Infrastructure Guidance for COVID-19/Alternate Care Sites
Return to Infrastructure Guidance for COVID-19
Infrastructure Guidance for COVID-19/Alternate Care Sites2
Infrastructure Minimum Guidelines for Alternate Care Sites for COVID-19
This guidance work was initiated under project titled:
Reducing Nosocomial and Community-Acquired Tuberculosis by Strengthening the Capacity of the South African Department of Health to Improve Implementation of Infection Control and Waste Management at All Levels of the Health System Under the President's Emergency Plan for AIDS Relief (PEPFAR)
Purpose and approach
The global pandemic of COVID-19 caused by the coronavirus, SARS-CoV-2 is likely to result in a surge in need for medical care for Severe Acute Respiratory Syndrome (SARS) in South Africa. Considering the course of the pandemic in other countries, it is anticipated that South African hospitals will not have sufficient capacity to cope with the surge of persons requiring medical attention and that surge capacity via alternate care sites (ACS) will need to be established. Surge capacity, contemplated here is not the frequent emergency department overcrowding experienced by healthcare facilities (e.g. Friday/Saturday night emergencies) or local casualty emergency that might overcrowd nearby facilities and have little to no impact on the overall healthcare delivery system. It is when a catastrophic event occurs and the affected population seek medical care from existing local healthcare facilities, causing healthcare infrastructure to become exhausted due to excess in demand. During a healthcare surge, the standard of care will shift from focusing on patient-based outcomes to population-based outcomes, and providers should anticipate “a shift to providing care and allocating scarce equipment, supplies and personnel in a way that saves the largest number of lives in contrast to the traditional focus on saving individuals.”[1] Surge capacity can be temporarily established in non-traditional environments, such as hotels, exhibition halls, community halls, and as field hospitals, on open spaces. In the context of this document, a quarantine site is a facility for patients who do not require continuous professional medical care, while an ACS is defined as a temporary facility that can provide continuous medical care for SARS. This document provides principles and considerations, high-level guidance for minimum requirements and examples for ACS. While an extensive set of health facility guidelines does exist2 , these are applicable for conventional facilities and thus include services and guidelines that are not necessarily relevant to the treatment of a novel, highly infectious pathogen, with pandemic effects. Moreover these do not provide well for the rapid and temporary establishment of facilities. In order to formulate high-level guidance, the team reached out to professional industry bodies for inputs, in particular the South African Institute for Architects (SAIA), The Gauteng Institute for Architects (GiFA) and the South African Federation of Hospital Engineering (SAFHE), by inviting input via a 36-hour research charrette. Relevant historical and contemporary literature was consulted, precedents identified and critically reviewed. Material from the Infrastructure Unit System Support (IUSS), international literature and guidance and input gathered from the broader architectural, engineering and healthcare professional communities was synthesised and moderated by the CSIR team. The draft was reviewed by an expert review panel. Contributors and reviewers are acknowledged in text.
Notes
Scope and assumptions
ACSs as discussed in this document are dedicated, temporary facilities for identification and treatment of persons: suspected of having contracted SARS-CoV-2, (persons under investigation (PUIs)), who are symptomatic and/or are awaiting results or are confirmed to be infected ACS will accommodate a variety of clinical, logistical, support and auxiliary services associated with the render of care. Pediatric patients are to be accommodated in separate wards, where strictly controlled visitation may be allowed.
Exclusions:
Quarantine facilities - for asymptomatic persons who are in self- or imposed isolation, but not displaying symptoms, or who are symptomatic, but are able to safely recover without clinical intervention are not considered in this document.. Service regime: The following assumptions are made with respect to services under consideration. Temporary - limited to the part of the pandemic when the “conventional” hospital platform cannot meet demand. To be dismantled, thereafter. Uncomplicated, dedicated Covid-19 care. Patients with comorbidities, paediatrics will be prioritised for conventional facilities. 24 hour, 7 days a week operations Assumed mechanism of transmission transmission is understood to be preferentially by the contact and droplet routes with opportunistic airborne transmission in special circumstances. reclassification of transmission mechanisms may nullify some of the approaches presented in this guidance.
Rationale and need
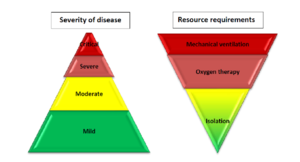
According to the WHO, Based on the largest cohort of Covid-19 patients, about 40% of patients with Covid-19 may have mild disease, where treatment is mostly symptomatic and does not require inpatient care; about 40% of patients have moderate disease that may require inpatient care; 15% of patients will have severe disease that requires oxygen therapy or other inpatient interventions; and about 5% have critical disease that requires mechanical ventilation. However, the evolution of the outbreak in some countries has shown a higher proportion of severe and critical cases and the need to rapidly increase surge capacity to prevent rapid exhaustion of biomedical supplies and staff. In some countries, doubling rates of cases every three days has been observed. South Africa has a high burden of disease, with a high prevalence of HIV and TB. Although evidence is yet to emerge of the effect of SARS-CoV-2 on a population with these pre-existing conditions, there is reason to proceed with caution. There is potential direct and indirect benefit of ACS to people living with HIV and TB, as well as to general public health and the health system preservation. It appears that South Africa is on the cusp between cluster transmission and community transmission according to WHO’s classification, indicating that preparation can include temporary hospital facilities and mass critical care.
| No Case | Sporadic Case | Clusters of Cases | Community Transmission | |
|---|---|---|---|---|
| Faculty Space, Including for Transmission | Usual Space. Enhanced Screening and triage at all points of first access to the health system | Dedicated COVID-19 patient care areas within health facility (e.g. infectious disease ward, isolation rooms in emergency or ICU wards). | More patient care areas re-purposed for COVID-19 within the health system, especially for severe cases | Expanded care for severe cases in new hospitals or temporary hospital facilities |
| Staff | Usual space. Enhanced screening and triage at all points of first access to the health system | Dedicated COVID-19 patient care areas within health facility (e.g. infectious disease ward, isolation rooms in emergency or ICU wards) | More patient care areas repurposed for COVID-19 within the health system, especially for severe cases | Expanded care for severe cases in new hospitals or temporary hospital facilities |
| Supplies |
|
|
|
|
| Standard of Care | Usual care with enhanced awareness and recognition of immediate needs for first COVID-19 patients | Usual care and treatment for all patients, including those with COVID-19 | Identify context-relevant core services. Shift service delivery platforms. Consider reduction in elective patient encounters, including elective surgical procedures. | Mass critical care (e.g. open ICU for cohorted patients). |
| Care areas expansion | No requirements for expansion | Designate 10 beds per suspected COVID-19 case | Expand COVID-19 patientcare areas by a factor of 35 | Expand COVID-19 patient care areas by a factor of 58 |
Quantification of need
AAt this time there are various parallel initiatives aimed at forecasting the South African epidemic, quantifying the projected need for facilities, and shortfall in existing capacity. At this time, there is no consensus on this. This section will be updated as further data becomes available.
ACS will attend to mild to moderately affected COVID-19 patients where basic, targeted medical care will be provided. Should patients’ needs evolve, requiring escalation of care, then transfer of patients from ACS sites to conventional sites of care will be needed as a matter of course, bringing with it logistical challenges and risks. The following pragmatic approach, aligned with the WHO recommended strategic approach, is suggested.
- ACS should be preferably identified with space for expansion. The set-up should be done so that levels of care can be upgraded to higher levels of care.
- This guidance makes the assumption that only uncomplicated COVID-19 cases will be treated at an ACS, entailing that patients with comorbidities, and paediatrics will be referred to conventional facilities. Depending on epidemic trajectory, it may be necessary to expand services to include a greater range of clinical services at ACS
Strategic approach
According to WHO, for clinical care, six major interventions must be put into place immediately, and then scaled up according to epidemiologic scenarios.
To meet the requirements set out above, prospective sites should be evaluated, by scrutinizing plans, satellite images and by physical inspection (walkabout). Expanded, services, under the current State of Disaster, could, on a temporary basis be hosted:
- Within and around existing healthcare facilities, via reconfiguration and/or augmentation.
- In existing non-healthcare buildings suitable for repurposing, such as universities, hotels and conference centres, warehouses, gyms etc.
- On open fields, including paved parking areas with rapidly constructed, dismantlable structures, such as modular tented structures or using rapid modular construction techniques.
The type of “host” site selected will strongly influence or dictate the choice of ACS service model. Some typological responses and service model are set out below in precedent examples.
| Case severity, risk factors* | Recommendations |
|---|---|
| Mild | Patient should be instructed to self-isolate and contact COVID-19 information line for advice on testing
and referral. |
| Moderate, with no risk factors | Test suspected COVID-19 cases according to diagnostic strategy. Isolation/ cohorting in:
(i.e. adjacent COVID-19 designated health post/EMT-type 1, telemedicine)
|
| Moderate, with risk factors | Patient should be instructed to self-isolate and call COVID-19 hotline for emergency referral as soon as possible |
| Severe | Hospitalization for isolation (or cohorting) and inpatient treatment.
|
| Critical | Hospitalization for isolation (or cohorting) and inpatient treatment.
|
* Known risk factors for severe COVID-19: age over 60 years, hypertension, diabetes, cardiovascular disease, chronic respiratory
disease, immunocompromising conditions.
Note: Probable cases should be retested immediately.
No site is likely to meet all requirements and recommendations set out in this document, Adaptations and compromises will be necessary. The examples set out above demonstrate that a variety of host settings are workable, provided that the appropriate utility can be contrived.
Ideally all services should be provided on site. However, the use of off-site services is not unconventional and may be practical/feasible for temporary sites, provided suitable procedures are followed. It should be noted that the key limitations are to be found in resource constraints (staff, equipment, funding), and therefore coordinated options appraisal and prioritisation is needed.
Infection Prevention and Control
Guidance for COVID-19 Infection Prevention and Control can be accessed Here