions at workshops'':'' | |
| − | + | {| class="wikitable" | |
| − | + | |Department of Public Works and Transport | |
| − | + | |Western Cape | |
| − | + | |- | |
| − | + | |Edendale Hospital clinical and nursing staff | |
| − | + | |KwaZulu-Natal | |
| − | + | |- | |
| − | + | |King Edward VIII Hospital clinical and nursing staff | |
| − | + | |KwaZulu-Natal | |
| − | + | |- | |
| − | + | |King George V Hospital clinical and nursing staff | |
| − | + | |KwaZulu-Natal | |
| − | + | |- | |
| − | + | |Inkhozi Albert Luthuli Hospital clinical and nursing staff | |
| − | + | |KwaZulu-Natal | |
| − | + | |- | |
| − | + | |Department of Health Infrastructure Department | |
| − | + | |KwaZulu-Natal and Western Cape | |
| − | + | |} | |
| − | + | '''Hosted visits to:''' | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | • Red Cross Children’s Hospital, Cape Town | |
| − | + | • Inkhozi Albert Luthuli Central Hospital, Durban | |
| − | + | • King Edward Hospital, Durban | |
| − | + | • King George V Hospital, Durban | |
| − | + | • Edendale Hospital, Pietermaritzburg. | |
| − | + | • Greys Hospital, Pietermaritzburg | |
| − | + | • Lower Umfolozi War Memorial Hospital, Empangeni | |
| − | + | • Ngwelezane Hospital, Empangeni | |
| − | + | • Mitchells Plain Hospital, Cape Town | |
| − | + | • Khayelitsha Hospital, Cape Town | |
| − | + | • G. F. Jooste Hospital, Cape Town | |
| − | + | • Worcester Hospital, Worcester | |
| − | + | • Brits Hospital, Brits | |
| − | + | • Waterfall Hospital, Midrand | |
| − | + | • Royal Alexandra Hospital, Brighton | |
| − | + | Fiona Stanley Tertiary Hospital, Perth | |
| + | [[Category:Clinical Services]] | ||
| − | + | ==References== | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
<references /> | <references /> | ||
Latest revision as of 17:08, 14 July 2020
Please help to expand this page. |
Contents
- 1 Policy and Service Context
- 2 SERVICE CONTEXT
- 3 Planning and design
- 3.1 Overview
- 3.2 General Planning and Design Requirements
- 3.2.1 Objectives of the operating theatre unit
- 3.2.2 Strategic planning considerations
- 3.2.3 Infection-control policies and procedures
- 3.2.4 Healing environments
- 3.2.5 Air quality
- 3.2.6 Patient privacy
- 3.2.7 Artificial lighting
- 3.2.8 Finishes
- 3.2.9 Child-friendly environment
- 3.2.10 Controlled access
- 3.2.11 Control of waste
- 3.2.12 Communications
- 3.2.13 Storage
- 3.3 Location
- 3.4 Sterile Core Principle
- 3.5 Traffic Flow Paths
- 3.6 General Zone
- 3.7 Clean zone
- 3.7.1 Holding area – Pre-operative
- 3.7.2 Central nurses’ station
- 3.7.3 Recovery area – post-operative
- 3.7.4 Staff rest room
- 3.7.5 Anaesthetic induction room (optional)
- 3.7.6 Storage
- 3.7.7 Bay – mobile equipment storage
- 3.7.8 Blood store
- 3.7.9 Laboratory area
- 3.7.10 Medical gas storage
- 3.7.11 Store – special instruments
- 3.7.12 Store – pharmaceutical
- 3.7.13 Store – linen
- 3.7.14 Anaesthetic workroom
- 3.8 Sterile Zone
- 3.8.1 Scrub-up/gowning room
- 3.8.2 Set up/Setting out/Preparation
- 3.8.3 Operating Theatres (Sterile Zone)
- 3.8.4 Operating theatre sizes
- 3.8.5 Theatre types
- 3.8.5.1 The general-surgery operating theatre
- 3.8.5.2 The Obstetrics Operating Theatre
- 3.8.5.3 The Orthopaedics Operating Theatre: – Ultraclean / Laminar-flow
- 3.8.5.4 The cardiothoracic operating theatre
- 3.8.5.5 The Neurosurgery Operating Theatre
- 3.8.5.6 The Ophthalmology Theatre
- 3.8.5.7 The Urology Theatre
- 3.8.5.8 The Bronchoscopy Theatre
- 3.8.5.9 The Paediatric Operating Theatre
- 3.8.5.10 The Burns Theatre
- 3.8.5.11 Digital Operating Theatres
- 3.8.6 Day-surgery unit
- 3.8.7 IT Requirements
- 3.9 Dirty Zone
- 3.10 Structure
- 4 Accommodation Plans
- 5 User Room Requirements
- 6 Case Studies
- 7 Regulations
- 8 List of Abbreviations
- 9 List of Definitions
- 10 Acknowledgements
- 11 References
Policy and Service Context
Introduction
Surgical and diagnostic facilities range from procedure rooms, where minor procedures may be performed, to operating theatres where more complicated procedures are performed. These require a full medical team and need to occur in dedicated hospitals with dedicated areas designed for and equipped with special lighting, equipment and air-handling systems. This area of the hospital is usually contained in the Operating Theatre Unit (OTU), which provides a highly controlled environment for the operative and perioperative care of patients who are undergoing diagnostic and surgical procedures under anaesthesia or sedation.
“The Operating Theatre Unit provides a highly controlled environment for the operative and perioperative care of patients who are undergoing diagnostic and surgical procedures under anesthesia”
Surgical procedures
Medical and surgical procedures are categorised according to their urgency, body system involved, department they are conducted in (e.g. dedicated operating rooms for specialised procedures such as orthopaedic, cardiac surgery, neurosurgery for which different equipment is used), type of procedure, degree of invasiveness and any special instrumentation that may be used (e.g. an endoscopic suite or catheterisation laboratory).
Surgical procedures are performed by a surgical team in a dedicated operating room and may be:
- Elective procedures: the patient chooses when and if to have the procedure.
- Required procedures: these need to be done but are not necessarily done immediately.
- Emergency procedures: these are often a matter of life or death and are required due to an urgent or traumatic event.
Surgical team members
The composition of the surgical team will depend on the surgery to be performed and may include:
- The surgeon, a qualified physician specialised in surgical procedures, who leads the team and is responsible for performing the surgery.
- The anaesthesiologist, a qualified physician specialised in anaesthesia, who is responsible for the safety of the patient during anaesthesia and for pain management. Anaesthesiologists are involved in all three stages of surgery (pre-operative, operative and post-operative).
- Nursing staff, which include:
- nursing staff involved in the care of the patient throughout the perioperative period;
- the scrub person, who prepares the setup and assists the surgeon during surgery;
- the circulating person, who supports the team and collects supplies; and
- the anaesthetic assistant, who assists the anaesthetist.
Support staff
These include:
- porters
- cleaners
- staff nurse
- clerks
- CSSD staff.
Patient care[1]
The surgical team has the responsibility of caring for the patient during the perioperative period, which includes the pre-, intra- and post-operative management of the patient - i.e. care given to the patient before, during and after surgery.
- Pre-operative care is the preparation and management of the patient prior to surgery and occurs in both the inpatient ward and the holding area in the operating theatre unit.
- Intraoperative care is the management of the patient during the operative procedure whilst in the operating room. This period begins when the patient is transferred onto the theatre table in the operating room and ends when the patient is transferred to the recovery area. During this period the patient may be anaesthetised, prepped and draped, and the operation is performed.
- Post-operative care is the management of the patient after the procedure until discharge and includes care in the recovery area in the operating theatre unit and the inpatient facility.
Surgical disciplines[1]
The most common surgical disciplines include:
- General surgery - this includes surgery by general surgeons, who operate on almost any part of the body and who refer patients to relevant specialists when other specialised surgery is required.
- Cardiothoracic surgery - the cardiothoracic surgical team performs procedures within the chest, including the heart and its valves, the lung, oesophagus, chest wall and blood vessels.
- Neurosurgery - the neurosurgical teams specialise in surgery to the nervous system, including the brain, spine, peripheral nervous system and their supporting structures.
- Oral and maxillofacial surgery - the maxillofacial surgical teams deal with surgical problems of the head and neck (i.e. the ears, sinuses, mouth, pharynx, jaw, etc.).
- Reconstructive and plastic surgery - this surgical team performs surgery on abnormal structures of the body due to injury, birth defects, infection, tumours or disease, as well as cosmetic surgery to improve a patient’s appearance.
- Transplantation - this advanced surgical team performs surgery specific to organ-transplant techniques, such as heart-lung transplants, liver transplants and kidney/pancreas transplants.
- Urology and renal transplantation - this surgical team performs surgery related to the kidney, kidney stones, bladder, urethra and ureters.
- Gastrointestinal surgery - digestive tract (stomach, bowels, liver and gall bladder).
- Vascular surgery - this involves diagnosis and treatment of arterial and venous disorders, such as aneurysms, lower-extremity revascularisation, and other problems.
- Paediatric surgery - this surgical team is specially trained to perform procedures on neonates, infants and children.
- Ear, nose and throat surgery - this team is specially trained for surgery procedures to the ear, nose and throat.
- Obstetric and gynaecological surgery - this surgical team will perform caesareans (both elective and emergency), hysterectomies, removal of ovaries and other female-specific surgical procedures.
Ophthalmology - this involves surgical treatment related to procedures to the eyes.
- Orthopaedic surgery - this involves surgical treatment related to the musculoskeletal system.
Surgical techniques[1]
These include the following:
- Open surgery - this requires a large incision to access the relevant area of skin and tissues to allow the surgeon direct access to the internal structures or organs involved (e.g. to remove an appendix.
- Laser surgery - this involves the use of a laser to allow the surgeon to precisely cut tissues instead of using a physical knife or scalpel. An example of its use would be in surgery to the eye and/or larynx.
- Microsurgery - this involves the use of an operating microscope positioned above a small incision, allowing the surgeon to visualise small structures such as those in the eye or nervous system.
- Robotic surgery - a surgical robot is used under the direction of the surgeon to control the instrumentation.
- Minimally invasive surgery (MIS) - this involves smaller incisions through the skin to insert a specially designed instrument into the body cavity or structure. The surgeon can see into the body through the use of associated devices. An example of MIS is the removal of the gall bladder.
- Reconstructive surgery - this involves the reconstruction of an injured, mutilated or deformed part of the body.
- Cosmetic surgery - this is performed to improve the appearance of an otherwise normal surface structure of the body.
- Transplant surgery - this involves the replacement of an organ or body part by removing the diseased organ and replacing it with a donated, healthy organ.
- Endoscopic procedures - this refers to any procedure using a device known as an endoscope, to look inside the body for medical, diagnostic or surgical purposes.[1]
- Interventional radiology - these procedures take place in the diagnostic and interventional radiology department.
Additional guidelines available
- SASA Practice Guidelines (2006)
- R158 (1996)
- RCA – Guidelines for Provision of Anaesthetic Services (2009)
- NHS Estates Guideline (2006)
- AAGBI Theatre Efficiency (2003)
- Indian Experience 2007
- 2004 HBN 26-Vol 1, Facilities for Surgical Procedures
- Australian health facility guidelines.
SERVICE CONTEXT
Hospital categories of service
The business case and the health brief define the correct package of service and the operating theatre number per facility based on the Provincial Strategic Transformation Plan and the government policy document: Government Notice - R.185, 2nd March 2012, National Health Act 61/2003.
| District | Regional | Tertiary | Central Hospital |
| General surgery | General and specialist surgery
Orthopaedic surgery Ophthalmology Obstetric surgery |
-Sub-speciality surgery
Orthopaedic surgery Ophthalmology Paediatric surgery Oral and maxillofacial surgery Cardiothoracic surgery Neurosurgery Urology Gastrointestinal surgery Vascular surgery Obstetric and gynaecological surgery -Facilities for holding, surgery and recovery of highly infectious patients
|
-Super specialties
-Transplants-Paediatric surgery -Facilities for holding, surgery and recovery of highly infectious patients |
Determining the number of operating theatres (OTs) required
The following rules of thumb relate the number of operating theatres to the number of beds in a hospital:
1 OT per 50 inpatient beds or 1 OT per 25 surgical beds.
The WHO Planning & Design Guide proposes the following calculation method:
Multiply no of surgical beds (160) by no of operating days/year (260)
- surgical bed-days available / year = (A)
e.g.
Divide A by average length of stay in surgical ward (4 days)
- maximum no of surgical patients admitted / year = (B)
e.g.
Divide B by actual no of working days (300)
- no of surgical operations expected / day = (C)
e.g.
Multiply C by average hours per operation (3)
- OT hours / day = (D)
e.g.
Divide D by actual no of working hours in the OT (6)
- No of operating theatres required = (E)
e.g.
Factor in occupancy rate (75%)
- corrected no of operating theatres required = (F)
e.g. theatres
Refer to: 2004 HBN 26-Vol 1 Surgical procedures: Appendix 3 – Capacity Planning
Planning and design
Overview
This section illustrates the desired planning principles and design considerations with applied examples to support the planning process.
Planning and design guidance, design considerations, functional relationships between the OTU and hospital departments and relationships therein are discussed
Workflow diagrams within departments are provided to assist in understanding the intradepartmental relationships in support of functional flow to ensure productive service delivery.
Workflow diagrams are provided to explain the flow of:
- patients, clinical staff,
- support goods and services,
- maintenance staff, as well as
- the flow of the public through the OTU.
The detailed room diagrams with accompanying guidelines are provided to clarify an understanding of the different space requirements and room-specific specifications.
During the planning and design stages, it is important that input from staff, technicians, cleaning staff, reception staff, porters, equipment personnel, clinical and nursing staff be encouraged and sought. This would promote efficient and appropriate operational functions in the OT.
General Planning and Design Requirements
The OTU is a specialised facility within the hospital where lifesaving or life-improving procedures are carried out on the human body by invasive methods under strict aseptic conditions in a controlled environment by specially trained personnel to promote healing and cure with maximum safety, comfort and economy. It is imperative that the OT is designed scientifically to ensure sterility, easy maintenance and effective utilisation.
Objectives of the operating theatre unit
The primary objectives of an operating theatre unit can be summarised as follows:
- Patient-focused care;
- Successful surgical or diagnostic procedures for the patient;
- Preservation of patient dignity at all times;
- Maximising efficiency in terms of throughput and outcomes. Due to the complexity of the OTU, the procedures performed and the technical equipment required, this life-saving unit is a major cost centre within the hospital and, as such, must function efficiently and be designed to be utilised effectively; and
- Ensuring maximum standards of safety of the patient through
- safe anaesthesia,
- promotion of a high standard of asepsis,
- the creation of a “sterile” environment in the OT and the set-up room to reduce the risk of infection,
- promoting clean equipment in the operating theatre, and
- Recruitment, development and retention of appropriately skilled staff that is achieved through optimising working conditions and providing a working environment;
- Facilitation of coordinated services;
- Clean storage of consumables, medicine and equipment pertinent to the procedures to be performed;
- Provision of administrative functions to ensure that the OTU performs effectively by optimising utilisation of the OTs and staff time;
- Security for the patient, for staff and for equipment;
- Minimise maintenance;
- Ensure functional separation of spaces;
- Control of traffic flow within the OTU; and
- Infection control - exclusion of contamination from outside the theatre achieved by
- limiting the number of people in the operating theatre,
- control of the environment - temperature, humidity, and surface and airborne contamination levels are to be maintained within prescribed levels, and
- the sterilisation of instruments and re-useable instruments used in the procedure.
Strategic planning considerations
Before proceeding with the planning and design of the OTU, it is important to clarify the following:
- The category of hospital and the levels of service required of that hospital.
- How many operating theatres will be required in the OTU.
- The type of procedures to be performed and the types of theatres required for those procedures.
- OT sizes required.
- OTU department location in relation to the rest of the hospital.
- Infection control – the hospital policies will determine the zoning within the department to an extent. Infection-control teams should be consulted from the onset of the planning and design process, and should remain members of the planning team throughout - from the business case to completion and occupation of the new or upgraded facility. Refer to Infection prevention and control for further guidance.
- Structural implications with regard to existing or new structures. These relate to the load-bearing capacity, as well as noise and vibration concerns.
- Constraints created by a modular construction where a specific grid has been adopted.
- Theatre equipment requirements in terms of environmental quality, vibration, structure, electrical and mechanical.
- IT & communication requirements especially related to the digital theatres.
- Decontamination of equipment, medical devices and instruments for re-use is essential in an OT in order to reduce the risk of contamination. Central sterile services department (CSSD).
Infection-control policies and procedures
The introduction of microbial contamination to the patient is the greatest risk in the operating theatre and must be the foremost focus of all design of spaces within these units, regardless of whether the space is a minor procedure room or specialist operating theatre. Surgical-site infections acquired during an operation can be fatal for the patient. To effectively reduce the risk of surgical infections, these areas and their environments must comply with strict policies and procedures.
These procedures are essentially common to all types of surgical facilities, especially with regard to:
- the operational procedures,
- the reprocessing of re-useable instrumentation and devices used for these procedures,
- infection control, and
- the cleaning and disinfection of the physical space.
“A clean operating room environment with sterile (or correctly decontaminated) equipment with restricted access and appropriately attired staff can go a long way to reducing the risks of surgical site infections"
Healing environments
Historically, operating theatre units have concentrated on designs that address only the technical aspects and the need for an uncontaminated, sterile or clean environment, with slim regard for the need to make patient and staff spaces pleasant and appealing. Today, a number of patients undergo surgery without a general anaesthetic, remaining conscious throughout the procedure. It is therefore important that the environment created within the OTU is soothing and encourages a healing environment. Design of the OTU environment needs to consider the needs of the theatre staff, potentially traumatised patients, guardians of minors and care for minors themselves. The evidence-based considerations and recommendations are discussed below.
Daylight
Studies indicate that the majority of people prefer indoor spaces that are illuminated by sunlight (Van den Berg, 2005). Lack of natural light is one of the most common complaints made by OTU staff about their working environment. As daylight tends to be brighter and renders a natural spectrum of colours in an indoor space, it is important to try and design elements that allow natural light into the OTU. Illumination by natural daylight has benefits for both clinical outcomes and the wellbeing of occupants. Where natural sunlight is introduced into the operating theatre, potential problems of reflection on digital screens and glare at specific times of the day can arise. These problems need to be identified, understood and mitigated.
The following areas should be provided with natural light, whenever possible:
- Operating theatres
- Recovery unit
- Waiting area
- Staff room.
For more detailed information, refer to Hospital Design Principles.
Noise
Noise and sound attenuation is an aspect often overlooked in the design of the OTU. Special attention is required when detailing doors, ceilings and the selection of trolley-wheels, etc.). Quiet retreats are also important for staff to sit and rest in between cases. The unwanted propagation of sound and speech between adjacent rooms should be prevented though carefully considered design and the observation of acoustic principles.
Views
Windows in staff areas, recover
Where OTU areas are provided with views to the outside, these views should be well considered and should not be distracting to the theatre staff. External windows in operating theatres may create a pleasant indoor environment at the expense of the patient’s privacy. For this reason, access to external areas that could provide sight into the theatre should be highly restricted. Windows installed in operating theatres should be flush and sealed on the inside. It is advisable to consider using double-glazed window panels with internal blinds which can be operated from inside the theatre.
Air quality
Air quality is critical in operating theatres. Air quality is quantified in terms of:
- Operative temperature
- Radiant temperature
- Humidity
- Airborne contamination (odour, biological and particulate)
- Air velocity.
These aspects are addressed in Building engineering services and further in this document.
Patient privacy
When designing the OTU, it is important to consider views and lines of sight within the facility from the aspect of patient privacy. Patients are especially vulnerable in the OTU as, at times, they may be both unconscious and uncovered.
Artificial lighting
Artificial lighting needs to be carefully considered in the design of the OTU as each space has different requirements. The lighting needs to provide the level of illuminance required to suit the activities in the relevant space. Placement of fittings is crucial in all the patient areas including the recovery area, the holding area, induction (anaesthetic) rooms, operating theatre and staff areas. Refer to Building engineering services for guidance on lighting levels and quality.
Finishes
Refer to Materials and finishes for a comprehensive specification of finishes.
Finishes, equipment and materials must be easy to maintain and clean, as well as observe infection-control principles. Materials should be selected to minimise maintenance and be sustainable, as well as compatible with their intended function. Special design consideration should be applied when planning spaces, corners, junctions, work tops, etc.
Child-friendly environment
Children should be separated from adult patients in the OTU. Separate holding and recovery areas need to be provided for children when sharing theatres with adults. These spaces must allow for parents to accompany their children. The spaces for children must create a calm environment suitable to children.
Controlled access
The maintenance of a highly controlled environment in the OTU requires restricted and controlled access into the OTU. Automated sliding doors assist in the maintenance of the hygienic environment by limiting the touching of common-use surfaces. Openable windows in the OTU are not acceptable.
Control of waste
Waste generated in the OTU must be treated appropriately as it has considerable environmental impact.
Bio-medical waste raises considerable environmental, biological and social issues. It is beyond the scope of this guidance document to explore legal and safety issues at length.
The reader is referred to the IUSS:GNS Waste disposal and IUSS:GNS Hospital mortuaries guidance documents for more information on anatomical waste and limb disposal.
Communications
Planning should take into consideration the fact that telephones are required throughout the OTU to facilitate good communication. This needs to be planned in conjunction with the system to be used throughout the hospital. It is important that noise reduction is considered with regard to telephone ringtones, and a subtle flashing indicator light may be more appropriate.
Phones need to be easily accessible, especially in areas where patients wait, recover, etc.
Storage
Storage space for theatres is easily underestimated. Planning should ensure that, prior to design, storage requirements are sufficiently identified and included. Storage planning should include for large equipment such as additional theatre tables, anaesthetic machines, mobile machinery - as well as pharmaceutical supplies, instruments, linen and consumables. Each discipline in the OTU has specific storage needs.
Depending on the size of the OTU and hospital policy, storage can be in a series of separate rooms or can be managed from one point in a central area. Pharmaceuticals are stored separately.
Shelving needs to be durable, washable, easily disinfected and have a hygienic finish to the surface.
Open-plan storage areas should be clearly delineated to help prevent overflow and creep of space used for storage. The flow of clean and dirty materials needs to be considered in the planning of storage areas. Where insufficient storage is provided, it is common for circulation space such as the “dirty” passages to become an ad hoc storage area, such as seen in the image to the right.
Public healthcare facilities are subject to lengthy procurement lead times. In order to maintain the requisite service levels, good management of these facilities demands the maintenance of high stock levels. For this reason it is normal for public health facilities to demand between two and three times the storage space of public hospitals.
Location
The OTU should be:
- located in an area accessible to the critical-care unit and supporting services like the CSSD, x-ray and laboratory;
- located away from traffic and other potential sources of disruptions and noise;
- located such that daylight must not distract lighting in the OT;
- located and arranged to prevent non-related traffic through the OTU;
- the OTU must be easily accessible from the emergency department, labour unit, surgical wards and ICUs;
- the Central Sterilising Services Department (CSSD) could be adjacent to the OTU, but should not be placed back-to-back or adjacent to a theatre room in order to prevent potential cross-contamination;
- the design of the OTU should allow for ease of access to the storage areas for delivery of OT consumables; and
- controlled access from an external corridor is highly desirable.
Sterile Core Principle
The main principle behind the design of an OTU is the establishment of a central sterile core, which consists of the patient on the operating table, the surgeon and scrub nurse, the scrub room, the set-up room and induction room (where applicable).
The clean zone connects the OT via the clean passage to the holding and recovery areas and the store rooms that directly supply the OT. The clean zone separates the OT (sterile zone) from the potentially contaminated areas (the general zone) such as the offices, staff change areas, reception and the disposal areas (the dirty zone) such as the sluice and waste areas. In ultraclean theatres an additional ultraclean condition is established within the unidirectional airflow (laminar flow) zone.
The four zones depicted in the diagram are areas of varying degrees of cleanliness in which the bacteriological count progressively diminishes from the outer to the inner zones (sterile core), and is maintained by a differential pressure gradient cascading from the inner zone (sterile core) to the outer zone. This pressure gradient is established and maintained by the ventilation system. For additional information on the design, classification and validation of the clean zones the reader is referred to Building engineering services.
Important principles to incorporate in the planning and design include:
- Exclusion of contamination from outside the OT;
- Separation of clean areas from contaminated areas within the OTU; and
- Efficient, controlled traffic patterns within the OTU.
| ZONE | ACCOMMODATION SPACES | WORKING AREAS |
| GENERAL | External area waiting area, porters’ room | Unrestricted area outside the operating theatre where street clothing is worn. |
| Receiving lobby, unit manager’s office, reception, trolley bay (optional) | ||
| Doctors’ offices, staff lockers area, ablutions, on-call rooms, staff change areas | ||
| Training/meeting rooms | ||
| CLEAN ZONE | Storage support areas for theatres, nurses’ station, theatre clean passage, holding area and recovery area, staff rest areas | Semi-restricted area
Restricted to authorised personnel only Theatre attire is worn |
| STERILE ZONE | Theatres, scrub area, set-up areas,
induction room (anaesthetic room) |
Restricted area where procedures are performed
Authorised personnel only |
| DIRTY ZONE | Dirty passages, dirty utilities, waste areas, clean up areas | Restricted area outside the operating theatre where street clothing is worn |
Traffic Flow Paths
The OTU design must prevent cross-traffic of staff and supplies from the decontaminated/soiled areas to the sterile/clean areas. The use of facilities external to the operating theatre for soiled/decontaminated processing, clean assembly and sterile processing must be designed to move the flow of goods and personnel without compromising universal precautions or aseptic techniques in both departments.
The following are key planning principles for designing traffic flow paths in surgery units:
- Patient and materials routes should move progressively forward without unnecessarily looping back.
- Ensure pre-operative and post-operative patients do not meet at any point in the unit (except perhaps at the point of entry/exit.
- Eliminate crossover circulation points.
- Reduce double-handling of patients and supplies.
- Reduce patient and staff travel.
Modern theatre layouts tend to rely more on creating operational policies than physically separate routes to control traffic flow in the theatre unit. The advantage of this approach is that this offers opportunity for a more efficient design although the reliance on policies exposes this unit to risk from human error and discipline issues.
Patient flow pathway
The patient is collected from the inpatient unit (ward) by the theatre porter or brought to the theatre area accompanied by a nurse from the ward, ICU or emergency centre. At the OTU, the patient is brought through the access-controlled doors into the OTU lobby area, where the patient is transferred to the care of the OTU staff. At this point the patient may be transferred onto a theatre trolley if not already on one.
The patient is wheeled by the OTU staff through the second set of doors, across the red line into the restricted OTU area. The patient is kept in the holding area, cared for by the nursing staff, until called to theatre by the anaesthetist/surgeon.
The patient is wheeled into the induction room, or taken straight into the theatre where the anaesthetist is waiting to anaesthetise the patient. From the induction room, the patient is taken into the operating theatre and transferred to the theatre table. The surgeon performs the procedure on the patient once the anaesthetic is effective.
Upon completion of the operation, the patient is transferred onto the patient trolley, and then taken to the recovery area to be cared for by the nurses under the supervision of the anaesthetist.
Once the patient’s condition is stable, the patient is then wheeled out of the OTU red-line area into the lobby area and out into the external passage, then on to the ward or ICU. The patient may be handed over to and collected by the ward staff or taken to the ward or ICU by the theatre staff when discharge criteria have been met.
Staff flow pathway
The flow of staff involves a number of clearly defined personnel:
- Doctors
- Nursing staff
- Service staff.
All personnel entering and leaving the OTU must be fully gowned in correct theatre attire within the red-line area (clean and sterile zones). This requires that personnel wishing to enter the clean and sterile areas must first change and gown up in a change area before entering the red-line area. These change areas must be separated into male and female change areas.
Personnel exiting the red-line area will be required to remove the theatre gown, head and foot covers in the change areas prior to exiting the OTU.
For new facilities, the red-line area could be demarcated as running through the change rooms, thereby classifying the change rooms as an intermediate space or “grey” area between clean and non-clean areas. Grey areas should be serviced and operated as if they were within the clean area, but allow for the practicalities of transition between clean and non-clean areas. Staff toilets should not be located within change rooms, grey areas or red-line areas as this could entice staff to use their toilets while still dressed in theatre garb. The inclusion of showers within the change rooms should be considered only where staff may need to shower before leaving the OTU. Dedicated ablution facilities are preferred for this purpose.
Services flow pathway
The routes and method of transport of waste and contaminated items through the operating unit need to be carefully considered in how they pertain to cross-infection, contamination and patient views. A one-way flow of supplies into the operating room, and then of soiled goods and trash out of the operating room, is preferred. The shared use of a corridor for staff and patient access into the OR is acceptable, but this same corridor should not be used for delivery of sterile supplies into the OR. Sterile supplies and instruments should have a separate, dedicated pathway from the central sterile supply into the operating room without encountering staff or patient traffic, whether in scrubs or not.
A separate service corridor backing on to the theatres could be a solution. This corridor will link through to the CSSD and the dirty utility room, from which waste can be collected externally.
It may be helpful not to think of this corridor as a “dirty” corridor as it then frequently manages to live up to its name. The aesthetics, air quality and architectural finishes of this zone should be the same as for the clean passage.
General Zone
The protective zone provides for:
- The admission and reception area with general overseeing of day-to-day operations, control of entry and exit from the OTU and completion of administrative tasks.
- Administrative and staff areas, including change rooms, office and administrative space.
- Offices for doctors and nursing staff.
- Overnight rooms for doctors and staff on call.
| PROTECTIVE ZONE | ||
| Standard room | Non-standard room | |
| Administrative offices | ||
| IT Switch Room | X | |
| Meeting Room – Large | X | |
| Office – Chief Anaesthetist | X | |
| Office - Chief Surgeon | X | |
| Office - Doctors | X | |
| Office – Unit manager | X | |
| Office – Sister | X | |
| Doctors on call rooms with en suite ablution | X | |
| Staff toilet | X | |
| Education and training | ||
| Seminar room | X | |
| Pre entrance to theatre unit | ||
| Waiting | X | |
| Entrance area | ||
| Trolley park area | X | |
| Entrance lobby | X | |
| Office-porters (optional)
Unit manager’s office |
X | |
| Reception | X | |
| Bay – Personal Protective Equipment | X | |
| Restricted access area | X | |
| Staff area | ||
| Female change room with toilet & showers | X | |
| Male change room with toilet & showers | X | |
Administration offices
Office space is to be provided as per office space norms.
The offices are to be located close to the entrance or exit and must be outside of the clean and sterile areas. Depending on the size of the OTU, office space may need to be provided for the:
- Chief anaesthetist
- Chief surgeon
- Doctors’ offices:
- Principal specialist
- Senior specialist
- Registrars
- Anaesthetic secretary x 1
- Unit manager
- Operational managers
- Sisters’ office
- IT –Switch Room.
Seminar room
This is a standard seminar room for meetings and training, to be located within the office area.
Services include:
- Plugs for computers and a projector
- Data points
- Video and audio point
Consider:
- Chairs and a large table
- Screen
- Small lockable cupboard for equipment.
Overnight stay
The overnight stay is a room for staff on call that may need to rest while waiting to be called to the OTU. Provision should be made for single-bed units with a shower/toilet facility en suite, or for a shower/toilet facility to be shared between two separate bed units.
The doctors’ overnight rooms must be external and adjacent to the theatres with immediate access in the event of an emergency and shall be designed considering the following:
Services to include:
- Two double-socket outlets
- Telephone
- Data point
- Ablution with shower and toilet, either en suite per bed unit, or shared between two bed units.
- Considerations:
- Privacy
- External window
- Bed and side table
- Desk with chair
- Mirror
- Cupboard for clothes.
Pre-entrance
Waiting area
Prior to entrance into the OTU there should be a waiting area for the patient’s escorts or family members to wait, should there be no such facility on the ward. A small counselling room off the waiting area should also be provided for doctors to speak privately with waiting family members.
Trolley park area
A trolley park area is required, where theatre policy requires patients to be fetched from the ward and transported on a theatre trolley to the theatres.
Entrance lobby
There should be one main entrance to the theatre unit which is access-controlled and through which staff pass and patients and supplies are carried. Disposals should be removed separately through an alternative exit that is controlled from reception. Entry should be controlled by an intercom system with CCTV linked to the theatre reception area. Staff access can be controlled by access cards. However, the type of access control chosen must not inhibit emergency escape from the theatre unit in the case of fire.
The entrance area should have two double automatic sliding doors to allow for the transfer of trolleys and patients on beds accompanied by clinical staff. A minimum clear door opening of 1800mm is required with the lobby passage area being a minimum of 3000mm wide x 4400mm long to allow for two beds to pass each other, as well as accompanying staff and equipment. The doors should be supplied with kick-plates and stainless steel door protectors. Provide clear demarcations on the floor for entrance control.
The entrance lobby should have the access-controlled door off the main passage that is operated from OTU reception desk within the OTU. The patient is wheeled through these doors into a lobby (interim space), where the staff from the OTU receive the patient from the ward staff. The patient is then wheeled through into the holding area over the red-line area, optionally through a second set of automated doors.
Important considerations include the following:
- There must be restricted access control over all persons entering and exiting the OTU.
- Glass sliding doors at entrance - first set.
- An optional separate glass sliding door into the theatre clean passage from the holding and recovery areas, providing some screening when necessary.
- A red line 50mm wide at the pre- and post-operative entrances, and after the staff change room.
- The interim space to receive patients should be 9m² minimum.
Refer to the case studies included in this document for examples.
Porters’ base
A porters’ base should have access to the main passage and the lobby area.
Unit manager’s office
The unit manager’s office should have a viewing window into the lobby to be able to monitor all patients, staff and other personnel entering and exiting the theatre unit. Access from the unit manager’s office into the theatre unit is also required.
Bay – personal protective equipment
An open storage bay for location of personal protective equipment such as gloves, gowns, overshoes, caps and masks should be located within the interim space of the entrance lobby, at the entrance to the OTU. The bay must be deep enough to allow storage of gloves, gowns, overshoes and masks. A minimum area of 2m² is required.
Reception
The reception area is the central area of communication for the theatre unit. The theatre clerk works from this desk and should have an unobstructed view of the main entrance, the waiting area, the lobby area as well as a view into the theatre unit and staff entrance from the change areas.
Staff areas
Change
Staff change rooms are for staff to change into appropriate operating-room attire, and to store their street clothing. Clinical staff encounter infection and handle contaminated instruments and dressings while in the OTU during the day, and therefore need to shower and change at the end of a shift (or during a shift, should the need arise).
Appropriate change rooms shall be provided separately for male and female personnel (nurse, doctors and technicians) working within the Operating Unit.
Staff change rooms should be adjacent to the theatres. Entrance to the staff change areas, prior to gowning and entering the operating-theatre suite, should be off the main passage external to the operating-theatre suite. These staff change rooms shall be arranged to encourage a one-way traffic pattern so that personnel entering from outside the surgical suite can change and move directly into the OTU red-line area (restricted area within the OTU).
Once inside the change room, staff collect clean gowns, caps and shoe covers before changing into their gowns. The change rooms shall contain adequate lockers, showers, hand basins and space for donning of surgical attire and shoes.
Once changed, staff are then permitted to exit the change room into the operating suite through a separate door.
After staff have completed their tasks within OTU, they exit through a door into the change area where they discard their gowns, caps and shoe covers before dressing and exiting through the door to the external passage.
The total area should be divided into male and female change areas and sized according to the number of staff in the operating-theatre suite.
A minimum of 8-9m² per operating theatre or 4m² for a single person, increasing by one m² for each additional person is required. Space provision should take into account peak numbers of full time staff, students and visitors at any one time.
Access will be required to showers, toilets and decontamination facilities.
Consider the following:
- Secure storage of personal property is essential.
- Full-length mirrors, towel rails, benches, hooks and rails, full-length lockers.
- Mobile bins for soiled laundry.
- Seating/benches to sit on while changing.
- Shelves for clean gowns, hats, footwear covers.
- The change room entrance door shall be provided with locks or electronic access devices to prevent the entry of unauthorised persons into the OTU.
- Hair-dryer outlet.
- Toilets. This is to be a room containing a toilet and hand basin.
- Toilets shall be provided at the minimum ratio of one per operating room but no fewer than two in total (1 per 8 staff).
- Staff toilets should not be located within change rooms, grey areas or red-line areas as this could entice staff to use their toilets while still dressed in theatre garb.
- Showers shall be provided at the minimum ratio of one per two operating rooms, but no fewer than two. Provide:
- a privacy latch
- bench for clothes
- hook for clothes
- walls to be full height.
- The above toilets and showers are to be divided equally between male and female change rooms.
Clean zone
The clean zone within the OTU separates the sterile core from the non-clean or contaminated areas and includes:
| Clean Zone | ||
| Standard room | Non-standard room | |
| Holding area – pre-operative | x | |
| Recovery area – post-operative | x | |
| Nurses’ station | x | |
| Clean passage | x | |
| Stores: | ||
| Clean linen | x | |
| Equipment | x | |
| Instruments | x | |
| Pharmaceutical supplies | x | |
| Surgical supplies | x | |
| Anaesthetic supplies | x | |
| Blood store | x | |
| Equipment cleaning | x | |
| Passage to operating theatres | x | |
| Induction room | x | |
| Bay - mobile equipment | x | |
| Laboratory area | x | |
| Medical gas storage | x | |
| Bay - x-ray equipment | x | |
| Anaesthetic workroom | x | |
Standard rooms as indicated in the table above are described in the IUSS standard-room documents. Non-standard rooms are described below.
Holding area – Pre-operative
This space is for patients waiting to have surgery. The area is close to the entrance lobby but within the red-line restricted-access area.
Services to include:
| -Hands-free wash hand basin. | 1 per 6 bays |
| -Oxygen point | 1 per trolley |
| -Suction point | 1 per trolley |
| -Electrical points | 3 per trolley |
| -Emergency call system | 1 per trolley |
| -Lighting | 2000 lux |
The patient-holding area should be as follows:
- Allow for trolley space, with curtain rails for privacy.
- The trolley cubicles must also be provided with intravenous fluid rails.
- The area must be supplied with shelves for patient folders and a cupboard.
- The patients must be clearly visible from the nurses’ station.
- There must be space for a resuscitation trolley.
- Light and good ventilation is important.
- Include a visibly positioned clock.
Minimum provision of one holding bay per theatre
Each patient-holding bay shall be a minimum of 9m².
A separate toilet is required off this area for patients.
NOTE: Children to be kept in a separate holding area, with a chair for parents accompanying the patient.
Central nurses’ station
The nurses’ station is the administrative base for the operating suite and an enquiry point for patients, staff and visitors. It provides for the coordination of patient care, observation, writing up of clinical notes, entering of data into computers, and the making and receiving of phone calls. The station must accommodate nurses, a clerk and doctors’ work space. From here the nurses must be able to observe patients in both the holding and recovery areas.
Services required include:
- Four telephones
- Data points
- Hands-free wash hand basin
- Nurse call system
- Power outlets for computer points, two central monitors, computer, fax and printer
- Light panel indicating which theatres are occupied
- Indication light showing gas per theatre
- Fire panel.
Special considerations include:
- The central nurses’ station should be positioned between the holding and recovery areas and should include a large counter facing patients in both holding and recovery bays.
- The nurses’ station should allow the nurses to have a view of the entrance as well.
- Work area to be provided for nurses and doctors to fill in forms and make notes.
- Wall-mounted wipe board and pin board.
- Engraved, wall-mounted aluminium OTU diagram, indicating fire exits.
- Workstation for computer, printer, fax machine, photocopier and telephone.
- Work surface and space for filing, shelves to accommodate files and stationery, with drawers and
- cupboards.
- All surfaces must be impervious and designed for easy cleaning.
Bay – resuscitation trolley
The resuscitation trolley bay is for the supervised holding of the resuscitation trolley and equipment.
The bay size should be a minimum of 2m² and must be deep enough to allow storage of the trolley without projection into the passage. The resuscitation trolley bay must be located adjacent to the nurses’ station and elsewhere if required, with direct access to the recovery and holding areas; rapid emergency access to the trolley from this area to patient areas is essential.
Recovery area – post-operative
The recovery area is for patients to receive care post-operatively prior to transfer back to the wards, and for patients to recover from the anaesthetic outside of the operating theatre.
- Minimum provision of one (or 1.5) bays per theatre
- Minimum floor area – 12 to 16m² per bay
- Minimum wall length -3,45m
The recommended distance to the recovery area is a maximum of 65m from the operating theatres to a stage-1 recovery bay. This distance equates to a minute of travel time for the patient from the operating room to recovery, and is considered the maximum time a patient can be off fixed monitoring post-surgery
Services include:
| -Hands-free wash hand basin. | 1 per 4 bays |
| -Oxygen point | 1 per bay |
| -Suction point | 1 per bay |
| -Electrical points | 4 per bay |
| -Deep-bowl sink | 1 |
| -Lighting | See BES |
| A call/panic button | 1 per holding area |
Consider:
- Space required for resuscitation trolley.
- Light and ventilation are important.
- All trolley bays in recovery must be provided with a curtain rail for patient privacy.
- Provide an x-ray viewing box / x-ray viewing screen (digital), and facilities to screen off the patient. The recovery area shall be within the restricted access area.
- If any post-operative imaging is to be done in this area, sufficient ionic radiation protection must be available for the bay walls and curtains.
- A separate area should be provided for children and breastfeeding mothers.
Staff rest room
The staff rest room is used by the staff for rest and relaxation during tea and meal breaks, especially where it is difficult for staff to use centrally located facilities.
The staff rest room must be located away from the operating theatre area.
Size is dependent on the number of staff using the facility. Allow 1.5m² per person, with a minimum area of 25m².
Services include:
- Double-bowl sink with drainage and hot and cold water.
- Microwave oven.
- 120ℓ fridge/freezer combination.
- Plug outlets for a kettle, microwave and fridge.
- Data outlets.
Considerations:
- Provide a general staff rest room and a separate quiet staff rest area.
- Facilities for food and beverage preparation and storage should be provided.
- Lounge chairs.
- Table and chairs.
- Where possible, the staff rest room is to be shared by all staff of the OTU.
Anaesthetic induction room (optional)
"The provision of anaesthetic rooms immediately adjacent to the operating room has also become a source of controversy. In many European hospitals the provision of the anaesthetic room has been removed in favour of holding areas. This is in response to the modern-day provision of better-equipped day-surgery suites, which have removed many of the minor procedural and short theatre-time cases from the inpatient theatre suite. The anaesthetic room therefore is no longer required as a holding area and, if the premedication can be delivered at ward level, the dwell time outside the operating room can be completed elsewhere. In a patient-focused environment, however, the anaesthetic room provides a soothing environment where carers can wait with the frail elderly or the very young and provide comfort right up to the point of intubation."[2]
The provision of anaesthetic rooms (induction rooms) immediately adjacent to the operating room depends on the facility and procedure type.
The anaesthetic induction room is for holding patients on mobile beds or trolleys prior to operative procedures at times when the operating theatre is not available. Local, regional or general anaesthetics can be administered in this area.
This should be a minimum of 16m².
The anaesthetic induction room should be directly connected to the operating/procedure room and may be shared between two operating theatres or procedure rooms. The anaesthetic induction room should be located en route between the entrance of the unit and the operating room.
Services include:
- Four PLUG outlets for equipment
- Vacuum
- Medical gas
- Oxygen.
Considerations:
- A countertop for the preparation of medication and for equipment.
- Cupboards for the storage of equipment and consumables.
Storage
With the impact of technology on the operating room size, more storage areas are required to house the technology when it is not in use.
Bay – mobile equipment storage
The mobile equipment storage bay is an open storage area for one or more items of mobile equipment in frequent use by the operating theatres, and will include the following:
- A blood-warming device needs to be available to all theatres
- A fluid-warming device (preferable in the setting -up room)
- Mobile scales
- Patient-lifting devices
- Portable x-ray equipment
- Camera equipment
- Plug-point space for charging.
Storage bays shall be provided at the minimum rate of 5m² per operating theatre and with a minimum dimension of 0.8m (one metre preferred). The areas should be located directly off the main passage, or areas of use, by recessing the bay into the corridor walls.
Blood store
There shall be adequate provisions for refrigerated blood storage. This may be a blood-storage refrigerator in a dedicated room or in a shared space. The blood-storage area requires a minimum area of 5m².
The blood-storage area should be located with ready access to the OT and may be combined with a pathology room.
Services include:
- Two power outlets
- The blood refrigerator requires essential power supply.
Considerations:
- An area for preparation
- Blood warmer.
Laboratory area
This is an area for preparation and examination of frozen sections which may be provided adjacent to the operating theatre, off the clean passage.
Services and furniture include:
- Stainless steel sink
- Suction point
- 4 x plug points
- Hands-free wash hand basin with elbow action taps
- IT connection
- Telephone
- Shelf for microscope
- Under-counter cupboards with worktop and space to write notes, look into microscope, work with frozen sections.
Medical gas storage
This area is for the main storage of medical gases, which must be outside the facility and reticulated internally to gas outlets. Provision shall be made for additional separate storage of sufficient reserve gas cylinders to complete at least one day's procedures.
Store – special instruments
This area is a secure room for the storage and holding of special instruments in a clean environment.
This store requires a minimum area of 9m².
The store should be located close to the operating theatres and off the clean corridor
Considerations:
- The store should be lockable.
- Stainless steel shelving is required.
- Store rooms are best designed in an elongated rectangular shape to allow easy access to all items.
Store – pharmaceutical
This is a secure room for the storage and holding of pharmaceutical items for use in the operating theatre. The room should be located off the clean passage with a dispensing counter for the issuing of pharmaceuticals upon request from staff from the operating theatres. Pharmaceuticals from outside the OTU should be delivered to this store area through an access-controlled door that connects to the external passage.
Minimum size: 9m²
Services include:
- Data points
- Plug points for computers
- Plug points for equipment
- A clinical-wash hand basin.
Considerations:
- The store should be lockable
- Stainless steel shelving is required
- Countertops for staff to work
- A hatch between the store and the clean passage to allow requisitions to be given and for the delivery of requested pharmaceuticals for specific procedures in the operating theatres.
Store – linen
- Typical storage within the OT suite
Anaesthetic workroom
An Anaesthetic workroom may be provided for cleaning, testing and storing of anaesthesia equipment and should be located with direct access to circulation corridors and ready access to the operating theatres.
Services include:
- Sufficient power and data outlets and a medical gas panel for testing of equipment.
- A clinical hand-wash basin shall be provided within the room.
- Stainless steel wash trough with hand shower.
- Hands-free clinical wash hand basin.
Considerations:
- The anaesthetic workroom shall contain workbenches, sink(s) and racks for cylinders.
- Provisions shall be made for separate storage of clean and soiled items.
- Work top area – stainless steel.
- Provide space for anaesthetic trolleys and other anaesthesia equipment.
====Scope cleaning====[3] This space is utilised for the cleaning, disinfection, sterilisation and storage of endoscopes and accessories.
The area is divided internally into a dirty area for the cleaning of used equipment and a clean area for the storage of cleaned, reprocessed equipment.
It is good practice for scope-cleaning and sterilisation to be performed in the CSSD and not in the OTU.
The dirty-area requirements include:
- The dirty area to be equipped with automated endoscope re-processors, with the required electrical supply and three water supplies – hot, cold and demineralised water.
- A deep-bowl stainless steel sink that is large enough to rinse and wash the endoscopes.
- A stainless steel work surface to be provided.
- Storage cupboards for special chemicals required (these are hazardous and must be handled and stored accordingly).
- Suction.
- Clinical hand-wash basin with elbow taps, soap dispenser and hand-towel dispenser with disposal bin mounted on the wall.
- Signage to be mounted in a clearly visible spot, warning of any hazardous substances and processes and detailing procedures in the event of contamination.
- Extract ventilation at bench level is required to remove toxic vapours.
The clean area requirements include:
- Storage of personal protective equipment such as nitrate gloves, goggles, impermeable aprons and respiratory-protection equipment suitable for use when decontaminating endoscopes or mixing chemicals.
Sterile Zone
The sterile zone comprises:
- The scrub-up/gowning room
- The set-up room
- The operating theatre (OT).
These rooms are directly adjacent to each other.
Scrub-up/gowning room
Each theatre should have a scrub room. The scrub-up/gowning room provides an enclosed, dedicated area for pre-operative scrubbing, gowning and gloving prior to entering the operating theatre. It is required that all entering the operating theatre should wear surgical scrubs and surgical masks
The scrub-up/gowning room should be a minimum of 11m² per operating room (to allow sufficient space for a minimum of three people). The scrub room should be large enough to allow staff to scrub up, gown and circulate without risk of contaminating each other or contamination from the surrounding fittings.
The scrub area should be situated off the clean passage, in a separate room adjacent to, and in front of, the theatre entrance - i.e. the scrub-up area should be directly accessible from the OTU corridor and from the associated operating or procedure room.
Services include:
- The scrub area to be equipped with a double stainless steel scrub sink with elbow taps.
- Splash-limiting stainless steel basins or drainage trough.
- Hot and cold water.
- Wall-mounted clock.
Considerations:
- The activities of scrubbing and gowning/gloving should be separate within the space.
- Taps should be non-touch – automatically operated or foot operated.
- Taps should be high enough so that hands and elbows can be washed and rinsed under the taps.
- Taps must be able to be operated with elbow action.
- Provide shelves for replacement gowns, gloves, head cover and foot covers.
- Provide adequate space to gown.
- Antiseptic hand-washing liquid dispensers should be fixed to the wall above the scrub sinks. These should be elbow-action dispensers.
- The scrub sink and taps should be at a height that facilitates hand- and arm-washing.
- The design of the drainage must ensure that the floor does not become wet during scrub-up procedures.
- The floors must be anti-slip.
- Wall-mounted paper towels to be provided.
- Wall-mounted glove dispensers to be provided.
- Space for floor disposal bins that are foot-operated.
- The door between the scrub and theatre should be an automatic self-closing door (however, a door is not essential between the theatre and the scrub room unless the scrub is shared between two theatres).
- Splash-back to the sink to be a solid waterproof panel.
The example image above shows an installation where the scrub area is included in the common-use theatre passage. While this appears to be an appealing and economical design, it presents a potential infection-control risk. The common-use passage is not normally served by the same class of ventilation, does not enjoy the same hygienic finishes as the theatre, and is not validated as an aseptic area. This arrangement also removes the clean transition zone between common-use areas and the aseptic theatre environment. Staff are forced to enter and leave the theatre through the main theatre door during surgical cases, thus disrupting the aseptic environment established in theatre while in operation.
Set up/Setting out/Preparation
The set-up room is the clean workroom in the OTU where clean or sterile materials are held and arranged prior to use in the operating theatres. Instrument packs and other sterile packs required for the day surgery are delivered to the set-up room from CSSD. Here the scrub nurse will set up for a procedure, before the full surgical team are present, opening sterile items and instrument packs on trolleys to check that all the required equipment is present and sterile.
Each theatre should have a set-up room which is outside but adjacent to the operating theatre, and which has direct access to the operating theatre. Sharing of one set-up room between two operating theatres is acceptable, provided the layout and size of the room facilitates such sharing.
Set-up rooms may be combined with the sterile stock store with direct access to the operating theatre.
A minimum of 12m² per operating room (or 20m² where one set-up room is shared between two operating rooms) should be provided. Larger set-up rooms are required for operating rooms where organ-transplant surgery and orthopaedic surgery take place (more trolleys are required to be set up prior to operating).
The main functions for which facilities shall be provided are:
- Setting up of instruments and packs on trolleys prior to a procedure.
- Storage of sterile packs, instruments and materials to be used in the operating theatre.
- Holding of sterile supplies and packs.
- Storage of lotions in a special-purpose warming cabinet.
- Preparation of dressing and instrument trolleys.
- Storage of drugs, including scheduled drugs.
Considerations:
- This is a sterile area and should not be accessed by people not in full theatre attire.
- Space is required for assembly of trolleys prior to delivery to the operating room.
- The set-up room shall be positively pressured relative to adjoining rooms.
- Any worktop areas should be stainless steel.
- Doors into the theatre must be automated.
- Storage and suitable work surfaces.
- Doors in and out of the set-up room must be large enough to allow instrument trolleys fully set out to pass through without being contaminated.
- Work surfaces to be high enough to store 870mm-high trolleys beneath.
Operating Theatres (Sterile Zone)
The operating theatre (OT) is central to the operating-theatre unit.
Essential principles of design for operating theatres
The OT is a specialised facility within the hospital where lifesaving or life-improving procedures are carried out on the human body by invasive or minimally invasive methods under strict aseptic conditions in a controlled environment, by specially trained personnel, to promote healing and cure with maximum safety, comfort and economy. It is imperative that OTs are designed scientifically to ensure sterility, easy maintenance and effective utilisation
All aspects of the theatre must be focused on maintaining the concentration of the operating surgeon and team during the operation.
The standardisation of theatre layouts within an OTU will offer great value to the performance and efficiency of the theatre staff. Mirroring theatre layouts in order to economise on space usage is therefore not recommended.
Infection prevention and control within the theatre
This section serves to outline a few critical aspects of infection prevention and control as they pertain to surgery facilities. For a more detailed review of IPC measures and practices, the reader is urged to refer to the IUSS Health Facility Guide: Infection Prevention and Control.
The following direct contact routes for surgical-site infection are identified as:
- Instruments
- Surgical Instruments are at risk of being contaminated prior to or during procedures by both contact and airborne routes. These contaminated instruments are considered to be a primary source of contact infection.
- Consumables
- Consumables are similarly at risk of becoming themselves contaminated, before being the agent by which contact contamination occurs.
- Utilities
- Utilities which are re-usable between procedures, and which may even be shared during simultaneous procedures, can harbour or transmit infection.
- Fixed room and equipment surfaces
- These surfaces shall be able to withstand the rigors of the regular cleaning and disinfection regimen prior to each invasive procedure.
- Theatre staff
- Theatre staff are a major source of infectious particles and for this reason theatre practice, gowning and etiquette is of critical importance in reducing incidences of surgical-site infections.
Airborne contamination can have the following sources:
- Theatre staff
- It is estimated that a person walking can liberate as many as 5 000 bacteria per minute (Kowalski & Bahnfleth, 1998). Many of these particles can remain suspended in the air currents for extended periods and therefore have a great potential for surgical-site infection.
- Ventilation systems
- Inadequately designed or maintained ventilation systems can harbour, generate, liberate and distribute airborne contaminants widely. Well-designed ventilation systems can suppress, control and dilute airborne contaminants.
- Environmental
- Airborne environmental contaminants are generally kept out of the surgery facility by the ventilation system. Where ventilation systems fail or are inadequate, viable and non-viable contaminants can enter the surgery facility and contaminate staff, equipment and the wound site directly.
- Surgical-site infections
- Surgical-site infections result in a higher healthcare burden. It is estimated that surgical-site infections (SSI) double the cost of treatment through length of stay (LOS) alone. This estimate excludes re-admissions
Space separation and differentiation within the operating theatre:[1]
Surgical procedures pose a risk of infection to the patient, necessitating that the space to perform these procedures be carefully planned accordingly. These procedures should occur in areas which must provide adequate space to accommodate the patient, the surgical team while performing the procedure, and the equipment required for the procedure. The set-up of an operating theatre is primarily influenced by the aseptic principles that have to be applied.
In order to maintain good aseptic principles it is essential to divide the areas in and around the operating theatre into three working areas:
- The core or centre of the operating theatre/room is where the patient is situated and where the procedure is performed.
- The “sterile” circle is the area directly around the patient where the scrub nurses and surgeon(s) performing the procedure, using sterile instruments, stand and work. It includes any theatre staff directly involved in the procedure who are wearing sterile surgical attire, the operating table, other accessory equipment and any furniture that is covered with sterile drapes, such as trolleys and stands.
- The unsterile area is where associated support staff (i.e. the anaesthetist, circulating nurse and students, etc.) are performing their duties within the operating theatre. While assisting “sterile” personnel, unsterile personnel must remain in the unsterile area and avoid crossing into or between sterile areas. They supply items to the scrub team attending the patient, move equipment around the theatre into place and monitor patient progress.
Generally, equipment, trolleys and members of the surgical team are on either side of the table, while the anaesthetic team and anaesthesia equipment is at the head of the table.
- Space separation and differentiation within the operating theatre
The equipment, supplies and people working within the immediate surgical field around the patient on the operating table (a 4m x4m envelope) are the area of greatest concern for infection control in the surgical environment. A carefully orchestrated workflow in, out of and within the operating theatre, is key to minimising the risk of contamination in this cleanest of patient-care environments. Anything that moves in and out of operating rooms, as well as the surgical suite as a whole, should be subject to rigorous control.
Size and space allocation in operating theatres
- The shape of the room should be rectangular and as close to square as possible.
- The shorter side of the room should be a minimum of 80% of the longer side.
- The room should have splayed corners for ease of cleaning. The ventilation return/extraction duct is commonly placed behind the splayed corner.
- Space allocation must be large enough for correct techniques and small enough to minimise unnecessary movements of personnel, patients and supplies.
- The speed of the development of technology has had, and will have in future, significant implications for the design of OTs. “The challenge for planners and architects is to design surgical facilities that are not only functional but have sufficient flexibility to adapt to the changes and rapid developments in surgical technology“ [3]
- Size is very dependent on the equipment to be utilised within the OT. Anaesthetic machines, for example, have increased in size due to the number and complexity of the integral patient-monitoring systems.
Operating theatre sizes
| THEATRE | AREA | COMMENT |
| Minor procedure | 20- 36 m² | |
| General surgery | 40 m² | |
| Ophthalmology | 40 m² | May need to accommodate a ceiling fixed or mobile microscope. |
| Burns | 40 m² | |
| Cath lab | 49m² | |
| Digital theatre | 49 m² | |
| ENT and scopes | 49 m² | May need to accommodate a ceiling-fixed or mobile microscope |
| General endoscopy | 55 m² | |
| Urology & plastics | 55 m² | |
| Cardiothoracic | 55 m² | May have to accommodate extra equipment like the heart-lung machine. |
| Orthopaedic | 60 m² | Needs to accommodate x-ray image intensifier, different tables - e.g. fracture tables |
| Trauma | 49 m² | |
| Neurosurgery & spinal | 60 m² | May need to accommodate a ceiling-fixed or mobile microscope. |
The provision of multipurpose operating rooms can be considered to give flexibility in booking cases to any operating room. This generally means operating rooms of around 55m² to cater for a variety of equipment that now accompanies many of the general procedures.
Advantages of a standard theatre size include the following:[3]
- Flexibility, as a variety of surgical procedures can be performed in the same size of theatre, which leads to better utilisation of the theatre and less downtime.
- Both minimal and open surgery can be undertaken in the same theatre space.
- Orthopaedic surgery requires as many as seven trolleys for different sets of instruments during surgery, and requires a larger space to accommodate the additional items.
- In a number of facilities, patients are transferred from the theatre table to their beds. Beds are larger than the traditional trolleys and require more space to manoeuvre within the operating theatre.
Finishes and fixtures
Ceilings
Ceilings in the operating theatres should be smooth and monolithic. The surface finish must be washable and completely sealed. While a solid concrete slab is preferred, with services directly above the slab, this is not always possible - which results in a suspended ceiling with a ceiling void above. This requires access panels to be fitted to the ceiling and should be the sealable type. The ceiling void must be deep enough to allow maintenance to be carried out on equipment above the ceiling.
While acoustically absorbent ceiling finishes reduce noise, it is essential that infection risks are minimised and only smooth, easily washable surface finishes are applied to the ceiling soffit.
Walls
Walls in the operating theatre must be smooth, impervious, durable, washable and easily cleanable. Added protection needs to be applied in areas where damage to the surface of the wall is more likely.
Floors
Floors in the operating theatre have to be particularly hardwearing and durable, as they are subject to:
- machinery loads as equipment is pushed back and forth throughout the unit and stored or utilised in the theatres;
- Frequent washing and scrubbing, as cleanliness is critical and decontaminating the theatres after each operation is critical for infection-control purposes; and
- spillages, which occur during most operations; consequently floor finishes must be easily washable, stain-resistant and sustainable.
It is therefore important that floors finishes are:
- Slip-resistant
- Continuous with sealed joints at junctions
- Smooth
- Impervious
- Easily washable
- Wear resistant
- Hygienic.
Skirtings should be coved and should rise 100mm up the wall. Best practice is to have a continuous floor finish that continues up the wall with no joint between the floor and the skirting. This allows for easy cleaning and discourages microbial colonisation.
The fixing of the floor finish to the underlying screed must be carefully carried out to the manufacturer’s specification to ensure good adhesion and so that the floor will withstand the heavy loads anticipated.
Where the theatre is under “laminar flow”, the floor directly below the airflow hood should be a different colour, so that staff can differentiate the area covered by the hood within which the sterile trolleys must be kept, and where key staff should remain during the operation.
It is useful to also demarcate with different colours floor areas where essential equipment needs to be always placed - e.g. the emergency trolley.
Doors and door frames
Doors and frames need to be durable and able to withstand frequent impact from mobile equipment. Solid-core doors must be used.
Where glazed panels are fitted to the theatre doors, these should be opaque to protect patient privacy.
Automatic door openers that are foot- or elbow-operated should be fitted to the entrance doors to the theatre.
Since the main entrance to theatres isn’t through an anteroom, the operation of this door during operations can severely affect the integrity of the clean zone established in the theatre. While the presence of sliding doors in theatres presents a concealed mechanism which is virtually un-cleanable, and does not provide an adequate seal to assist with contamination control, swing doors also present a plethora of additional problems. The surge of air from swinging doors in theatres could disrupt the ultra-clean zone around the operating table, and the use of swinging doors in theatres with unidirectional airflow (UDAF) or laminar flow should be applied with caution. Sliding doors, when used, should be installed such that the door mechanism is not within the operating-theatre room.
Windows
Windows in the OTU should be weather-tight, durable, washable, and easily accessible for cleaning and maintenance.
Windows should have blinds installed which enable the OTU to be darkened as appropriate. These must be washable and easily maintained and of a material that does not encourage microbial colonisation. The positioning of windows is critical within the OTU, and should prevent glare, ensure maximum user comfort, provide views out while protecting internal privacy. See paragraph 5.4.3 “Views” for more information.
Music
Many theatre staff insist on music in theatres. For this reason it is advisable to install a CD player or AV receiver in the theatre panel, or at a similar discreet location. Where music players are permanently installed in theatres, their controls should be flush with the panel. AV receivers should not be limited to propriety hardware interfaces, but should accept multiple device types. A suitable consideration would be a wireless Bluetooth receiver supporting easy pairing with universal remote audio and volume controls. This would permit staff to bring their own portable media players and playlists for use with the system.
Lighting
Good lighting levels and quality are essential in operating theatres. In addition to irradiance, colour rendering and evenness are important factors. For details of lighting requirements for surgeries the reader is referred to building engineering services
Computer equipment
Digital display of imaging results should be available to the surgeon at the operating table. For this purpose a display panel should be provided on a movable or retractable pendant. The inclusion of a conventional keyboard and mouse is not recommended. Should the imaging display system require a user interface, a de-contaminable touch interface is recommended.
Swab-count board
Theatre policy requires safe checking and counting of swabs, needles and instruments before, periodically during, and after each case. This process requires the use of containers for used or contaminated swabs, and a count board and swabs will remain in the theatre throughout the case.
For this reason, a swab-count board should be accommodated in the theatre-layout planning. The swab-count board could include the stand with bins and racks to facilitate the counting and control of swabs and instruments.
Theatre warning light
A visual alarm panel should be included in the theatre. This panel should give an indication of any critical engineering system failure, such as ventilation or medical gases. Alarms to this panel should also be relayed to the nurses’ station and engineering office. Non-critical alarms should be relayed only to the engineering office and nurses’ station as necessary. The theatre alarm panel should also give a visual indication of the theatre temperature. For information the reader is referred to the Building engineering services
Theatre types
The general-surgery operating theatre
This operating theatre provides an aseptic environment in which to carry out surgical procedures under local, regional, general anaesthetic or sedation.
- The general-surgery operating theatre is located within the operating unit and away from through-traffic.
- Direct access is required to the holding bay/anaesthetic room, scrub room, exit bay/circulation corridor.
- Ready access is required to recovery, clean-up areas, sterilising bay, sterile store and CSSD.
Staff Contingent And Locations
The surgeon normally stands on the patient’s right-hand side if it is open surgery; however, in the case of laparoscopic surgery the position varies. The surgeon may stand at the foot end of the table.
The scrub person stands opposite the surgeon, with the assistant surgeon.
The anaesthetist and assistant will be at the head of the theatre table.
The circulating person will be at any area that makes it easy to work in close proximity to the scrub team.
Overhead Services
Overhead services should include one central ceiling-mounted, dual-luminaire theatre light that should be securely fixed above the operating table.
Also, two services pendants, one for surgical and one for anaesthetic use, are to be securely fixed to the ceiling. These pendants shall be positioned such that they are readily accessible to either the surgeon or the anaesthetist, as appropriate. Retractable pendants shall be designed such that they accommodate the ergonomics of even the most diminutive nursing staff.
| General theatre services | Anaesthetic pendant | Surgical pendant |
| 230V socket outlets and connection to the UPS systems | 6 | 6 |
| Oxygen | 2 | - |
| Medical vacuum points | 2 | 2 |
| Low-pressure medical air | 1 | 1 |
| Nitrous oxide | 1 | - |
| Anaesthetic gas-scavenging points | 1 | - |
| High-pressure medical air | - | 2 |
Wall-Mounted Services
A wall-mounted control panel is commonly provided and should include the following services:
- Radio or AV receiver
- Clock and stop-clock
- Telephone
- Sterile touch-screen-controlled computer
- Temperature controller
- The control panel could have a conventional x-ray viewing box or a 42” LCD screen (this may be on a fixture suspended from the ceiling.
A swab board shall be mounted on one wall.
An indicator light is required outside the entrance of the theatre to indicate whether the theatre is occupied.
It is essential that at least one wall be free from door openings and services that require frequent attention. This provides a quiet area for sterile equipment and scrubbed personnel, which is not compromised by frequent traffic. It is preferable for the adjacent wall to be free, or impinged upon only for exit from the operating room.
Anaesthetic Equipment
The following anaesthetic equipment should be accommodated:
- Anaesthetic machine, with cardiac monitor
- Two or three drip stands
- Equipment positioning for endoscopic surgery
- Trolley with the anaesthetic-induction and -reversal drugs
- Trolley for the anaesthetist to work on
- Suction apparatus - may or may not be part of anaesthetic machine
- Records / computer to record patient data
- Waste-sharps container
- Chair.
Surgical Equipment
The following surgical equipment should be accommodated:
- Digital display and recording system for patient’s records
- Two infusion pumps
- Three syringe pumps
- Blood warmer
- Feeding pump
- Operating table
- Suction apparatus
- Two kick-abouts
- Three to four instrument trolleys
- Three basin stands
- Mayo stand or table
- Diathermy machine
- Two small trolleys
- 1 for the catheter
- 1 for the telescope warmer
- Two endoscopy carts with the camera system, video, light source and insufflators
- Equipment monitors for specialised equipment
- Writing worktop, with drawers for nursing staff
- Four chairs
- Sharps container
- Emergency call system.
Additional Considerations
- The scrub area and setting-up area may be shared by two adjacent theatres.
- The use of automatic, foot-operated, sliding doors for all theatre entrances is recommended.
- Passive infrared proximity sensors are not appropriate for activating theatre doors.
- An emergency call button linked to the sister’s office should be accessible from within the theatres.
- All theatre electrical services should be on emergency backup supply. This includes a UPS and generator.
The Obstetrics Operating Theatre
This theatre is principally the same as a general theatre, save for the wall panel which includes services for two new-borns.
This should include two separate sets in the panel, each with:
- Oxygen
- Vacuum
- Medical air
- Six plugs.
Two baby-resuscitation stations are to be located permanently adjacent to the theatre’s wall service panel.
The Orthopaedics Operating Theatre: – Ultraclean / Laminar-flow
This theatre is principally the same as a general theatre, but orthopaedic units generally have a higher demand for space for personnel, storage and set up.
Personnel Required In the Theatre
- Surgeon
- One or two assistant surgeons
- Scrub person - can be one or sometimes two
- The circulating person
- Anaesthetist
- Anaesthetic nurse or assistant
- Possible additions:
- students
- medical reps
The surgeon normally stands on the patient’s left-hand side or, depending on the type of surgery he will be doing, in another position. If it is surgery of the extremities, he will stand on the side to be operated on.
The assistant surgeon stands opposite the surgeon, next to the scrub person.
The circulating person is at the bottom and side of the table, and looks after the scrub team.
The scrub person stands opposite the surgeon, with the assistant surgeon.
The anaesthetist and assistant will be at the head of the theatre table.
Overhead Services
Overhead services should include one central ceiling-mounted, dual-luminaire theatre light that should be securely fixed above the operating table.
Also, two services pendants, one for surgical and one for anaesthetic use, are to be securely fixed to the ceiling. These pendants shall be positioned such that they are readily accessible to either the surgeon or the anaesthetist, as appropriate. Retractable pendants shall be designed such that they accommodate the ergonomics of even the most diminutive nursing staff.
| General theatre services | Anaesthetic pendant | Surgical pendant |
| 230V socket outlets and connection to the UPS systems | 6 | 8 |
| Oxygen | 2 | - |
| Medical vacuum points | 2 | 2 |
| Low-pressure medical air | 1 | 1 |
| Nitrous oxide | 1 | - |
| Anaesthetic-gas scavenging points | 1 | - |
| High-pressure medical air | - | 2 |
Anaesthetic, wall-mounted and surgical equipment accommodation considerations are principally the same as for general theatres.
Unidirectional Airflow/ Laminar-Flow Plenums
- The plenum shall be fitted to the ceiling in the middle of the theatre.
- All metal work on the laminar flow unit shall be stainless steel or baked epoxy-coated mild steel.
- HEPA filters shall be terminally mounted at the unidirectional-airflow (UDAF) plenum.
- The UDAF screen shall be hinged such that the lighting and HEPA filters are serviceable from within the theatre.
- HEPA filters shall be removable into the theatre for testing and replacement. This protects the theatre from being directly exposed to the service-space environment during HEPA filter changes.
- The UDAF plenum shall include sealable upstream sampling ports for in situ filter-efficiency testing.
- The UDAF plenum shall include concealed lighting to achieve the required background lighting levels and quality.
Equipment
The equipment required in an orthopaedic theatre is similar to that of a general theatre, although the equipment trolleys are larger and more numerous to accommodate the specialist equipment. There may be as many as seven equipment trolleys for certain procedures.
Additional Considerations
The “Plaster of Paris” or POP store room should be adjacent to the theatre and should include a stainless steel sink with hot and cold water and storage space for materials.
The cardiothoracic operating theatre
This theatre is principally the same as a general theatre, with the following considerations:
Personnel Required In the Theatre
- Surgeon
- One or two assistant surgeons
- One or two scrub persons
- One or two anaesthetists
- One or two anaesthetic assistants or nurses
- One circulating person
- Perfusionist.
The surgeon stands on the patient’s right-hand side during the procedure.
The assistant stands opposite the surgeon.
If there are two assistants, the other one will stand on the surgeon’s side, opposite the scrub person.
The scrub person stands next to the assistant surgeon, opposite the surgeon.
The anaesthetist is always at the top end of the operating table.
The anaesthetic nurse or assistant will be in close proximity to the anaesthetist at all times.
The perfusionist sits behind the surgeon, next to the heart-lung machine.
Overhead Services
The overhead services required are similar to that of a general theatre.
Anaesthetic Equipment
The following anaesthetic equipment should be accommodated:
- Anaesthetic machine, with cardiac monitor
- Two or three drip stands
- Small trolley for insertion of lines like the CVP, arterial line (ideal in induction room)
- Trolley with the anaesthetic induction and reversal drugs
- Trolley for the anaesthetist to work on
- Suction apparatus-may or may not be part of anaesthetic machine
- Records / computer to record patient data
- Monitors
- Infusion pumps
- Waste-sharps container
- Chair.
Surgical Equipment
The following surgical equipment should be accommodated:
- Operating table
- Three to four surgical instrument trolleys
- Small trolleys for insertion of a urinary catheter
- Basin stands - two or three
- Two kick-abouts
- Mayo stand or table
- Suction apparatus
- Three basin stands
- Mayo stand or table
- Diathermy machine
- Two small trolleys
- 1 for the catheter
- 1 for the telescope warmer
- Defibrillator machine
- Drip stand with sternal saw motor
- Special operating table which can be adjusted to any position needed
- More than one suction apparatus
- Four chairs
- Sharps container
- Emergency call system.
Perfusionist Equipment
The following perfusionist equipment should be accommodated:
- Heart-lung machine
- Heater/cooler machine
- Intra-aortic balloon pump
- Arterial blood gas machine
- Ice machine (outside OR)
The heat load of the perfusionist’s equipment (heart-lung machine, inter alia) must be considered.
The Neurosurgery Operating Theatre
This theatre is principally the same as a general theatre, save for the following considerations:
Personnel Required in the Theatre
- Surgeon
- One or two assistant surgeons
- One scrub person
- One anaesthetist
- One anaesthetic assistant or nurse
- One circulating person.
The surgeon and assistant stand at the head of the table.
The anaesthetist and anaesthetic machine will be at the side or at the foot end of the table.
The scrub person stands either between the surgeon and assistant, or on the right-hand side of the patient.
The circulating person is next to the sterile team, at the head end of the table.
The anaesthetic nurse or assistant will be in close proximity to the anaesthetist.
Overhead Services
Overhead services should include one central ceiling-mounted, dual-luminaire theatre light that should be securely fixed above the operating table.
Also, two services pendants, one for surgical and one for anaesthetic use, are to be securely fixed to the ceiling. These pendants shall be positioned such that they are readily accessible to either the surgeon or the anaesthetist, as appropriate. Retractable pendants shall be designed such that they accommodate the ergonomics of even the most diminutive nursing staff.
| General theatre services | Anaesthetic pendant | Surgical pendant |
| 230V socket outlets and connection to the UPS systems | 6 | 8 |
| Oxygen | 2 | - |
| Medical vacuum points | 2 | 2 |
| Low-pressure medical air | 1 | 1 |
| Nitrous oxide | 1 | - |
| Anaesthetic-gas scavenging points | 1 | - |
| High-pressure medical air | - | 2 |
Consider that since the surgeon is at the head of the patient and the anaesthetist moves to the side of the patient, the anaesthetic pendant should be located to the side (side of the patient’s head).
Wall-Mounted Services
The wall-mounted services required for this type of theatre are principally the same as for a general theatre.
Anaesthetic Equipment
The aesthetic equipment space requirements are principally the same as for a general theatre.
Surgical Equipment
The following surgical equipment should be accommodated:
- Operating table
- Two or three surgical instrument trolleys
- Suction apparatus
- Two or three basin stands
- Small trolley with shaving equipment
- Small trolley for inserting the urinary catheter
- Mayo stand or table
- Operating microscope
- Ultrasonic surgical aspirator-for tumours
- Head rests like the Mayfield and the horseshoe
- Special operating table that can be adjusted to suit the particular procedure
- Two suction machines or apparatus
- Diathermy machine with both bipolar and monopolar settings.
Additional Considerations
The surgical equipment utilised in this type of theatre can be highly sensitive to vibration. The theatre should therefore be appropriately isolated from vibration. Refer to the equipment installation requirements for acceptable limits.
The Ophthalmology Theatre
This theatre is principally the same as a general theatre, save for the following considerations:
Staffing Requirements
Consider that the surgeon is at the head and the anaesthetist moves to the side of the patient; therefore the anaesthetic pendant is to the side (side of patient’s head).
Overhead Services
This theatre requires ceiling-mounted scopes. This demands that the ceiling structure be sufficiently supported to carry the additional load.
Additional Considerations
The surgical equipment utilised in this type of theatre can be highly sensitive to vibration. The theatre should therefore be appropriately isolated from vibration. Refer to the equipment installation requirements for acceptable limits.
The following additional features need to be accommodated in the setting-up room:
- Washing and cleaning area for instruments.
- Storage space.
- Flash sterilisers are often requested for emergency sterilising of dropped utensils. This solution is not recommended, as these can create an additional maintenance and operational burden and risk. In addition, the responsibility of equipment sterilisation then shifts away from the CSSD to the theatre staff. It is recommended that the capacity for emergency sterilising is incorporated into the CSSD to ensure proper sterilisation processes are followed. The implementation of flash sterilisers as a convenience to supplant good operational planning is therefore not acceptable.
The Urology Theatre
This theatre is principally the same as a general theatre, save for the following considerations:
Additional Considerations
The surgical equipment utilised in this type of theatre can be highly sensitive to vibration. The theatre should therefore be appropriately isolated from vibration. Refer to the equipment installation requirements for acceptable limits.
Urology theatres usually function as a set of two theatres in tandem:
- The first theatre is a standard theatre.
- The adjacent theatre is used for imaging, and has a scope and x-ray table with x-ray – therefore it needs a water supply and drain to the table.
- The imaging room may require lead-lined doors for radiation protection. The hinges or sliding mechanism and closers of these doors should be designed to reliably manage the additional weight of these doors.
Where separate imaging rooms are not implemented and integrated imaging bays are used instead, the theatre architecture should incorporate ionising radiation-protective measures.
The Bronchoscopy Theatre
This theatre is principally the same as a general theatre, save for the following considerations:
A scope-cleaning room is required near or attached to the theatre. This is detailed further on in this document.
- Flash autoclaves are often requested but are not recommended, as these can create an additional maintenance and operational burden. In addition, the responsibility of equipment sterilisation then shifts away from the CSSD to the theatre staff.
- A clean, ventilated storage cupboard is required for the drying and storing of scopes.
Since bronchoscopy theatres present a very high risk for airborne infection, these theatres should be maintained at a relative negative pressure with high ventilation rates. Recirculation ventilation is not recommended for these theatres; instead full fresh-air exhausted ventilation systems are recommended with special consideration for the control of contaminated exhaust discharge. The three elements of control are direction, dilution, and disinfection.
The Paediatric Operating Theatre
- This theatre is principally the same as a general theatre, save for the following considerations:
- Consideration should be given to creating a warm welcoming environment for paediatric theatres.
- Waiting areas should be provided for mothers and family.
- OT tables shall not be fixed.
- Independent temperature control is required to reduce the risk of mortality in paediatric care.
- The temperature range for paediatric theatres and induction rooms should be between 18°C and 28°C.
Context Consideration
- Paediatric theatre caseloads will vary from institution to institution and may be as high as 20-25%.
- Paediatric theatre cases treated within district hospitals should be limited to children over four years of age or 10kg.
The Burns Theatre
This theatre is principally the same as a general theatre, save for the following considerations:
- The operating table should facilitate waste-water management during patient washing.
- Floor drains are not recommended within theatres as these can present a conduit for cross-infection between procedures and theatres.
- Two hoses should be available for patient wash.
- Temperature range = 22-28°C.
- Humidity range = 45-60% RH.
- Temperature and humidity display is required at the theatre control panel.
Digital Operating Theatres
Most modern theatres can be termed digital theatres as they now use digital imagery during surgery. An effective implementation of digital technology in theatres requires consideration of the following questions in planning:
- Which surgical team member needs to see what, and at what stage?
- Where are the images being recorded from, and where do they get recorded to?
- Is imaging equipment constantly used in the theatre for procedures?
- If not, then mobile units could be considered.
- Fixed or ceiling-mounted equipment could become an obstruction if it is not continuously utilised in the theatre in question.
Day-surgery unit
"Day-surgery units are defined as “self-contained, dedicated units, suitable for carrying out surgical procedures and treatments on adult and child patients whose discharge is planned for the same day as their admission"[4]
Day-care services mainly include day surgery, endoscopy, and medical investigation and treatment. Provision of a large theatre size is preferable to accommodate a variety of surgical procedures. The infrastructural requirements for a day-surgery unit theatre are principally the same as that of a general theatre.
Planning considerations
Design of the facility should accommodate the sequence outlined below, such that the patient progresses in one direction through the unit. Principal routes should be designed to minimise clashes between patients and services.
Patient-related activities occur in the following sequence:
- entering the unit
- reception and waiting
- pre-admission and assessment
- pre-operative preparation
- operation/procedure
- post-anaesthesia recovery
- pre-discharge recovery and care
- discharge and exit of the unit
- transfer to a larger theatre to accommodate scopes..
Privacy is essential. Men and women should be attended to in separate areas, and children must be kept separate from adult patients. Continuous observation by the nursing staff is crucial.
Location
Day-theatre units should preferably be close to the OPD or adjacent to the theatres where the day theatre can share services with the main theatre unit.
Accommodation Requirements:
| Room | Standard | Non-standard | Comments | Location |
| Entrance to day unit | ||||
| Entrance | x | Refer to Item 9.1 | Entrance | |
| Waiting area with play area | x | |||
| Reception | x | |||
| Pre-operative area | ||||
| Pre-admission assessment room | x | Consulting room configuration | Adjacent to waiting area | |
| Change rooms for male patients | x | Change room area | Adjacent to assessment room | |
| Change rooms for female patients | X | |||
| Patient locker area | x | Adjacent to change areas | ||
| Male patient toilets and shower | x | |||
| Female patient toilet and shower | x | |||
| Admissions room | ||||
| Nurses’ station | x | Focal point within the pre-operative area | Adjacent to patient changing rooms, admissions rooms and patient sub-waiting areas. | |
| Operating Theatre suite | ||||
| Pre-operative nurses base | x | Pre-operative area in theatre | Theatre area which may be separate to the main theatre block or attached to the main theatre block in the hospital. This should also be adjacent to the day ward area - pre- and post-op. | |
| Pre-operative holding area | x | |||
| Anaesthesia room | x | Theatre unit (refer to IUSS document re operating theatres) | ||
| Scrub-up and gowning | x | |||
| Operating room | x | |||
| Set-up room | x | |||
| Mobile x-ray equipment bay | x | |||
| Post-operative recovery room | x | Post-operative area | ||
| Post-operative nurses’ station | x | |||
| Sluice room | x | Support services off theatre passage | ||
| Scope cleaning room | x | |||
| Equipment store | x | |||
| Dirty utility | x | |||
| Surgical store | x | |||
| Medicine cupboard | x | |||
| Equipment service room | x | |||
| Medical gas cylinder store | x | |||
| Wheelchair/trolley park bays | x | |||
| Anaesthetic-gas scavenging | x | |||
| Post-operative recovery area | ||||
| Pre-discharge recovery area - trolleys | Adjacent to the nurses’ station | |||
| Pre-discharge recovery area - chairs | ||||
| Pre-discharge recovery area – nurses’ base | x | Adjacent to
pre-discharge recovery area | ||
| Patient toilet (to accommodate a patient in a wheelchair) | x | |||
| Clean utility | x | |||
| Shared support areas | ||||
| Dirty utility | x | Located between pre-op, post-operative recovery and pre-discharge areas | ||
| Sluice | x | |||
| Cleaners’ room | x | |||
| Sterile pack store | x | |||
| Equipment store | x | |||
| Clean linen store | x | |||
| *Or central store | x | |||
| Crutches and splint store | x | |||
| Switch room | x | |||
| Staff facilities | ||||
| Staff change for theatre - female | x | A separate staff area closely situated to the theatres | ||
| Staff change for theatre - male | x | |||
| Staff toilet female | x | |||
| Staff toilet male | x | |||
| Staff locker area | x | |||
| Staff room | x | |||
| Seminar room | x | |||
| Administration | ||||
| Unit manager’s office | x | Adjacent to the theatres | ||
| Sister’s office | x | |||
IT Requirements
It is important that the design team understand the intra-dependencies of all the services within the OTU early during the design process. This includes collating and analysing the extensive information regarding the following equipment and services:
- medical gases
- oxygen and air
- suction
- data cables and data equipment
- surgical equipment.
These interdependencies will inform the IT requirements that need to be planned for. This is especially relevant in theatres where ready access to diagnostic imagery is used to assist in, and assess, procedural progress.
The incorporation of real-time imaging provided by MRI or CT-scanning during neurosurgical, cardiovascular or orthopaedic surgery demands larger operating rooms. In many tertiary hospitals specialised operating rooms of 65-80m2 are in evidence.
Imaging equipment capable of performing 3D rotational angiography, CT-scanning and intravascular ultrasound enable open surgery and endovascular techniques to be employed simultaneously.
The challenge to the design team exists in understanding where and how this technology is to be located and to anticipate possible clashes between this and other services and circulation that may result.
The equipment that is installed in the specialised or hybrid theatres should not impede their use in more standard cases.
Communication between operating rooms and pathology and radiology can be implemented, enabling real-time consultation with other medical experts to provide a seamless and integrated delivery of care to the patient.[2]
The use of IT and communications may now include voice-activated control of equipment and the room environment, robotic surgery, electronic patient records and CCTV for training and consultation.
Dirty Zone
The dirty zone includes the following areas:
The dirty zone includes the following areas:
- Dirty utility
- Sluice
- Wash-up areas (scopes)
- TSSU/CSSD
- Cleaner’s room
- Scope-cleaning room.
Scope-cleaning room
Washing and hanging provision is required for scopes and equipment.
Sluice
This is a standard room of a minimum of 9m² and its documentation should be read in conjunction with the IUSS generic room documentation.
The sluice in the administration zone should be adjacent to the recovery area.
The sluice provides for:
- Cleaning and holding of used equipment for collection and sterilisation elsewhere
- Disposal of clinical and other waste and soiled linen
- Testing and disposing of patient specimens
- Decontamination and storage of patient utensils such as pans, urinals and bowls.
The sluice should include the following services:
- Hand-wash basin with elbow taps and gooseneck outlet in each room with splash-back, soap dispenser and paper-towel dispenser
- Automatic bed-pan washer, in all sluices
- Stainless steel sluice sink
- Two 230V socket outlets.
Storage space for the following should be accommodated:
- Clean bed pan and urinal drying racks
- Built-in cupboard
- Two run-abouts, two-bucket system
- Soiled linen area
- Bumper rails to prevent bins marking walls
- Storage for used CSSD supplies, urine testing, detergents, urinal covers
- Space for large bins
- Shelves for wash basins and buckets.
Structure
Ceiling Void / Engineering Space
When planning the OTU, the construction of the operating room’s ceiling detail bears some consideration. The ceiling structure above the operating theatre should be safely trafficable, without interrupting the operation below.
The designer has the option of creating a reinforced concrete slab and finishing the soffit to serve as the OT ceiling. This solution offers the advantage of providing a structural component to which the lights and pendants can be fixed directly. Unfortunately this solution requires very careful detailing and planning, as larger penetrations need to be created during the construction of the slab and they consume precious vertical space.
Sufficient space should be provided for uncompromised routing of services above the operating theatre. The interstitial engineering space should provide enough room for installing and maintaining services. It is therefore helpful to allow for sufficient headroom for maintenance staff.
Alternatively, a trafficable, flush-finished, monolithic and impervious ceiling constructed below the slab offers a more efficient solution. This solution requires that special structures need to be installed to support the lights, plenums and pendants.
Where ceiling void access is to be through the ceiling itself, access through removable lights is not recommended as these inevitably become damaged. Dedicated trapdoors should be installed outside of the clean zone so that maintenance staff do not need to re-enter the clean zone after being in the ceiling.
Smooth cornice details are recommended to aid cleaning. Floated ceilings are not recommended. No effluent or waste pipes should be routed in the space directly above any theatre.
Accommodation Plans
The flexibility of this theatre design permits natural light into the operating room by the removal of the dirty corridor, which previously ran around the perimeter. Grouping operational rooms together into effective clusters enables stores and set-ups to become tailored to case types, and helps staff identify with their location. This is particularly important for large theatre floors to reduce travel times between stores and where there is little reference/orientation to outside views.
At the Gold Coast Hospital the operating rooms are positioned around a central sterile support area in clusters of eight. The operating rooms in turn were encircled by a peripheral patient transport corridor which enabled patients to see out. It is noted that in the Mackay Hospital Redevelopment the use of Case Carts enabled flexibility in the use of corridors because of the containment of used materials within the carts
User Room Requirements
Table 6: Room list for surgical facility
| ROOM | COMMENTS | STANDARD | NON-STANDARD | |
| GENERAL AREAS | ||||
| GENERAL AREAS | Administrative offices | Outside of OTU | ||
| IT Switch room and UPS | x | |||
| Meeting room - large | x | |||
| Office – Chief anaesthetist | x | |||
| Office - Chief surgeon | x | |||
| Office – Doctors | x | |||
| Office – Unit manager | x | |||
| Office – Sister | x | |||
| Doctors on call rooms with en suite ablution | x | |||
| Staff toilet | x | |||
| Education and training | ||||
| Seminar room | 20-30 places | x | ||
| Library | x | |||
| Study area | 5 places | x | ||
| Pre-entrance to operating theatre unit | ||||
| Public waiting area | Allow at least 4 chairs | x | ||
| Wheelchair accessible toilet | x | |||
| Counselling room | x | |||
| Entrance area | ||||
| Lobby | x | |||
| Porters’ base | x | |||
| Trolley park | x | |||
| Unit manager’s office | x | |||
| Reception | x | x | ||
| Bay – Personal protective equipment | x | |||
| Restricted access area | ||||
| Staff area | ||||
| Female change room with toilet & showers | x | |||
| Male change room with toilet & showers | x | |||
| OPERATING THEATRE SUITE | ||||
| CLEAN AREA | Office | x | ||
| Patient holding bays | x | |||
| Nurses’ station | x | |||
| Patient-recovery bays | x | |||
| Clean utility for recovery | x | |||
| Clean passage to operating theatres | x | |||
| Stores | ||||
| Clean linen | x | |||
| - Equipment | x | |||
| - Instruments | x | |||
| - Pharmaceutical supplies | x | |||
| - Surgical supplies | x | |||
| - Anaesthetic supplies | x | |||
| CLEAN AREA | Blood store | Or blood storage refrigerator bay | x | |
| CLEAN AREA
|
Equipment cleaning | x | ||
| Mobile equipment bays | ||||
| Emergency trolley | x | |||
| Trolley | x | |||
| Anaesthetic trolley | x | |||
| Bay for mobile x-ray | ||||
| X-ray | x | |||
| Ultrasound | x | |||
| Laboratory area | x | |||
| Medical gas store | x | |||
| Anaesthetic workroom | x | |||
| Induction room | x | |||
| Staff rest area | x | |||
|
|
Staff quiet rest area | x | ||
| Staff toilet | x | |||
| STERILE ARAES
DIRTY AREAS |
Minor operating theatre | x | ||
| Major operating theatres | x | |||
| Scrub room | Allow 3 people minimum | x | ||
| Set-up room | x | |||
| Sluice for theatres | x | |||
| DIRTY AREAS | Disposable corridor | x | ||
| Scope-cleaning room | Flexible endoscope cleaning room and store | x | ||
| Sluice for recovery | x | |||
| Dirty utility | x | |||
| Cleaners’ room | x | |||
Case Studies
![Theatre and CSSD plan (Courtesy of Mitchells Plain [District] Hospital)](/images/thumb/2/28/Theatre_and_CSSD_plan_%28Courtesy_of_Mitchells_Plain_%28District%29_Hospital%29.png/677px-Theatre_and_CSSD_plan_%28Courtesy_of_Mitchells_Plain_%28District%29_Hospital%29.png)
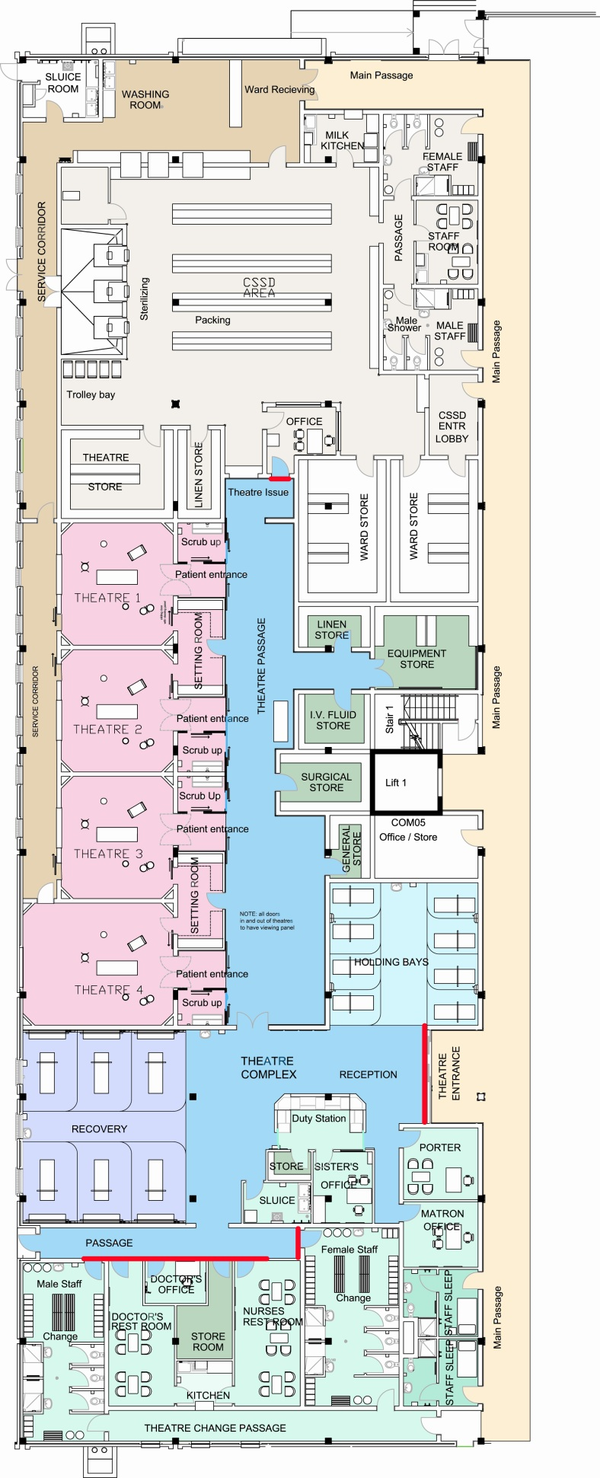
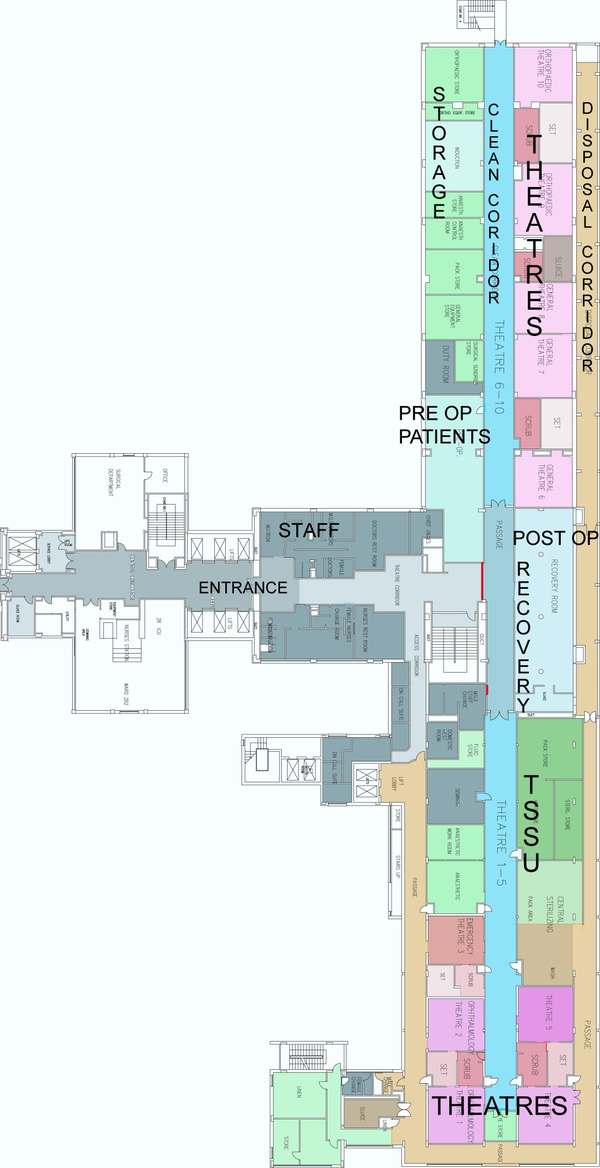
Regulations
- All local Municipal laws and regulations.
- Any other applicable Laws or Regulations.
- International Organisation for Standardisation (ISO), 2005. ISO 14644-3 Cleanrooms and associated controlled environments - Part 3: Test methods. Switzerland: ISO.
- National Health Act 2003. (c.61). Cape Town South Africa: Government Gazette.
- Regulations of the local Electricity Authority.
- South African Bureau of Standards (SABS), 1990. SANS 10400:1990 Code of practice for the application of the national building regulations. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 1993. SABS 0252-2 Code of practice Water supply and drainage for buildings Part 2: Drainage installations for buildings.Pretoria South Africa: SABS Standards Division
- South African Bureau of Standards (SABS), 1999. SANS 10313:1999 Protection of structures against lightning. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 1999. SANS 14644-1:1999 Cleanrooms and associated controlled environments Part 1: Classification of air cleanliness. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 1999. SANS 14644-1:1999 Cleanrooms and associated controlled environments - part 1: Classification of air cleanliness. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2003. SANS 10173:2003 The installation, testing and balancing of air-conditioning ductwork. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2003. SANS 14644-2:2003 Cleanrooms and associated controlled environments - part 2: Specifications for testing and monitoring to prove continued compliance with ISO 14644-1. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2003. SANS 14644-4:2003 Cleanrooms and associated controlled environments - part 4: Design, construction and start-up. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2005. SANS 10114-1:2005 Interior lighting Part 1: Artificial lighting of interiors. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2005. SANS 1238:2005 Air-conditioning ductwork. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2008. SANS 1424:2008 Filters for use in air-conditioning and general ventilation. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2008. SANS 7396-2:2008 Medical gas pipeline systems Part 2: Anaesthetic gas scavenging disposal systems. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2009. SANS 10114-2:2009 Interior lighting Part 2: Emergency lighting. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2009. SANS 10142-1:2008 The wiring of premises part 1: Low-voltage installations. Pretoria South Africa: SABS Standards Division
- South African Bureau of Standards (SABS), 2009. SANS 7396-1:2009 Medical gas pipeline systems Part 1: Pipeline systems for compressed medical gases and vacuum. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2011. SANS 1453:2011 Copper tubes for medical gas and vacuum services. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2012. SANS 10142-1:2012 The wiring of premises Part 1: Low-voltage installations. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2012. SANS 10252-1:2012 Water supply and drainage for buildings part 1: Water supply installations for buildings. Pretoria South Africa: SABS Standards Division
- South African Bureau of Standards (SABS), 2012. SANS 1091:2012 National colour standard. Pretoria South Africa: SABS Standards Division.
- South African Bureau of Standards (SABS), 2013. SANS 62040-1:2013 Uninterruptible power systems (UPS) Part 1: General and safety requirements for UPS. Pretoria South Africa: SABS Standards Division.
- The Occupational Health and Safety Act 1993. (c.85). Cape Town South Africa: Government Gazette.
List of Abbreviations
| A & E | Accident and Emergency Department |
| AHU | Air- handling Unit |
| CSSD | Central Sterile Supply Department |
| EMS | Emergency Medical Services |
| HCW | High Care Ward |
| HEPA | High Efficiency Particulate Air (filter) |
| ICU | Intensive Care Unit |
| NBR | National Building Regulations SABS 0400 |
| NICU | Neonatal Intensive Care Unit |
| OT | Operating Theatre |
| OTU | Operating Theatre Unit |
| SABS | South African Bureau of Standards |
| SANS | South African National Standards |
| SSO | Switched Socket Outlet |
| UDAF | directional Air Flow |
| UPS | Uninterrupted Power Supply |
| URS | User Requirement Specification |
List of Definitions
| central hospital | means a public hospital designated by the Minister of Health to provide health services to users from more than one province. |
| health establishment | means the whole or part of a public or private institution, facility, building or place, whether for profit or not, that is operated or designed to provide inpatient or outpatient treatment, diagnostic or therapeutic interventions, nursing, rehabilitative, palliative, convalescent, preventative or other health services. |
| hospital | means a health establishment which is classified as a hospital by the Minister in terms of section 35 of the National Health Act. |
| operating room | is a room within the operating suite in which surgical or other invasive procedures can be carried out. |
| operating suite | refers to a suite of rooms within the demarcated area where surgical and other invasive procedures are carried out or where support to these procedures is provided. |
| barrier isolator | refers to a device comprising a physical film separating an operator or clinician from a work process; The work process is maintained within an isolated environment which may be held at a positive or negative pressure. |
| Central Sterile Supply Department (CSSD) | means a facility for the receiving, decontamination, preparation, packing, sterilising, storing and issuing of sterile and disinfected instruments and other reusable materials. This facility is also known as the "sterilisation and disinfection unit" (SDU). |
| cleaners' room | means a room for the storage of cleaning equipment, the drawing of clean water and the disposal of dirty water, and the washing and drying of cleaning equipment. This room may be combined with the dirty utility room. |
| clean air | means air that does not contain a considered contaminant. |
| clean utility room | means a room for the storage of sterilised packs, dressings, sterile equipment and pharmaceutical supplies respectively; this area may also be used for a set-up area for ward procedures. |
| considered contaminant | means any actual contaminant, surface or airborne, that may have a certain impact for which avoidance measures are taken. |
| cross-contamination | refers to the contamination of any zone or surface by fomites, considered particulates aerosols, biological agents, fumes or gases originating from another zone or surface. |
| cross-infection | refers to the spreading of an infection from one organism to another by cross-contamination. |
| department | means a grouping of accommodation which has a specific function within a hospital; its area includes the associated internal or departmental circulation space. |
| dirty utility room | means a room used for the collection and temporary storage of used equipment and general ward material; it can combine the activities of the sluice room, the soiled linen and waste room and the cleaners' room. |
| emergency trolley/crash cart | means a mobile cart used for the storage of all appropriate resuscitation equipment and pharmaceuticals. |
| equipment store | means a room used for the storing of monkey chains, traction kits and other general equipment. |
| fresh air | means air drawn from the outside air of a building and contamination sources. |
| high-care ward | refers to a ward for the care and management of specific types of patients requiring a minimum of eight hours of nursing care per patient day. |
| holding area | means an area or room where pre-operative patients in transit to a procedure room/theatre are identified and continuously monitored by nursing personnel. |
| induction room | means an area where patients are prepared for surgery/invasive procedures prior to being transferred to the operating theatre. |
| intensive care unit | means a unit designed, staffed and equipped for the care and management of specific patients (e.g. medical, cardiac or post-operative) requiring a minimum of twelve hours of nursing care per patient day, or for the care of a patient who requires ventilation, continuous invasive monitoring, invasive care, or who is clinically unstable and whose life is at risk. |
| main kitchen. | means a facility suitably finished and equipped for the receipt, storage and preparation of meals, special diets and beverages |
| maternity unit | means a unit where antenatal care is provided, babies are delivered and postnatal care is given to mothers and infants. |
| midwife obstetric unit (MOU) | means a maternity unit usually attached to a clinic or a community health centre (CHC), which is staffed by nursing sisters or midwives. |
| milk kitchen | means an area for the preparation of feeds for babies which must be separate from the hospital kitchen or ward kitchen; it must contain a clinical-wash hand basin. |
| mortuary | means a facility that receives, holds and allows for the identification of bodies of patients who died in the wards, theatre or casualty department, or who were dead on arrival at the facility. |
| neonatal unit | means a facility for premature and new-born babies requiring incubation, specific care and monitoring |
| nurse station | means the control point for all activities in the patient-care areas. |
| nursing unit or ward | means a unit with the facilities to accommodate patients as specified in this regulation. |
| operating room | means a room within an operating-theatre suite in which surgical or other invasive procedures are carried out. |
| operating suite | refers to rooms within the demarcated area where surgical interventions are performed or support is provided to these surgical activities; |
| patient room | means a room where the patient can be accommodated. |
| procedure room | means a room in which certain restricted procedures generally taking less than one hour can be performed without making use of general anaesthetic - e.g. endoscopies, procedures under local anaesthetic, such as suturing of lacerations, removal of skin lesions, biopsies, closed reductions and other similar procedures; may be situated outside the operating suite. |
| recovery room/area | means the section of the operating suite specially set aside for the immediate post-operative recovery, resuscitation, nursing and special care of patients, until such time as such patients are considered to have recovered sufficiently to be safely removed from the operating suite. |
| sluice room | means a room used for the emptying, cleaning and storage of bedpans and urine bottles; it can be combined with the activities of the soiled-linen and cleaners' rooms in the dirty utility room. |
| specialised area | means any clinical area rendering specialised services such as intensive care, high care, or rehabilitation, for which additional space around the patient is required. |
| soiled linen and waste room | means a room used for the collection and temporary storage of soiled linen and waste; may be combined with the dirty utility room. |
| treatment room | means a room used for the treatment of patients in the wards, containing a clinical hand-wash basin. |
| ventilation | means The process of supplying air to or removing air from a space for the purpose of controlling air contaminant levels, humidity or temperature within the space (ASHRAE Standard 62.1-2007, Section 3). |
| validation | means the method of proving and documenting that an installed system or process performs reliably as intended and required. |
| natural ventilation | means Ventilation provided by thermal, wind, or diffusion effects through doors windows or other intentional openings in the building (ASHRAE Standard 62.1-2007, Section 3). |
| ward kitchen | means the room that forms an integral part of a nursing unit or units for the preparation of snacks and beverages; it also includes the area for the heating, storage and refrigeration of meals. |
| uninterrupted power supply | means a battery system, which in the event of a normal mains supply failure will immediately provide the electrical supply for essential equipment and lighting. |
| surgical | refers to a speciality in medicine that investigates or treats disease or injury by an operative procedure. Surgical procedures involve entering the body or body cavities by incision (breaking through the skin or other areas of the body) . This may be to treat a disease or injury or to enhance body appearance or function. |
| diagnostic | refers to a variety of observations and/or tests that can be performed in order to identify a particular disease or medical problem, and to providing the supporting evidence such as the cause - e.g. various types of endoscopy, cardiac stress tests, blood tests, x-rays etc.1 |
Acknowledgements
Documents of particular reference
1. NHS Estates, 2004. HBN 26, Facilities for Surgical Procedures: Volume 1[3]
IUSS N&S task team A:15: Tobias van Reenen, Edwina Fleming, Magda Coetzer, Zane Farina, Denise Sheard, Mirinda Coertzen
Contributions at workshops:
| Department of Public Works and Transport | Western Cape |
| Edendale Hospital clinical and nursing staff | KwaZulu-Natal |
| King Edward VIII Hospital clinical and nursing staff | KwaZulu-Natal |
| King George V Hospital clinical and nursing staff | KwaZulu-Natal |
| Inkhozi Albert Luthuli Hospital clinical and nursing staff | KwaZulu-Natal |
| Department of Health Infrastructure Department | KwaZulu-Natal and Western Cape |
Hosted visits to:
• Red Cross Children’s Hospital, Cape Town
• Inkhozi Albert Luthuli Central Hospital, Durban
• King Edward Hospital, Durban
• King George V Hospital, Durban
• Edendale Hospital, Pietermaritzburg.
• Greys Hospital, Pietermaritzburg
• Lower Umfolozi War Memorial Hospital, Empangeni
• Ngwelezane Hospital, Empangeni
• Mitchells Plain Hospital, Cape Town
• Khayelitsha Hospital, Cape Town
• G. F. Jooste Hospital, Cape Town
• Worcester Hospital, Worcester
• Brits Hospital, Brits
• Waterfall Hospital, Midrand
• Royal Alexandra Hospital, Brighton
Fiona Stanley Tertiary Hospital, Perth
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 G.McDonald and D Sheard “ A Practical Guide to Decontamination in Healthcare”
- ↑ Jump up to: 2.0 2.1 Ron Bridgefoot Principal of HASSELL
- ↑ Jump up to: 3.0 3.1 3.2 3.3 Facilities for surgical procedures in acute general hospitals (HBN 26)[1]
- ↑ NHS Scotland, SHPN52 Accommodation for Day Care, 2002
- ↑ MPDH Architects in Association
- ↑ Osmond Lange Architects
- ↑ FGG Architects