Legionella Control
Section 1
Please help to expand this page. |
Section 2
THE CHAIN OF INFECTION
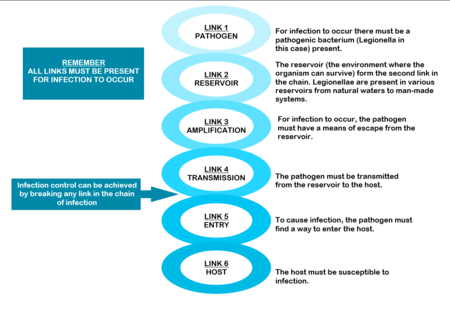
The mere presence of legionellae in a water distribution system does not necessarily imply a human health risk. For human infection to occur, certain conditions are necessary. These conditions are referred to as the “chain of infection” consisting of six links. All the links have to be present for disease to occur (Diagram: Chain of infection ). The first link, the pathogen, was discussed in Section 1.
SOURCES AND RESERVOIRS
Legionellae are natural inhabitants of water, found a wide range of habitats. They are ubiquitous in streams, lakes and rivers. They also survive in dust, soil and mud. In fact, one of the species, Legionella longbeacheae, is so often isolated from potting soil in Australia that soil has been suggested as the natural habitat of this particular species.[1]

Legionellae from these natural environments can be transmitted to man-made water systems by various means. For example, from raw water, during water treatment, as part of post-treatment after-growths within water distribution systems, during building and construction activities and during plumbing repair.[2]
Once established, they can persist in the water supply for long periods of time and are difficult to eradicate. Therefore, their presence must be considered in all aspects of the design, operation and maintenance of buildings. For this to be effective, cooperation between engineers, occupational health practitioners and microbiologists is essential.
Figure 2.3 Man-made sources of Legionella
Water sources that provide optimal conditions for Legionella growth can be separated into those containing “non-potable” and those that contain “potable” water. Non-potable water distribution systems
Heat rejection devices like cooling towers, evaporative condensers and HVAC (heating, ventilation and air-conditioning) systems are often implicated as sources of legionellosis. They contain reservoirs filled with warm, recirculating water that makes them ideal for the growth, amplification and dissemination of micro organisms (including Legionella). In a typical water-cooled system air in induced through or blown over, packing material down which water, circulating from a pond under the packing, is allowed to fall by gravity, producing a large wetted surface that cools the falling water.
The constant fall of water through the tower, the large area of the basin, fill, pipes and heat exchanger, the warm temperature of the water, the high relative humidity and high organic content within these devices provide conditions that favour contamination by algae, protozoa, fungi and bacteria. The risk is increased further by the open nature of the systems, excessive aeration and the constant addition of fresh water to make up for water lost through evaporation.
In systems that are not regularly cleaned, sludge accumulates in the reservoir and slime adheres to water covered surfaces, resulting in the presence of large concentrations of micro-organisms, including legionellae, on these surfaces. In addition, water temperatures below 60°C, the age and configuration of the system, the pH of the water and the presence of certain metals may also increase the risk of contamination.
Water derived from municipal supplies but subsequently stored in cisterns, or conditioned prior to heating, is considered non-potable due to the deterioration in chemical and bacteriological quality during storage. Colonisation of such non-potable sources inside large buildings, such as hotels, factories or hospitals, may be a major cause of legionellosis.[3][4][5]
Potable (domestic) water distribution systems
Legionellae are often present in potable water supplies, especially in the hot water sections of these systems. The organisms may enter potable water supplies from the main source, even from municipal water, and survive standard treatment protocols because most municipal water systems are not routinely screened for the presence of legionellae and the organisms are chlorine tolerant. Once inside the system, they find a suitable environment to multiply and are usually very difficult to eradicate.
Legionella levels can rise from very low to very high within short periods of time. The factors that give rise to these fluctuations are not well understood and often very hard to determine. These factors include the age and configuration of the pipes, the degree of scaling and sediment and the potential for biofilm formation within the system increase the risk of contamination. Water temperatures of 25 – 42°C, stagnation and the presence of certain free-living amoebae capable of supporting the intracellular growth of legionellae are often mentioned as amplifying factors in published reports. The biofilm and scale that form on surfaces in water distribution systems provide nutrients for legionellae and protect them from hot water and disinfectants. Some materials used in these systems, for example neoprene washers, are more readily colonised than others (Table 2.1). Building location may also play a role in the colonisation of potable water with legionellae.
Hot water tanks are often colonised with legionellae, especially at the bottom where a warm zone may develop and scale and sediment accumulate.7 Hot water piping, especially deadlegs, presents an additional risk as legionellae thrive in stagnant water.
Soil
Outdoors, the soil may be contaminated through contact with Legionella-polluted water and become a source of airborne bacteria during earth moving operations, such as construction work.
Table 2.1 Materials used in the construction of potable water lines and fixtures
|
Very good |
|
|
Good |
Other synthetic materials
|
|
Reasonable |
|
|
Not recommended |
Plastics
|
2.2 AMPLIFICATION
Legionellae are usually present in low numbers in natural sources. However, certain factors present in man-made reservoirs can promote Legionella growth and amplification. To improve our understanding of Legionella, its potential to cause disease and how to better control the organisms in water systems, we must understand these conditions. The most important factors amplifying Legionella numbers in man-made reservoirs are listed in Table 2.2.
Table 2.2 Amplifying factors for Legionella in man-made sources and reservoirs
|
TEMPERATURE |
|
|
pH |
|
|
STAGNATION |
|
|
WATER TREATMENT |
|
|
DISINFECTANTS |
|
|
CHEMICAL PARAMETERS |
|
|
RELATIVE HUMIDITY |
|
|
SLIME, ALGAE AND PROTOZOA |
|
|
CORROSION PRODUCTS |
|
|
CONSTRUCTION |
It is believed that legionellae are released from the soil during excavations from where they can enter the cooling tower of the building, air intakes or water pipes, or may be inhaled directly. Another possibility is that, during construction, nutrients already present in dust and dirt may become more readily available for the organisms. In new buildings, plumbing should be flushed before use. Renovated buildings may contain stagnant water, that should be flushed out before returning the building to normal use.
|
|
WATER PRESSURE |
|
|
BIOFILM, SCALE AND SEDIMENT |
· Legionellae have been found in biofilms forming on plastic surfaces in water piping systems. At a temperature of 40° they were shown to account for approximately 50% of the total biofilm flora; · Legionellae are less likely to be present on copper surfaces because copper generally do not support biofouling. If present, the bacteria are usually found in small numbers; · Metal plumbing components and associated corrosion products provide iron and other metals needed for Legionella, thereby supporting their survival and growth.
Algal slime also provides a stable habitat for their survival and multiplication.
|
DISINFECTANTS
After disinfection, municipal water supplies usually travel several kilometers before it reaches the point of use. During this course, disinfectant residuals diminish and there is increasing exposure to potentially biofilm-contaminated piping. Although municipal water systems are required to be disinfected at their points of distribution to conform to existing standards for bacterial disinfection, these standards are based upon the absence of coliform bacteria and do not include any specific testing requirements for Legionella.
2.3 TRANSMISSION
After growth and amplification of legionellae to potentially infectious levels, the next requirement in the chain of infection is to achieve transmission of the bacteria to a susceptible host. Modern technology like cooling towers used to recirculate water for air-conditioning and humidifying purposes and other ventilation systems can cause the formation and distribution of aerosols through which the organisms can spread. Transmission can also occur through direct installation, aspiration or ingestion (Table 2.3).
Table 2.3 Dissemination of Legionella bacteria [relook this table!]
|
AEROSOLISATION |
| |||
|
DIRECT INSTALLATION |
| |||
|
INGESTION |
| |||
|
ASPIRATION |
Never presume that you cannot get Legionnaires’ disease from drinking water containing Legionella.
|
2.4 INFECTION AND HOST SUSCEPTIBILITY
Infections caused by Legionella species are collectively known as legionellosis and include Legionnaires’ disease and Pontiac fever. Subclinical (asymptomatic) infections have been reported. Legionellosis occurs worldwide, in people of all ages and race groups, with no evidence of person-to-person spread of infection. It is most common in summer and autumn months. The incidence of legionellosis varies from country to country and from region to region. Recently, an increase in the worldwide incidence of reported legionellosis cases has become evident. This may be explained by the availability of improved diagnostic and testing methods, increased awareness of the symptoms and improved surveillance. However legionellosis, especially sporadic cases, is still not always reported to public health authorities, making it difficult to estimate its true incidence.
The mode of transmission, inoculum size, particle size and host susceptibility influence the severity of infection. Approximately half of the currently known Legionella species are implicated in disease, but L pneumophila is still considered to be the causative agent in about 80% of diagnosed cases. However, this picture might change as the number of available diagnostic tests increases – it is thus important to regard all legionellae a potentially pathogenic until proven otherwise.
References
- ↑ Dennis PJ (1993). Potable water systems: insights into control. In: Barbaree JM, Breiman RF and Dufour AP (eds). Legionella: Current status and emerging perspectives. American Society for Microbiology, Washington DC. Pp 223-225.
- ↑ Colbourne JS and Dennis PJ (1985). Distribution and persistence of Legionella in water systems. Microbiol. Sc. 2: 40-43.
- ↑ Muraca PW, Stout JE, Yu VL and Yee YC (1988). Mode of transmission of Legionella pneumophila. A critical review. Am. J. Hyg. Assoc. 49: 584-590.
- ↑ Yamamoto H, Sugiura M, Kusunoki S, Ezaki T, Ikedo M and Yabuuchi E (1992). Factors stimulating propagation of legionellae in cooling tower water. Appl. Environ. Microbiol. 58: 1394-1397
- ↑ Freije MR (1996). Legionella control in healthcare facilities: A guide for minimising risk. HC Information Resources, Inc. United States of America. P 8