TB Services: Difference between revisions
| Line 769: | Line 769: | ||
Prevailing climate conditions should be taken into consideration during the design process. The closest freely available (open source/ public domain) or alternate annual and diurnal temperature, rainfall, wind-speed and direction data should be collected, analysed and used in addressing building performance and patient comfort objectives (see Figure 10). Material specifications and details should address corrosive attributes associated with proximity to the sea. | Prevailing climate conditions should be taken into consideration during the design process. The closest freely available (open source/ public domain) or alternate annual and diurnal temperature, rainfall, wind-speed and direction data should be collected, analysed and used in addressing building performance and patient comfort objectives (see Figure 10). Material specifications and details should address corrosive attributes associated with proximity to the sea. | ||
Rational peak demand of electricity use and demand management systems should be considered in the design and specification. There should be a split between essential and non-essential electricity use, and emergency backup should be provided for essential services. Separate metering for water and electricity should be provided for the new unit. Refer to [https://www.iussonline.co.za/norms-standards/healthcare- | Rational peak demand of electricity use and demand management systems should be considered in the design and specification. There should be a split between essential and non-essential electricity use, and emergency backup should be provided for essential services. Separate metering for water and electricity should be provided for the new unit. Refer to [https://www.iussonline.co.za/norms-standards/healthcare-environment IUSS:GNS Sustainability and the environment]. | ||
===Future development=== | ===Future development=== | ||
Revision as of 19:15, 29 July 2020
Policy and service context
Legislation, policies and international guidance
Infection Prevention and Control Legislation
- Constitution of the Republic of South Africa, 1996. s.2,24,27,36&39.
- The National Health Act 2003. (c.61). Cape Town South Africa: Government Gazette.
- The Occupational Health and Safety Act 1993. s.8(1). Cape Town South Africa: Government Gazette.
Department of Labour, 2001. Regulations for hazardous biological agents. (Government notice No. R. 1390 of the Occupational Health and Safety Act, 1993. s.43). Pretoria South Africa: Government Gazette
Department of Health, 2003. Regulations relating to the application of the hazard analysis and critical control point system (HACCP system). (Government notice No. R. 908 of the Foodstuffs, Cosmetics and Disinfectant Act, 1972. (c.54)). Cape Town South Africa: Government Gazette.
- The Environmental Conservation Act 1989. (c.73). Cape Town South Africa: Government Gazette.
- The Foodstuffs, Cosmetic and Disinfectants Act 1972. (c.45). Cape Town South Africa: Government Gazette.
Building legislation
- The Pharmacy Act 53 of 1974. (c.53). Cape Town South Africa: Government Gazette.
- The National Environmental Management Act 1998. (c.107). Cape Town South Africa: Government Gazette.
- Building Regulations and Building Standards Act 1977. (c.103). Cape Town South Africa: Government Gazette.
- South African Bureau of Standards (SABS), 1990. SANS 10400:1990 Code of practice for the application of the national building regulations.Pretoria South Africa: SABS Standards Division.
- Promotion of Equality and Prevention of Unfair Discrimination Act 2000. (c.4). Cape Town South Africa: Government Gazette.
Infection prevention and control and TB management policy and guidelines
- National Department of Health (NDoH), 2007. The draft national infection prevention and control policy for TB, MDRTB and XDRTB. South Africa: NDoH.
National Department of Health, 2007. Management of drug-resistant tuberculosis: Policy guidelines. [pdf] South Africa: NDoH. Available at: http://www.search.gov.za [Accessed 26 March 2014].
South African building practice policy and guidelines
- The South African Pharmacy Council, 2004. Good pharmacy practice. (Board notice 129). Cape Town South Africa: Government Gazette.
International design guidance
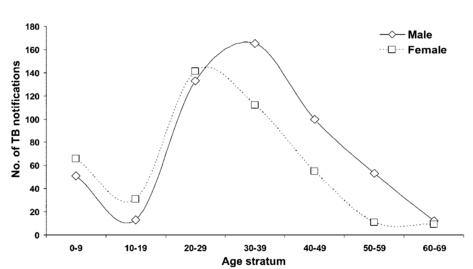
South Africa faces one of the most devastating TB epidemics in the world. TB – with TB/HIV/Aids – is the leading cause of death
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 1999. ANSI/ASHRAE standard 52.2-1999 Method of testing general ventilation air cleaning devices for removal efficiency by particle size. Atlanta USA: ASHRAE.
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 1989. ASHRAE standard 62 Ventilation for acceptable indoor air quality. Atlanta USA: ASHRAE.
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 2003. HVAC design manual for hospitals and clinics. Atlanta USA: ASHRAE.
Chartered Institution of Building Services Engineers (CIBSE), 1997. CIBSE applications manual AM10 natural ventilation in non-domestic buildings. London: CIBSE.
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE),
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 2009. ANSI/ASHRAE/ASHE standard 170-2008 ventilation of health care facilities. Atlanta USA: ASHRAE.
- QASA, “Know Your Rights” [Accessibility & the Built Environment]
- Department of Health and Human Services (Centre for Disease Control and Prevention), 2003. Environmental control for tuberculosis: Basic upper-room ultraviolet germicidal irradiation guidelines for healthcare setting. USA: DHHS.
- World Health Organisation (WHO), 2009a. Natural ventilation for infection control in health-care settings. Geneva Switzerland: WHO
- World Health Organisation (WHO), 2009b. WHO policy on TB infection control in health-care facilities, congregate settings and households. Geneva Switzerland: WHO
Service context
The WHO reports that TB treatment success is low and treatment default rates and mortality are high. The high default from TB treatment by patients represents a major problem which, in conjunction with other factors, has led to the emergence of drug-resistant TB (DR TB). Transmission of TB, multi-drug-resistant TB (MDR TB) and extreme (or extensively) drug-resistant TB (XDR TB) in communities and congregate settings has been documented in several studies, frequently linked to HIV infection and affecting vulnerable groups such as children. MDR and XDR TB linked with HIV therefore have the potential to result in an uncontrollable epidemic with devastating economic and social consequences. The epidemiological burden co-infection in South Africa is currently estimated to be in excess of 70% of TB and HIV (WHO, 2009b). Provision of poorly designed, maintained and operated infrastructure can exacerbate transmission. Well-designed and well-maintained facilities can reduce the risk of TB infection.
M. tuberculosis is an infectious disease, and is transmitted from person to person exclusively by the airborne route, usually through coughing by a patient with active pulmonary TB. MDR TB is a consequence of human error resulting from combinations of the management of drug supply, patient management, chemotherapy prescription and patient adherence. Treating MDR TB takes longer and requires drugs that are more toxic, more expensive (up to 100 times the cost of treating a drug-susceptible TB patient) and generally less effective, particularly in persons with HIV infection.
The problem of drug resistance in TB has been compounded by the emergence of XDR TB. Patients with XDR TB are extremely difficult and expensive to treat, with mortality rates between 50 and 70% (CDC, undated). In XDR TB patients with HIV co-infection, mortality rates, though improving, remain at about 90% (Neel, et al., 2010).
Owing to the District Health system, patients are intended to, and generally do, enter the healthcare system via primary healthcare services - namely the clinics and community health centres (CHCs) and private general practitioners (GPs). It is in these settings that untreated, undiagnosed infectious individuals will inevitably come into contact with susceptible individuals and the risk of transmission is produced. With the introduction of the NHI, the profile of risk in former “private” facilities may change as demographic shifts in access to these services occur. It is therefore in the interest of public health that private-sector facilities are designed, constructed and operated to meet airborne infection control requirements.
The National Department of Health (NDoH) Primary Healthcare Directorate advocates the WHO-endorsed approach in the public sector to integrated service provision (WHO, 2011). In the context of this document, this means that individuals seeking care are to receive all appropriate services and interventions at a “one-stop shop”. The common practice of provision of service by diagnosis within a facility (e.g. separation of TB, HIV/Aids, diabetes) or by vertical programmes (different clinical activities on different days) does not support integration of services. This implies that, as far as it is safe and reasonable, most services should be available in most patient/client contact spaces. The integration of services should not subject healthcare workers, clients or the public to undue exposure to airborne pathogens. In particular, when reconfiguring services in existing facilities, due diligence must be paid in ensuring that designs meet required standards for TB infection control.
Most TB patients will access services at the primary healthcare level and will require access on site to integrated services including, but not limited to:
- clinical assessment (consulting room with examination facilities, clinical scale);
- safe facilities for sample (sputum) collection;
- nutrition;
- psychosocial services (counselling); and
- pharmacy dispensary for chronic medication.
In addition, on- or off-site access to the following services is required
- laboratory services (microscopy, culture, GeneXpert, for drug sensitivity), and
- radiology.
For a quick reference to primary healthcare services for uncomplicated building projects consult IUSS:GNS Primary Healthcare.
Evidence suggests that drug-susceptible TB and MDR TB, when diagnosed and under treatment, become rapidly less infectious (Dharmadhikari, forthcoming). This means that, after as little as 24 hours on appropriate treatment, TB patients - and even MDR patients - can be regarded as and accommodated with the non-infectious population. No special facilities are required for these patients (if they are short-term patients) and they can be accommodated in accordance with IUSS norms and standards (Refer to IUSS:GNS Adult inpatient services).
Patients recently enrolled on treatment (<24hours) who are suspected of having XDR, confirmed XDR patients, patients who interrupt treatment, and complicated cases may be considered infectious and negative-pressure isolation is strongly recommended - or, if not possible, at least patient management by respiratory isolation or, if that is not possible, by patient cohorting (patient management by clustering patients with most similar diagnoses).
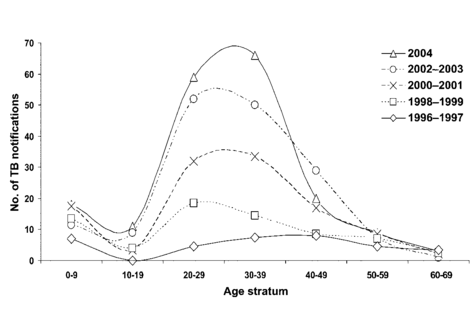
The number of DR TB cases in South Africa increased from 10 085 in 2011 to 15 419 in 2012 (WHO, 2013, p.52). This is largely due to intensified case finding and investment in laboratory services. However, it represents only a portion of the estimated cases (WHO, 2013).
Since 2010 the SA National Department of Health has adopted a policy of decentralised management of Multi Drug-resistant TB. In addition to outpatient services, there is a requirement for inpatient hospital facilities:
- for all types of TB patients (pulmonary, extra-pulmonary, etc.) requiring acute treatment for TB or other comorbidities
- within patient populations of general hospitals,
- In dedicated wards at general hospitals for acute episodes, and
- at specialised hospitals (long-term accommodation) for sub-acute and palliative care for patients who are not best served by community-based care, for various reasons.
Inpatient beds for TB services have frequently been provided by converting old wards and sanatoria as a quick solution to address at least part of the pressing need. In many instances building infrastructure has been modified or retrofitted with the intention of making it suitable. However, because beds are provided in this reactive way, the infrastructure is frequently poorly aligned with current best infection-prevention and ‑control practice and patient-centred care.
There have been both legal and ethical challenges posed to TB hospitalisation (Singh, Upshur and Padayatchi, 2007; London, 2009). Media have reported incidents of patients rioting and absconding (Dugger) which attested to the unpopularity of the policy and the unsuitability of the arrangements, including - though by no means limited to – the building infrastructure provided.
The NDoH has subsequently recognised the need to provide recreational, occupational and educational facilities for patients that require specialised long-term DR TB treatment (NDoH, 2007b, p.25). Social support should also be provided for all patients and their families whilst hospitalised. In the past TB facilities were simply not designed or built to address these needs. This must be recognised when assessing precedent or in identifying case study examples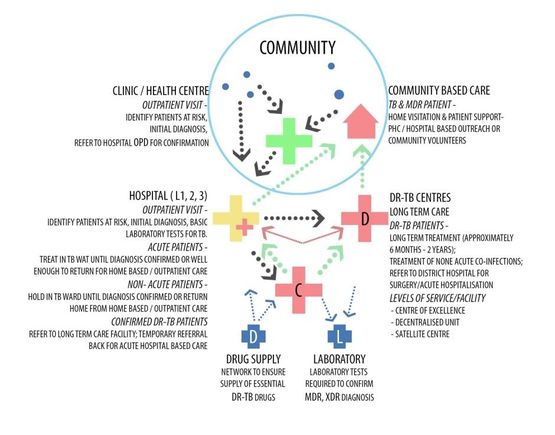
- Well ventilated consulting room
- Well ventilated waiting area
- Well ventilated rooms that can accommodate from one to six patients
- Distance between beds not less than 1.2 m
- Administration control measures of infection control in place
- UVGI lights and extractors fans where possible
- Respiratory protection tools available: surgical masks, N95 respirators
These policy requirements will go some way to addressing the twin objectives of patient-centred care and effective infection prevention and control in the emerging pandemic. However, there are additional planning, design, management and maintenance considerations to reach best practice standards and these are discussed in detail below.
Understanding transmission to manage risk
Transmission of M. Tuberculosis
When the droplets produced by an infected person are inhaled by a susceptible person, TB may be contracted. However, this alone does not seem to account for observable instances of transmission. There is a widely accepted theory - the droplet-nucleus hypothesis - that infectious droplet nuclei containing tubercle bacilli may remain suspended in air for prolonged periods of time, potentially long after the infector has left the room. This leads to a high risk of infection in congregate settings (shared spaces). This risk cannot be eliminated. However, expert consensus is that with adequate ventilation or air purification the risk can be reduced. Here is a brief explanation for the transmission theory (Riley and O’Grady, 1961).
The bacterium, M. tuberculosis, becomes aerosolised in small droplets of water or bodily fluid when a person with the disease of the lung coughs, sneezes, laughs or sings. Many of the smallest respiratory droplets dry into “droplet nuclei” and become airborne following room air currents is described. Infection can occur when the droplet nuclei containing the bacterium are inhaled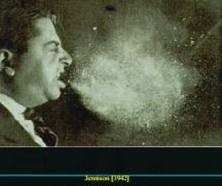
The infection turns to disease when the body can no longer contain the infectious material in the lung. The infection then spreads, usually within the lung (where it is called pulmonary TB) and possibly to other areas of the body. This spread usually shows up as chronic respiratory symptoms such as cough and fever. People with TB disease of the lungs can therefore transmit the infectious bacterium.
Disease status
- be actively diseased and infectious;
- be simultaneously infected by more than one strain;
- be diseased and undergoing treatment;
- be recovered after undergoing therapy;
- be developing resistance while undergoing therapy;
- have latent disease;
- have relapsed into disease;
- be re-infected;
- be immune; or
- have additional related/ unrelated medical conditions (co-morbidity)
Determining the current status of any given patient or transition times between statuses is problematic (given lags in diagnosis, individual patient responses etc.).
Table 1: Drug resistance TB (CDC, 2010, slide number 28)
| Mono-resistant | Resistant to any one TB treatment drug |
| Poly-resistant | Resistant to at least any 2 TB drugs (but not both isoniazid and rifampin) |
| Multidrug-resistant
(MDR TB) |
Resistant to at least isoniazid and rifampin, the 2 best first-line TB treatment drugs |
| Extensively
drug-resistant (XDR TB) |
Resistant to isoniazid and rifampin, PLUS resistant to any fluoroquinolone AND at least 1 of the 3 injectable second-line drugs (e.g., amikacin, kanamycin, or capreomycin) |
Manifestations of TB
Drug-susceptible TB
Pre-MDR TB
Drug resistance [see Table 1: Drug resistance TB (CDC, 2010, slide number 28)] can only be defined through laboratory confirmation of in-vitro resistance to one or more anti-TB drugs. Results are defined as follows:
- Mono-resistant TB: in patients whose infection isolates of M. tuberculosis are confirmed to be resistant to one first line anti-TB drug.
- Poly-resistant TB: TB in patients whose infection isolates are resistant in vitro to more than one first line drug, other than isoniazid and rifampicin.
MDR TB
Pre-XDR TB
XDR TB
Paediatric patients
Origin of airborne infection
The size of the droplets swept by an air current from the surface of a liquid is determined principally by the velocity of the air and the surface tension of the liquid. As the air velocity increases, the size of the droplets decreases until above 100 m/s where the diameter of the water droplets approaches at least 10 microns (μm). In sneezing and coughing, the peak air flow in the bronchi approaches 300 m/s and the droplets are in the order of six μm in diameter.
After being expelled from the TB patient’s mouth and nose, even the smallest droplets begin to fall. Generally, the large particle droplets fall to the ground where they become mixed with dust (see Figure 11). The fate of the smaller droplets is however, quite different. Droplets below a certain aerodynamic diameter fall slowly and lose water rapidly and evaporate almost instantaneously. In this way the droplet diminishes in size until the concentration of dissolved substances is such that the vapour pressure which the droplet exerts equals that of the atmosphere.
The residue of the droplet after evaporation, which may contain the micro-organism(s) from the respiratory tract, has been called the droplet nucleus. Droplet nuclei are so light that they may not settle in the gentlest of moving air of occupied spaces and may remain suspended for extended periods of time. This poses risk to building occupants until the particles are removed by ventilation or through other air disinfection.
Tubercle bacilli cannot be cultured from the air because of their low concentration and slow growth rate relative to other micro-organisms. The slow growth of tubercle bacilli and low concentrations in air require long sampling periods during which culture media, even with selective antibiotics to suppress microbial growth, become overgrown with fungi and other bacteria. Molecular amplification methods can detect nucleic acid from tubercle bacilli in the air, but cannot distinguish living from dead organisms nor quantify those with infectious potential. It is therefore not possible to measure infectiousness of TB or DR TB directly, nor can the efficacy of environmental infection control interventions to reduce or prevent transmission be measured directly.
Also, when considering airborne contagion, it is not well understood is how many infectious particles, or droplet nuclei, are required to infect. Compounding this uncertainty there are marked differences in the numbers of organisms liberated by coughing and sneezing of individual infectors. Despite these limiting factors, which are the subject of on-going speculation, investigation and scientific research, the general principles of contagious potential applies.
In any form of contagion the probability of infection increases with the degree of exposure to the infection (see Figure 3: Contagion). The factors implicated in the potential to be contagious are:
- the presence of susceptible members of the community
- the presence of infectious cases
- the effective contact rate (opportunities for transmission) influenced by variables which in the airborne example are factors such as:
- exposure time
- breathing rates of infector and susceptible
- virulence (strength) of bacteria
- environment (qualities of the room, such as humidity, air volume)
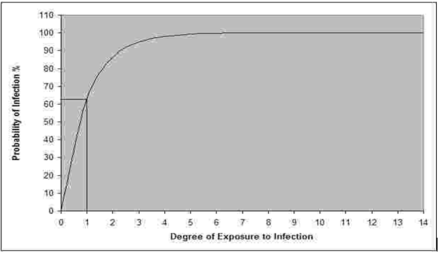
The probability of infection (1- e -Iqpt/Q) as a function of degree of exposure to infection Iqpt/Q (The point where Iqpt/Q =1 is identified by the co-ordinates).
The number of new cases occurring in an epidemic is directly related to the number of susceptible persons, the number of infectors and the effective contact rate. Respiratory droplets (for example flu), with their limited flight, range and dependence on the simultaneous presence of source and subject, behave as a form of effective contact. Droplet nuclei, with their prolonged suspension and rapid dispersion may provide an enhanced exposure and effective contact rate. It was for this reason that Wells called droplet-nucleus-borne infection, airborne contagion.
DR TB can be acquired in two different ways: primary and secondary modes. Primary transmission is caused by person-to-person transmission of a drug-resistant strain of the TB bacilli. Secondary infection develops during TB treatment, either because the patient was not treated with the appropriate treatment regimen or because the patient did not follow the treatment regimen as prescribed. Approximately 1.8% of new TB and 6.7% of retreatment cases results in MDR. DR TB can be transmitted in the same way as drug-susceptible TB.
Evidence suggests virulence of DR TB is the same as for drug-susceptible strains. However, DR TB is more difficult to treat because it can survive in a patient’s body even after treatment with the first-line drugs is started. A key challenge with current tuberculosis diagnosis technique is the delay in culturing this slow-growing organism in the laboratory. Blood or sputum culture results can take between four and twelve weeks. Because there has historically been a delay in diagnosing drug-resistant TB, these patients may be infectious for a longer period of time. Rapid screening tools for drug-resistance (GeneXpert) have been approved by the WHO, and are now in widespread use in South Africa.
The infectious droplet-nuclei which may remain suspended in air for prolonged periods of time and the respiratory droplets leads to a high risk of infection in shared spaces. This risk cannot be eliminated. However, expert consensus, based on strong circumstantial evidence, is that with adequate planning, design, management and maintenance, this risk can be reduced or managed. International best practice indicates that patients with drug-resistant TB should be closely monitored when commencing treatment and they should remain in isolation until they are no longer infectious.
The following invasive procedures should be regarded as high risk situations for transmission (Culver, Gordon and Mehta, 2003):
- bronchoscopy,
- sputum collection and induction, and
- administration of aerosolized medications
Infection prevention and control hierarchy
The requirement for controls to minimise the risk of spreading this airborne disease is legislated in the OHS Act (Act 85 of 1993). The National Department of Health Tuberculosis Strategic Plan for South Africa, 2007-2011, in the Decentralised Management of Multi Drug Resistant TB – a Policy Framework for South Africa and various international agencies such as the WHO, Centers for Disease Control and Prevention in the USA provide policy guidance for infection control practices. Common to the last two is the need to base these practices on the hierarchy of control measures. These are arranged from most to least important as follows:
Administrative measures such as work practices, policies and procedures, education and training, TB screening of healthcare workers, and appropriate utilisation of existing facilities, the implementation of environmental (engineering) controls, and the use of personal respiratory protection in specified areas where there is a high risk of exposure.
Administrative IPC measures
- early diagnosis of potentially infectious TB patients,
- prompt separation or isolation of infectious TB patients, and
- the prompt initiation of appropriate anti-tuberculosis treatment.
Other important administrative control measures include an assessment of the risk of transmission in the facility, the development of a TB infection control plan that details in writing the measures that should be taken in a given facility, and adequate training of healthcare workers to implement the plan.
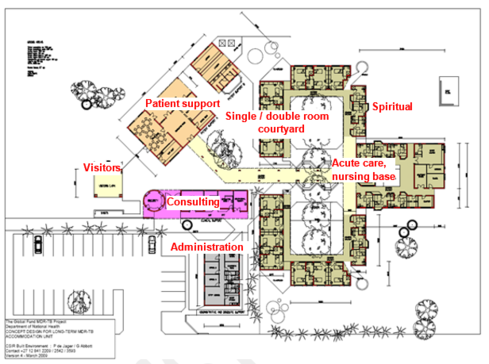
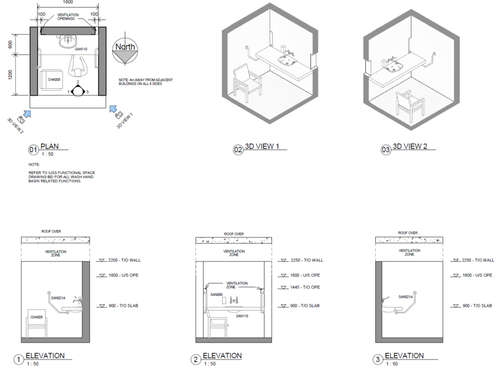
From a facility planning and design perspective, administrative control measures can be addressed through the spatial separation techniques of functional separation, respiratory isolation, and separation for patient management. Functional separation (see Figure 4) provides for the physical separation of functionally discrete parts of the facility. Administrative functions and clinical support (admissions and discharge, accounts and finance, information services, medical records) should be substantially or exclusively reserved for staff use, and zoned separately. Nursing services, outpatient facilities, allied health services (radiology, pharmacy, rehabilitation) and visitors’ spaces may be used by both patients, staff and visitors, but should be laid out and managed so that the appropriate infection control measures are ensured. Finally patient support facilities, recreation facilities, and patient wards should be accessible to patients, but not necessarily all patients at all times, because of risk of cross-infection.
The following situations and design features have been identified as presenting the potential for increased risk of TB transmission in healthcare settings, so that when allocations of spaces are made in existing infrastructure systems the following should be borne in mind:
- Congregate settings - any setting (usually waiting areas) where large groups of patients are kept in close proximity to each other are potentially high risk areas. The highest risks are usually in admission, main outpatient, emergency or pharmacy waiting areas where undiagnosed or untreated patients congregate. Smaller waiting areas or other functional areas, such as in x-ray departments or even multi-bed patient rooms can equally pose a risk.
- Restricted / inadequate ventilation - appropriate ventilation is important, especially in congregate settings or other direct contact areas, such as dining facilities, occupational therapy areas etc. Waiting areas need to be adequately ventilated at all times in order to dilute concentrations of infectious airborne bacteria. Areas such as consulting, examination, counselling or treatment areas where staff spend long times in relatively small areas in close proximity to patients should be considered high risk areas. Minimum opening window areas are prescribed but often not complied with. The WHO guidelines (WHO, 2009a) indicate a target of 20% open window area to space floor area. The design of the window is also important to promote natural ventilation. However improved ventilation alone is usually not enough to reduce risk in that the directional flow of air to and from adjacent areas needs to be addressed.
- Shape and volume - the shape and volume of a space can also be a risk indicator. Occupied spaces with minimal floor to ceiling height (often found in multi-storey buildings) are generally higher risk areas than those with a shaped ceiling to high level clear storey windows. Shape and volume usually is linked to ventilation flow patterns and rates. The position and ease of opening of both high and low level windows is important. Staff awareness of the need to keep windows open to allow unobstructed ventilation is needed. “Open window” stickers are frequently used to provide visible reminders of open window policy.
- Adjacency - the distance between carriers and staff or other patients is a risk factor. Congregate areas where patients are sitting close together is an obvious situation and settings where close contact occurs such as during consultation, examination and treatment are risk situations. Narrow bed spacing (less than 1.2 m) presents risk for both fine droplet and droplet nuclei contamination. Multi-bed wards configurations are risk situations.
- Places where aerosol-generating procedures are undertaken- These are defined as high-risk procedures that may increase the potential of generating droplet nuclei because of the mechanical force of the procedure (e.g. intubation, cardiopulmonary resuscitation, bronchoscopy, autopsy, and surgery where high-speed devices are used) (WHO, 2007)
Total respiratory isolation for TB treatment would be ideal from an infection prevention and control point of view. Several factors make this both impractical and undesirable. First there are negative social and psychological impacts to strict separation including isolation and stigmatisation of patients. Second, nursing requirements, acuity and management dictate that patients must be visible to healthcare workers and accessible to them.
TB facilities generally experience highly fluctuating patient demographics and needs. Given resource constraints and high demand, it is frequently useful to provide configurations which allow for flexible arrangements which can be administered according to prevailing needs.
Management of patients may require spatial and/ or physical separation in accordance with facility policy:
- according to gender
- ostensibly drug susceptible TB – retreatment (treatment failure)
- Mono-resistant TB (suspected-MDR)
- Poly-resistant TB (suspected-MDR)
- MDR TB
- MDR treatment failure
- Pre XDR TB
- XDR TB
- XDR treatment failure
- First sputum culture negative result, pending second result (suspected cured)
- children (with or without boarding parents)
- patients requiring isolation ( for additional infectious diseases, psychological disturbance, prisoners)
Occasionally facility policy may allow for or require additional accommodation for outpatients, visitors or patients awaiting transfer. This may be applicable to specialised facilities (Centres of Excellence), where family and patients are likely to travel great distances but will not be applicable to Satellite Facilities on the decentralised scheme.
Administrative control measures must also ensure optimal operation of environmental control measures (see below). This may include assignment of a person to oversee environmental controls, to open and close windows as appropriate, change filters, test environmental control measures periodically, clean UVGI lamps if installed, perform preventative maintenance measures, etc. Whatever environmental control measures are in place, their adequate operation and maintenance should be included in the administrative control measures through the TB Infection Control Plan and their operational parameters and proper function should be evaluated regularly.
Environmental IPC measures
Dilution is most easily achieved through maximising air volume through design of large spaces and addressing ventilation, in particular the introduction of “fresh” air from a “safe” source (preferably outdoor air) to continually replenish indoor air as it is exposed to infected persons.
The removal of contaminated air by dilution alone requires extremely large per-occupant ventilation rates to minimise risk. Acceptable levels of room airborne contaminant removal in most South African healthcare facilities cannot be sustainably accomplished by artificial ventilation alone. Its application is limited by engineering constraints and by cost. The professional consultant team is to consider the strategy to ventilation in the following prioritised sequence and only proceed to the next option if the previous is not achievable or not feasible: natural ventilation, mixed mode ventilation and finally mechanical ventilation.
The disadvantages of reliance on natural ventilation for infection control include climate dependence and impact on patient comfort. Yet, the low cost of installation, operation and maintenance should be considered as benefits. The continuous escalation in the cost of electricity and ever-present risk of power outages further support the need to design, wherever possible, for natural rather than artificial ventilation.
The ventilation capacity of any naturally ventilated building is dependent on:
- Wind direction and profile;
- Building geometry;
- Interior obstructions and flow paths;
- Inner and outer temperature (buoyancy);
- Type and degree of envelope and building permeability;
- Adjacent structures and building location;
- Terrain; and
- Complimentary ventilation systems.
The successful commissioning of the installed ventilation system depends on the successful completion of the following steps:
- Definition of performance and functional requirements as identified during the project definition stage
- Ensuring that the performance and functional requirements are met by the design and specification
- Validating that the ventilation system performs and functions as intended. An independent authority shall validate the performance and functioning of the ventilation system.
Whereas the requirements of SANS 10400 XA contemplate the limitation of infiltration and exfiltration of air from the building (sealing for energy conservation) a rational design approach must be adopted for natural and mixed mode systems.
Dilution systems
According to the WHO Guideline Natural Ventilation for Infection Control in Health-Care Settings (WHO, 2009a), if natural ventilation alone is not able to reliably meet both the recommended ventilation and indoor comfort requirements then alternate ventilation systems, such as mixed-mode ventilation, should be sought. If that too does not meet the ventilation requirements, only then should mechanical ventilation systems be considered.
A summary of the advantages and disadvantages of natural, mechanical and mixed-mode ventilation is provided in Table 2
| Mechanical ventilation | Natural ventilation | Hybrid (mixed-mode) ventilation | |
| Advantages | Suitable for all climates and weather with air-conditioning as climate dictates | Suitable for warm and temperate climates – moderately useful with natural ventilation possible 50% of the time | Suitable for most climates and weather |
| More controlled and comfortable environment | Lower capital, operational and maintenance costs for simple natural ventilation | Energy saving | |
| Capable of achieving high ventilation rate | |||
| Smaller range of control of environment by occupants | Large range of control of environment by occupants | More flexible | |
| Disadvantages | Expensive to install and maintain. | Easily affected by outdoor climate and/or occupants’ behaviour | May be expensive |
| Reported failure rate in delivering the required outdoor ventilation rate | Reduces occupants comfort level when hot, cold or humid | May be more difficult to design | |
| Potential for noised from the equipment | Inability to establish negative pressure in isolation areas, but may be provided by proper design; depends on situation | ||
| Potential for noise intrusion | |||
| High tech natural ventilation shares some of the disadvantages and limitations of mechanical ventilation |
Table 2: Summary of the advantages and disadvantages of mechanical, natural and mixed-mode ventilation systems (WHO, 2009A).
Natural ventilation systems
- The desired airflow patterns from inlets to outlets (windows) through the occupied spaces need to be defined. This is closely related to the form, arrangement and management of the building, which in turn depends on the use patterns and even configuration of the site.
- The principal driving forces, which enable the desired airflow patterns and ventilation rates (air changes) to be achieved, must be defined and quantified. Certain strategies tend to be wind-driven; others stack-driven. In successful designs, the principal airflow drivers are complementary to the intended flow rate and distribution.
- Size and locate the openings (windows) so that the minimum and average required flow rates can be delivered under all operating regimes.
The incorporation of additional openings and devices such as solar chimneys, wind towers, turbine ventilators and wind scoops and cowls may assist the natural ventilation design by encouraging air to flow in a specified direction. These devices could also increase the ventilation rate.
For natural ventilation, the WHO recommends the following minimum hourly ventilation rates (WHO, 2009a):
- In new healthcare facilities or renovated spaces, an hourly average of 160 l/s/patient in airborne precaution rooms, with a minimum of 80/l/s per patient.
- In general wards and outpatient departments (OPD), 60 l/s/patient. The occupancy of general wards and OPDs vary, and this should be considered in the design phase.
- In corridors and other transient spaces, a minimum of 2.5 l/s/m3 is required. When emergency medical procedure are performed in these areas , an hourly average of 160 l/s/patient is required for high risk procedures, and 60 l/s/patient for all other procedures.
In these areas the airflow should be from the infectious patients, to areas where there is adequate dilution, and exhausted directly to the outside. If this is not achievable, consideration should be given to mechanical ventilation. Sputum booths should be provided externally if at all possible. Only where this is not possible should mechanically ventilated sputum booth options be considered.
- the fluctuation rates due to changes in weather in the design of natural ventilation systems (including extremes of wind speed);
- building performance in inclement weather;
- patient comfort; and
- control of drafts in the occupied zone- Air currents in excess of 0.8 m/s in the occupied zone can cause disturbance and discomfort.
Mixed-mode systems
- Complementary mixed-mode ventilation
- Zoned mixed-mode ventilation
Complementary mixed-mode ventilation uses natural ventilation and mechanical ventilation strategies at different times of the day, or different seasons of the year, i.e. natural ventilation is used when wind conditions are favourable, and mechanical ventilation is extreme conditions. Complementary mixed-mode ventilation can further be classified as concurrent or changeover. In concurrent operation, the mechanical ventilation system works in the background to the natural ventilation system, assisting where temperature, airflow, or indoor air quality parameters are not met. In changeover strategies, the natural and mechanical ventilation systems work alternately. Seasonal and night-day changeovers are the most common.
Mixed-mode ventilation systems may benefit from control strategies. These control strategies may be manual or automatic. Automatic controls usually include sensors, actuators and controllers. The control strategy should be triggered if the required ventilation rates are not met. When this happens, the system switches from natural to mechanical. Once climatic conditions are able to deliver the required ventilation rate, the system should be set back to natural ventilation. Control strategies may also be temperature-based, or rain-based, but the required ventilation rates should be met if these controls are employed.
Mechanical ventilation systems
In high risk areas, the mechanical ventilation system should, at least, meet the following minimum ventilation requirements:
- A ventilation rate of 12 ACH, or
- A ventilation rate of 80 l/s/patient of outside or sterilised air.
Criteria 2 is required when considering congregate settings, such as waiting areas and dining halls. Criteria 1 is not relevant where option 2 is achieved. Criteria 1 is not relevant in high volume spaces (>3.5m AFFL).
Where neither of the points above can be sustainably achieved, the occupancy levels in high risk indoor spaces should be managed to remain below a level that which can be effectively served by the considered ventilation system.
The use of exhaust air filtration in single pass ventilation systems as a means of removing hazardous infectious particles from the room should be restricted to “in-room” filtration. “In-duct” filtration, will not lower the concentration of infectious airborne particles in the occupied zone in which they are being expelled by infectious persons. “In-duct” filtration can only remove the infectious particles present in the incoming air or in air being redistributed to other areas served by the recirculating system. “In-room” filtration can be achieved using portable air cleaners (PAC). PACs may therefore serve as an effective extension to the dilution process provided by controlled ventilation, where the ventilation rates required for IPC cannot be achieved. PACs can be used as a means to increase the contaminant removal effectiveness of the ventilation system (at the cost of increased energy consumption). The law of diminishing returns is applicable to any common intervention applied to reduce the probability of airborne cross-infection. For this reason it is important to quantify the expected gains before renovating, adjusting or augmenting systems.
Given the maintenance requirements for HEPA filtration and in-duct UVGI systems and the inherent occupational health risks associated with their maintenance, these systems should only be used as a measure of last resort in airborne precaution areas.
Where mechanical ventilation systems are used, consider the failure-mode fall-back option of reverting to natural ventilation.
For more detail on airborne contamination control concepts refer to the IUSS:GNS Building Engineering Services.
Disinfection systems
Upper-room air UVGI
- include the sensitivity of the microorganisms to UVGI
- and the dose of UVGI received by a microorganism
- the room occupancy levels
- or population of microorganisms.
UVGI dose is the ultraviolet (UV) irradiance multiplied by the time of exposure and is usually expressed as μW·s/cm2. A appropriatly-designed upper-room UVGI system may be effective in killing or inactivating most airborne droplet nuclei containing mycobacteria if designed to provide an average UV fluence rate in the room in the range of 15 mW/m³ to-20 mW/m³ and provided the other elements stipulated in these guidelines are met. In addition, the fixtures should be installed to provide as uniform a UVGI distribution in the upper room as possible without losing too much fluence to the walls. There is likely an upper threshold where adding more UVGI will not achieve significant increases in inactivation (Xu, et al., 2003).
Upper-room UVGI systems rely on air movement between the lower portion of the room where droplet nuclei are generated and the upper irradiated portion of the room. Once in the upper portion, droplet nuclei containing M. tuberculosis may be exposed to a sufficient dose of UVGI to kill or inactivate them.
When upper-room UVGI systems are installed, general ventilation systems should be designed to provide optimal airflow patterns within rooms and prevent air stagnation or short circuiting of air from the supply diffusers to the exhaust grilles. Also, heating and cooling seasons should be considered and the system designed to provide for optimal convective air movement. Consideration of the drop and throw parameters of selected ventilation air terminals is critical to ensure good mixing under all seasonal conditions.
Most rooms or areas with properly installed supply diffusers and exhaust grilles should have adequate mixing. If f air stagnation is possible, air mixing should be improved by the considered addition of vertical air mixing fans or repositioning the supply diffusers and/or exhaust grills. If there is any question about vertical air mixing between the lower and upper portions of the room due to environmental or other factors, a fan(s) should be used to continually mix the air. In a room without adequate air mixing under experimental laboratory conditions, UVGI system effectiveness increased by up to 72% when a mixing fan was used.
A number of studies have indicated that the effectiveness of upper-room UVGI systems decreases as humidity increases. The reason for the decrease in UVGI effectiveness is not clearly understood. However, the effect needs to be considered in the general context of upper-room UVGI systems.
For optimal efficiency, relative humidity (RH) should be controlled to between 25% and 60% where upper room UVGI systems are installed. This is consistent with American Institute of Architects (AIA) and the American Society of Heating, Refrigerating, and Air-Conditioning Engineers (ASHRAE) recommendations that the RH affecting patient care areas in hospitals and outpatient facilities range from 30% RH to 60% RH. If high humidity conditions are normal, it may be necessary to install a system with greater than normal upper-room irradiance levels.
Recommendations developed by ASHRAE and AIA stipulate that the design temperature for most areas affecting patient care in hospitals and outpatient facilities range from 20 °C to 24 °C. This temperature range is consistent with the optimal use of low pressure mercury lamps that are used in upper-room UVGI systems.
The most common way to generate germicidal UV radiation in lamps used in well-designed upper-room UVGI systems is to pass an electrical charge through low-pressure mercury vapour that has been enclosed in selected glass tubes that transmit only certain UV wavelengths. Care must be used in selecting the correct UVGI lamp for use in upper room UVGI systems. Typically, the optimal wavelength for UV germicidal radiation is 254 nanometres (nm) in the UVC range. UV lamps are made for a variety of purposes that may have a negligible consequence in killing airborne microorganisms. Some UV lamps (such as those used for tanning) radiate energy in the UVA and/or UVB range and over extended periods may have adverse health consequences for exposed persons. Other UV lamps are designed to emit radiation at 184.9nm and produce ozone, which is hazardous to humans even at low concentrations. Low-pressure mercury lamps should be rated for low or no ozone generation. Since all lamps must eventually be discarded, each lamp should contain only a relatively small quantity of mercury (i.e., 5mg or less).
In upper-room UV irradiation, fixtures containing UVGI lamps are suspended from the ceiling or installed on walls. The base of the lamp is shielded to direct the radiation upward and outward to create an intense zone of UVGI in the upper air while minimizing the level of UVGI in the lower (occupied) portion of the room or area. The height of the room must be considered in the design of an effective system.
A professional who is knowledgeable in upper-room UVGI systems design and installation should be consulted before procurement and installation of the system. The number of persons competent in the design of upper-room UVGI systems is normally limited.
Persons who may be consulted include engineers, industrial hygienists, and radiation/ health physicists. A mechanism to provide training certification for system designers should be developed and based on the guidance document UVGI Disinfection of Room Air: an Evidence Based Guideline for Design, Implementation and Maintenance.
Once the number and types of UVGI fixtures appropriate for the room or area have been determined, the fixtures need to be appropriately installed. Installation guidelines are provided in the Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation - Guidelines for Healthcare Settings document and the guidance document UVGI Disinfection of Room Air: an Evidence Based Guideline for Design, Implementation and Maintenance. Only qualified service technicians who have received training on the installation and placement of UVGI lamp fixtures should install the systems. Following installation UV lamps require on-going maintenance and frequent replacement, by suitably skilled technicians. This consideration may be a limiting factor in the use of the solution.
Personal protection measures
Respiratory protective devices for healthcare workers that are capable of adequately filtering out infectious particles are more expensive than surgical or procedure masks. Nevertheless, their use in high-risk DR TB settings is strongly recommended, particularly in high burden HIV settings where many healthcare workers may be HIV infected. Respiratory protection should be used only when all other administrative and/or environmental control measures are fully implemented. Acceptable respirator types meet the performance requirements outlined in table 7, and include:
- SANS 50149 FFP2/3 respirators
- CDC - NIOSH N95 respirators
The use of N95 respirators should be used with caution in South Africa as there is no framework of compulsory standards and regulations controlling their use. The user may therefore not be adequetly protected from fake devices. The National Regulator for Compulsory Specification (NRCS) has published a homologated database of FFP2/3 devices compliant with SANS 50149.
http://www.nrcs.org.za/siteimgs/CMM/Homologation%20Database%20-%20PPE.pdf
An analysis of the facility design should be made in respect of where provision for personal protective equipment PPE should be made available. These include:
- protective eyewear (for UV device maintenance)
- respiratory protection (typically respirators for healthcare workers, cleaning and maintenance staff, visitors), and
- surgical masks (for patient use).
Dry, secure storage of bulk PPE supplies conveniently located close to points of use should be provided. As respirators are costly and personalised (respirators cannot be shared) secure hanging/ drying facilities clearly marked to avoid confusion are recommended. Stations are required for daily PPE supplies and for disposal facilities (bins) for discarded masks and respirators.
Planning and design principles
- a safe, secure and functional environment for patients and staff;
- optimal accommodation and support for long term patient stay;
- low capital and on-going operating costs (service, staffing and maintenance);
- an environmentally appropriate design solution; and
- a fully accessible, inclusive environment.
Patient profile
Some population groups, such as prisoners and miners are at increased risk of contracting TB.
Patient-centred care
There is strong evidence from research studies which describe the importance of health facility design as a means to improve health outcomes (Ulrich, et al., 2008). The more supportive the environment is, the less chance there will be of admitted patients absconding and infecting others in the community while still in an infectious stage of the disease. Environmental factors such as large windows with high levels of daylight, views of nature, low noise levels all reduce stress and depression and promote healing. Some visual and acoustic privacy (screening for confidential/ personal activities in counselling, consulting and ward areas) promotes patient dignity. Personal choice and control over heating, lighting and furniture layout instils a sense of empowerment.
Safety
Isolation
Distinction can be made between five types of segregation:
- Separation – patients are housed in single room accommodation though they may not be self-harming or violent.
- Negative pressure room applied to infectious patients, with airlock ante-chamber (e.g. TB patients).
- Positive pressure isolation room applied to immuno-compromised/ susceptible patients, with airlock (e.g. burns patients).
- Duel-function isolation – with controls to convert from positive to negative pressure according to current room occupancy, with airlock. This is discouraged due to complexities in designing and operating these and due to increase risk in accidental incorrect use.
- Seclusion (Social isolation) – for patients who are self-harming or violent. A room with high level of security which complies with national norms and standards for psychiatric care facilities. Airlock not required.
- Barrier isolation – patients are housed within a chamber constructed of an impermeable barrier and typically ventilated through HEPA filters. Decontamination airlocks and material transfer chambers are included in the system. These types of systems are exclusively used for suspected P4 level pathogens, and are not indicated for use with TB patients.
When briefing professional consultant teams, it is important to convey where each of the above is required. For TB, infection control is useful and usually all that is provided. For further information on Isolation rooms, the reader is referred to the IUSS Adult In-patient Services guidance document. https://iussonline.co.za/norms-standards/clinical-services
Infection prevention and control
Slips, trips and falls
Alarms and fire alarms
In addition to the usual compliance requirements, it should be noted that as deafness is a common side-effect of TB treatment regimes, all sounding alarms including fire alarms should be supplemented with visible alarms in patient areas e.g. red or yellow flashing lights to accompany fire or emergency evacuation alarms.
UV exposure risk
UVC is unlike UVA and UVB, as it has extremely low penetrating ability. It is nearly completely absorbed by the outer layer of the skin (stratum corneum), where little or no harm is experienced. Although listed as a potential carcinogen for man, UVC is unlikely to be carcinogenic or to cause skin or eye irritation (keratoconjunctivitis) if applied correctly within exposure limits as set out by the International Radiation Protection Agency (IRPA) and other international health bodies.
Since open UVGI devices are principally designed to emit a certain amount of UV-c radiation, these devices cannot be considered to be intrinsically safe. The UVGI system should be designed to achieve the maximum system output and maintain the lowest reasonable exposure levels in the occupied zone of the room.
Safe Exposure Limit
Therefore, in the typical application of 254nm devices, occupant exposure shall not exceed 0.40µW/cm² for a period of time equivalent to 4 hours per work day. If exceeded, steps must be taken to reduce the effective irradiance dose to less than 6.0mJ/cm2 for the total duration per day.
It becomes important to consider the actual nature and usage of these spaces to determine appropriate safe exposure rates. In determining these rates, occupancy factors such as the eye level of regular occupants, position of occupants (seated, standing, lying down), frequency and duration of exposure, need to be determined and incorporated. Therefore different areas or rooms will require different safety limits.
Areas such as passages and wards would therefore demand vastly different safety limits from each other.
The economic considerations of infection control suggest that high risk areas be given priority for air disinfection. These areas will be determined through the outcome of a comprehensive risk assessment of the facility. Installation of open UVGI devices in stairwells is not considered safe practice as there is seldom sufficient soffit height for an effective upper room zone. Where passages are used as return air plenums in recirculating ventilation systems, these passages shall be considered for air disinfection.
Reflections into the Lower Room
Security
Inclusive design
Holistic care
Balanced service provision
Given resource constraints, it is not always possible to invest in the full complement of these facilities at DR TB centres in one capital investment. However, as each potentially adds to quality of care that can be delivered, which leads both directly and indirectly (say, through preventing absconding) to improved health outcomes, best practice recommends that these aspects be addressed as fully as practicable. It is useful to produce master-plan proposals, within a phasing framework so that a full complement of services can be provided over time, and so that short term development does not compromise medium and long term development potential.
Patients in some DR TB settings are permitted to prepare their own meals, but this is unusual practice and is usually optional and reserved for patients who are pending discharge. Policies in terms of meal presentation and delivery vary between institutions. Three basic modes of delivery include a pre-plated service delivered to the patient bed. The second mode is a tray served at a dining table and the third is a buffet-style service. As meal preparation services are frequently outsourced, the first two modes of delivery are most commonly found in South Africa. Dedicated dining facilities are not always available, so that meals must be served at patients’ bedsides or lounge areas (if provided). Bedridden and ill patients may be unable to use formal dining facilities. International studies in long-term care facilities have shown that there are increased appetite, nutrition and patient satisfaction in communal dining settings, and particularly with buffet-style eating. However these studies have primarily been undertaken for the elderly. Similar studies have not been undertaken in South Africa or for TB patients. To complicate matters, patients in communal dining settings are unable to use personal protective equipment, raising risk at these encounters. Nevertheless it is recommended that patient formal dining facilities be provided for and that they are treated as high risk areas in terms of infection control.
Facility policy may provide that patients in long-term care facilities are encouraged to participate in cleaning, laundry and gardening activities.
Healing environments
Occupant comfort
Buildings should be designed so that comfort conditions in indoor environments can be achieved irrespective of climate conditions, bearing in mind that TB sufferers are typically very underweight and may have little tolerance for cold. The climate may require supplemental heating to achieve comfort conditions in winter without compromising the ventilation requirements. The operational constraints of the hospital (in terms of maintenance and operational costs as well as environmental impact) mean that fully air-conditioned or heated wards are usually not desirable either.The ISO standard 7730 provides a measure of thermal comfort based on the predicted mean vote (PMV) method. The ASHRAE 55 Thermal environmental conditions for human occupancy guide provides methodology for measuring comfort conditions, including provision for naturally ventilated buildings. It is proposed that these form the basis of the design assessment relating to thermal comfort.
The ventilation and comfort control design must weigh up these competing requirements to provide an optimal indoor environment (ventilation and thermal comfort) while bearing in mind the operational impacts on the hospital in the long term. As such, the following metrics should be used to demonstrate an optimal balance of ventilation, thermal comfort and operational costs:
- Proportion of hours where the targeted ACH rate is achieved (currently 160 l/s per person for naturally ventilated areas)
- Proportion of hours where either:
- PMV levels between -1.0 and 1.0 are achieved; or
- Acceptability limits of ASHRAE Standard 55, 2004 are achieved within 80% of acceptability limit 1
- Predicted operational costs (energy use and maintenance)
The decision-making with respect to the mechanical or naural ventilation system or other systems relating to thermal comfort should take all these into account.
Staff: patient ratios
| Doctor | 1/40 beds |
| Professional nurse / Staff nurse or Nursing Assistant | 4/ 11 per 40 beds |
| Pharmacist | 1 per 100- 200 beds |
| Social worker | 1 for > 40 beds |
| Dietician | 1 for > 40 beds |
| Clinical Psychologist | 1 for > 40 beds |
| OT | 1 for > 40 beds |
| Audiologist | 1 for > 40 beds |
| Physiotherapist | 1 for > 40 beds |
| Data Capturer/ Admin Clerk | 1 for 100- 200 beds |
| Driver | 1 for > 40 beds |
Table 3: Sample Organisational Development Investigation the following staffing complement per 30 bed functional unit (courtesy Brooklyn Chest Hospital)
| OFFICE: ADMINISTRATION | NUMBER OF POSTS | COMMENTS |
| Administration clerk | 1 | |
| CLINICAL SERVICES | ||
| Medical officer | 1 | |
| MEDICAL AUXILLARY SERVICES | ||
| Physiotherapist | Central services | |
| Occupational therapist | Central services | |
| Social work | Central services | |
| Dietician | Central services | |
| Audio/speech therapist | Central services | |
| Clinical Psychologist | Central services | |
| Radiographer | Central services | |
| Pharmacist | Central services | |
| Counsellor | Central services | |
| NURSING SERVICES | ||
| ASD nursing area | Central services | |
| Operational manager nursing | 1 | |
| Professional nurse | 4 | |
| Staff nurse | 4 | |
| Auxiliary nurse | 8 | |
| Housekeeping supervisor | 1 | |
| Household aid | 6 | |
| NIGHT DUTY MANAGEMENT | ||
| Night duty manager | 1 | Central services |
| Professional nurse | 1 | |
| Staff nurse | 3 | |
| Auxiliary nurse | 2 | |
| Household aid | 1 |
Supporting the caregiver
Recruitment, retention and productivity in staff
Staff is thus a critical factor to take into consideration when DR TB planning facilities. In particular the provision of safe working environments:
- which address risk from an IPC perspective in a way which is explicit and reassuring;
- which provides for physical safety against violent/ disturbed patients; and
- which allow adequate safe storage for personal belongings.
Provision of staff housing, recreation facilities and other staff amenities may be an attractive benefit.
Additional personnel considerations
While the most significant factor in staff recruitment and retention is salaries and benefits, especially in relation to many overseas destinations, many experts emphasize that pay is not the sole motive for leaving the South African public service. Other factors include poor work environments characterized by heavy workloads, lack of supervision, and limited organizational capacity. There are also environmental considerations; workplaces may be dangerous due to condition, functional or environmental design, or there may be a lack of supplies to protect workers from occupational exposure to diseases like tuberculosis.
Site appraisal
Building layouts
- existing buildings with measured footprint and scaled spatial layout on site plan;
- current functional allocation (use) of existing buildings;
- level of utilisation of buildings;
- national monument status;
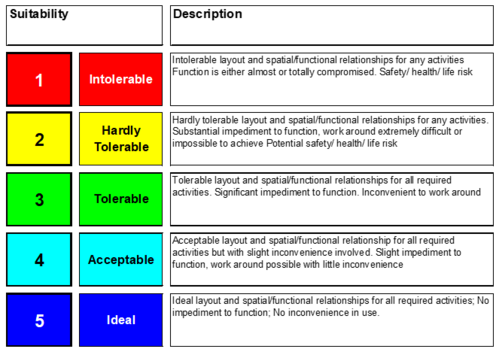
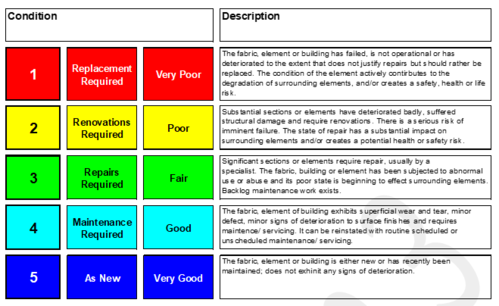
- building condition assessment (high level and quick professional estimate on scale one condemn to five as new);
- evaluate of the level of accessibility of proposed new structures and linkages to existing buildings; and
- evaluation of existing pedestrian and vehicular routes (i.e. staff, visitors, and service vehicular and pedestrian routes) to determine optimum layout of proposed new buildings.
Site Information
- Major landscaping, trees and features;
- Site access points for staff, patients and service personnel and access constraints;
- Existing fencing and level of security provided;
- Service connection points, main service runs, water tanks (as they are currently being constructed), transformers, substations, generators, etc.; and
- Flood lines, water table levels, site storm water drainage and general potential for flooding.
Engineering and bulk services
- Power: Analysis of existing power supply – types, current load, reliability, capacity, potential for expansion,
- Water supply: Analysis of existing water supply – source/s, storage, condition, current and projected demand,
- Sewage: Analysis of existing sewage reticulation and disposal system, connections, capacity, condition, current and projected load,
- ICT services: Telephones, internet connectivity, intranet connectivity. Analysis of existing supply – types, load, reliability, capacity, potential for expansion,
- Other services as identified by consultant team (gas, steam etc.)
It is recommended that the photographic survey of existing infrastructure be compiled by the consultants.
Climatic and sustainability considerations
Prevailing climate conditions should be taken into consideration during the design process. The closest freely available (open source/ public domain) or alternate annual and diurnal temperature, rainfall, wind-speed and direction data should be collected, analysed and used in addressing building performance and patient comfort objectives (see Figure 10). Material specifications and details should address corrosive attributes associated with proximity to the sea.
Rational peak demand of electricity use and demand management systems should be considered in the design and specification. There should be a split between essential and non-essential electricity use, and emergency backup should be provided for essential services. Separate metering for water and electricity should be provided for the new unit. Refer to IUSS:GNS Sustainability and the environment.
Future development
Future development for the site should be studied. The consultant team is to provide evidence that a very high level study has been undertaken to ascertain whether or not the proposed facility will likely compromise, limit or enable the proposed development through appropriate means (such as crude scale block positioning on site). The implications of the project on future development should be discussed in an open forum with stakeholders. Consideration should be given to the optimal positioning and size of central services to satisfy the future demand of the hospital site.
Additional Project Studies, Approvals and Requirements
Environmental Impact Assessment (EIA)
An Environmental impact assessment (EIA) may be required.
Local authority submissions
The following approvals must be provided, as stipulated by the local authority:
- A site development plan (SDP);
- A copy of a set of working drawings;
- A traffic engineer’s report; and
- A fire department.
Phasing and decanting
Where the project calls for a construction project to be conducted within an existing functional healthcare environment, phasing and decanting plans are required. The appropriate precautionary measures should be taken. Refer to IUSS:GNS Decommissioning. The services currently provided for at the hospital must continue with as little disruption as is reasonably possible. Phased construction and/ or temporary decanting of functions may be required. Should decanting activities be required to accommodate the construction project, then this activity should be planned timeously with all stakeholders’ involvement under the leadership of the briefing authority (or if defined as extraordinary scope of services, principal agent, contractor or other clearly identified party).
Commissioning and validation
Refer to IUSS:GNS Commissioning.
Post-occupancy evaluation
At one year from practical completion date a post-occupancy evaluation is recommended. All participants in the planning, design, construction and commissioning of the new facility will be required to participate in a half day on-site assessment on whether the project objectives where met. Feedback should be provided to the briefing authority and custodial agent to inform future building projects.
Operation and maintenance manual (O&M)
The consultant team is required to prepare an operations and maintenance manual for the hospital management and the custodial agent for presentation at practical completion. The requirements regarding the content of this document will be determined by consensus at a focus meeting with stakeholders to be convened by the principal agent during the construction phase of the project. As a recommendation these manuals may contain the following information:
General information
- Description, make, model number of all equipment installed; and
- Contact details of suppliers and /or manufacturers etc.
Design information
- Design data sheets, containing all design and selection parameters, calculations, selection curves, etc.;
- Settings and values recorded during commissioning;
- Manufacturer's brochures and pamphlets;
- Maintenance data and schedules;
- The lapse of time between services and the description of the service required of each part, lubrication requirements, etc.;
- Schedule of spares; and
- A complete electrical equipment schedule.
These will include the description, make, model number, rating and other performance criteria, commissioned (default) settings, including all brochures, pamphlets and maintenance requirements. Names and contact details of supplier and manufacturer.
Detail description of the operation of the electrical, mechanical and control systems including the design information, manufacturer’s brochures and pamphlets, settings and values recorded during commissioning, maintenance data and schedules. Complete sets of:
- as built drawings";
- architectural work drawing;
- structural drawings;
- site works drawings;
- electrical reticulation drawings;
- mechanical installation drawings (i.e. all workshop and equipment layout drawings required for the manufacture and erection of the installations); and
- instrumentation/control drawings, such as schematic control diagrams and electronic/ electrical layout drawings.
Operational narrative and user room requirements
Daily Schedule
Table 4: Sample: Current daily activities at long-term care facility
| TIME | ACTIVITY | VENUE | DESIGN IMPLICATION |
| 5:00 | Patients are woken up, urged to complete ablutions, and dress.
|
Wards | Each patient will have his own bedroom and adjoining bathroom.
Each bed will have an adjacent cupboard for clothes and possessions, and space for a bedside table.
|
| Patients to produce sputum | Sputum booth | 1.Monthly sputum samples taken from relevant patients | |
| 07:00 | Nursing on day shift attend a handover meeting with night staff. This includes discussing problems, and planning activities for the day. | Nursing station | The nursing station is a general area where much clinical information is shared between staff and between disciplines and is a separate area in the ward. Secure cupboards (and a safe), under desk shelving and notice board space are required.
|
| Matron’s office | While office should be separate from nursing station due to space requirements, easy communication and visible access should be available. Built-in office furniture with network points, plugs, telephone, filing space, lockable cupboards, enough space for at least three filing cabinets, appropriate storage and availability for ward stationery (some open and others locked), additional filing workspace, provision of pigeon holes for each for each patient file board, key cupboard. | ||
| 7:30 | Daily injection given to patients | Procedure room | Nurses prepare injections according to medicine chart per individual patient.
The room requires a clinical hand-wash basin with clinical taps, lock-up cupboards, worktops, a patient couch, good lighting |
| 08:30 | Breakfast and issuing of medication | Dining hall | This adjoins the kitchen and food delivery area. The nursing station should be nearby so that medication and general nursing tasks can be co-ordinated efficiently.
As patients mostly will proceed to the dining area from various other activity areas (sleeping, clinic, recreational, OT etc.) it will have to be in a central location, easily accessible from other patient areas. Food must be delivered through a dedicated staff access point that allows for minimal patient contact.
|
| 09:30 – 12:30 | Therapeutic activities | ||
| Medical officer
The ward will have at least one medical officer. |
Consulting room
|
These should have enough space for interviewing at least 3 people, as well as a desk, examining coach and x-ray box.
| |
| Occupational Therapy (OT) | Games room and lounge | During the day most patients will be allowed to attend the OT programme. | |
| Psychologists & Social Workers
Interviews, psychotherapy and counselling with patients or their families (often together) occur daily, usually by appointment. |
Counselling rooms
|
Each office will need built-in desks, computer and telephone points, and secure storage space. | |
| 12:30 – 13:30 | Lunch and using of medication | Dining hall | |
| 13:30 – 14:00 | Rest period
|
General rest areas | Some patients may retire to their rooms for a brief period, but most will be in general areas (lounge, restricted outdoor areas). |
| 14:00 – 16:30 | Continuation of many morning activities | ||
| Sport and Recreation | Outdoor field | These patients will have easier access to outdoor areas.
| |
| Indoor group area | For use for group leisure. | ||
| Lounge | A comfortable furnished area containing a TV, board games (such as Kerem). This area has to be fully visible from the nursing station. Public telephones should be situated nearby. It may be helpful if this was close to the dining area. | ||
| Visiting
Families, friends (and occasionally others) are allowed to visit during two afternoons per week and each evening between 19:00 to 20:00 |
Visitors area | Although visiting times are regulated, families here have easier access to the patients, and there does not have to be a strict separation between patients and visitors. | |
| 16:30 – 17:30 | Supper
|
Dining area | Activities as for other mealtimes. |
| 17:30 – 19:00 | Leisure time | Lounge | Access to enclosed courtyards allows patients to smoke and relax in the restricted outdoors before retiring to sleep. |
| 18:00 | Nursing handover to night staff
|
Nursing station | The same as in the morning |
| 19:00 – 21:30 | Preparation for sleep
Dispensing of night medication |
Lounge and sleeping areas | Usually a snack and hot drink is given to patients. Many watch TV, others socialise or smoke (the latter activity will take place in designated courtyard areas that adjoin onto the ward, but without direct access to the general campus area). |
| 22:00 – 07:00 | Night activities
|
Sleeping areas,
Nursing station |
User room requirements
Refer to IUSS:GNS Generic room requirements and IUSS:GNS Primary healthcare.
TB outpatient services
Discharged patients need to be seen for follow-up visits in their communities or at facility-based outpatients department (OPD) usually every two months or so. Treatment for newly diagnosed and uncomplicated MDR TB and TB patients is typically initiated by clinical staff at OPD, and in accordance with policy decentralised management of TB treated in the community. Complicated cases and XDR patients may be admitted into the inpatient accommodation units through the OPD unless a dedicated admissions facility is provided.
Paediatric patients may be seen for follow-up at paediatric wards or at the general OPD, depending on organisational structure. In small facilities the outpatient department can share clinical support services for inpatient care. Depending on patient loads and institutional preference, a dedicated OPD can be provided with similar facilities to clinical inpatient and support services.
Care should be taken to avoid enclosed congregate settings (such as waiting areas) where possible. Where these are required, they should be regarded as high risk for airborne contamination.
Consulting room
The consulting room is used by doctors and nursing staff for interviewing and examining patients, and to prescribe treatment for their condition. The doctor or certified nurse practitioner discusses the patients’ symptoms and records her case history. The patient sits on a chair during this stage and if a physical examination is necessary, lies on an examination couch. Once on the couch, the doctor or certified nurse practitioner examines the patient standing on the patients’ right hand side using medical supplies and instruments on an instrument trolley placed next to the head of the examination couch. The doctor or certified nurse practitioner may dispense medicine or instruct the patient to proceed to the treatment room for further medical treatment. Privacy is required during the consultation.
One consulting room should be provided per 30 patient beds or part thereof. The consulting rooms should be standard size. The consulting rooms requires a clinical hand-wash basin with a soap dispenser and paper towel holder, a desk and chair, two patient chairs, an examination couch with a curtain screen, a place to hang clothing, examination lights, access to shared x-ray viewing facility, wall mounted blood pressure monitors, telephone and computer and network connectivity. The room must have a desk with cupboard for the nurse/clinicians’ own personal belongings and a cupboard for standard forms. A separate cupboard must be in this room to provide for equipment and medicine necessary for procedures. Each room must be provided with a pinning board 900 x 900. An examination couch with an exam lamp is to be provided. Provide space next to the couch for a medicine and instrument trolley. Curtain tracks should be provided around the examination couch for visual privacy for patient being examined, if appropriate.
Counselling room
The counselling rooms must be the same size as the consulting rooms and correctly handed for use as consulting rooms should the need arise. The counselling rooms require a desk and chair, with telephone, shelves, IT and a network point, clinical hand-wash basin, soap dispenser and two easy chairs for counselling purposes.
Diagnostic radiology services
Diagnostic radiology services (chest x-rays) of all patients may be routinely required for diagnosis, during treatment and in follow-up. Baseline x-rays of all the staff and annually as part of the hospital’s infection prevention and control programme. Diagnostic radiology should be provided on-site or at a nearby referral facility. Refer to IUSS:GNS Diagnostic radiology. Mobile x-ray services are a suitable alternative where fixed radiology equipment is not available and if not provided at a nearby referral facility.
Sputum collection and induction
Sputum collection is a process whereby a specimen of sputum, liberated from the lungs, is collected. In many adults this process is readily achieved, however, in younger children and adults who cannot liberate sputum spontaneously, sputum induction is performed. Sputum induction is a process whereby sputum is liberated from the lungs using sterile water or hypertonic saline to irritate the airway, which promotes coughing, to produce a sputum specimen (Francis J Curry National Tuberculosis Centre, 1999).
It is advised that sputum collection be conducted in an area which provides privacy, for patient dignity, but also conducted under observation of a clinician, should the patient go require support and in order to ensure sample integrity (that the sputum is from the individual). As sputum collection is a high risk procedure, good administrative and environmental control measures for the designated sputum collection area is essential for the safety of healthcare workers and patients.
The functional area for sputum collection should comprise a covered area, clinical hand-wash basin, soap dispenser and counter top and, if sputum induction is performed in the same space, a splash-proof power point for a nebulizer.
Sputum collection should be performed in a designated area. At naturally ventilated primary healthcare clinics and community healthcare centres, or any other single-storey naturally ventilated healthcare establishment, sputum collection should preferably be performed in a designated outside area. The “sputum booth” should be positioned within view of the nurse’s station, but should be at least four meters away from the nearest building. Sputum should not be collected in patient toilets or consulting/counselling rooms. Details of an outdoor sputum booth are available in ANNEXURE 2.
In a mechanically ventilated healthcare facility, rooms having characteristics of airborne infection isolation rooms (AIIR) can be used for sputum collection. These rooms should be ventilated with 80 L per second per person of outside air or the requirements of the National Building Regulations, whichever is greater (SANS 10400 Part O, Table 2, as amended) and are to be maintained at negative pressure relative to the adjacent space, with a pressure differential in the order of -5 Pa. These rooms should preferably be served by full fresh air systems, or in the case of recirculating systems, the exhaust air should be HEPA filtered (EN1822 H13).
Special, purpose-built sputum booths, also referred to as Local Exhaust Ventilation (LEV) devices can also be used for sputum collection. These devices may be portable, where they are beneficial in multi-storey healthcare facilities, where a single sputum booth can be used for the whole facility. Details of a mechanically ventilated sputum booth are available in ANNEXURE 1.
A patient is seated in a chamber where he/she produces a sputum specimen. Fresh air, preferably filtered, is supplied overhead, and exhausted from the chamber at low level. The exhaust air is passed through an H13 HEPA filter to remove the airborne contaminant, and is passed back to the room. To ensure the chamber is safe for the next patient, a time-lag between one patient and the next should be calculated and stipulated, based on the validated clean-up rate of the sputum booth (SANS 14644-3). Downflow booths are preferred as this provides the most efficient contaminant removal. For reliable operation, downflow velocities of 0.35-0.45 m/s should be maintained in the booth with the door closed.
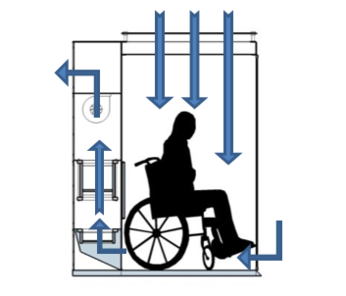
To ensure that AIIRs and LEVs operate as designed, a good maintenance plan is essential. This involves maintenance of pre-filters and HEPA filters, general ventilation maintenance, and standard daily checks to ensure downward and inward airflow is maintained. These checks are simple, and may be performed with incense sticks or smoke /vapour generating ventilation tubes. Maintenance is critical in LEVs, as failure to maintain the device operating as designed could result in contaminated air being passed into occupied zones. Since ducted UV lights can fail catastrophically without any indication, it is not recommended that the HEPA filters considered for LEV systems be substituted with only in-duct UV lights.
Where sputum collection or induction is performed, signage informing patients about the associated procedure should be considered. This should include:
- Instructions inside the sputum collection booth about the sputum collection procedure.
- Time-lags between patients producing a sputum specimen in the same booth.
- Reminders to healthcare workers to wear respirators in the sputum collection area.
Pharmacy
Pharmacist and assistants pharmacists are required to prepare and dispense medication, and manage medicine stock for inpatient and outpatients services. Refer to IUSS:GNS Pharmacy. The pharmacy may be responsible for community outreach programmes for community-based care and may be responsible for distributing medication to downstream referral facilities.
Laboratory services
Refer to IUSS:GNS Clinical and specialised diagnostic laboratory guidelines
Patient accommodation
Table 5: Patient accommodation cohorts for short-term accommodation
| Service type | Accommodation | Occupancy | Notes |
| Paediatric
(unisex) |
|||
| TB and MDR TB (female) | |||
| TB and MDR TB (male) | |||
| XDR (male/unisex) | |||
| XDR (female/unisex) | |||
| XDR paediatrics (unisex) | |||
| Former correctional services/(unisex isolation) | |||
| Psychiatric TB patients/ (unisex isolation) |
Clinical support services for inpatient care
Nursing support is to be located centrally to serve several bed functional units (for sub-acute services) or dedicated per unit for acute services to ensure supervision and control of the department. Alternatively if functional units are physically separate, these nursing support facilities are to be duplicated. In addition to the inpatient facilities described here, TB patients will need access to facilities described in 2.1 above either as a dedicated facility or where appropriate, shared with outpatients.
Duty station/ nurse’s station
The duty station should be provided with a built-in worktop (desk height), a telephone, computer and network points, cupboards and a clinical hand-wash basin.
Clean linen area
A locked linen store with slatted racks to support the airing and safe storage of clean linen should be provided.
Dirty utility room
The dirty linen store near the sluice and a dirty utility service door with direct access to waste collection points for easy removal and disposal. Space for separate refuse bins for paper, medical waste and general waste.
Sluice room
A standard sluice room with bedpan, urinal racks, storage cupboards and a worktop should be provided.
Surgery services (operating theatre)
Surgical services are commonly required by TB patients so should be readily available in nearby referral facilities or for stand-alone TB-services minor procedures room may be provided on site. Support infrastructure such as CSSD is required in accordance with.
Staff facilities
A cluster of staff facilities should be provided for exclusive use by staff. These include a lounge/tea area/room; a kitchen area/room; staff locker area/room and staff ablutions. Staff facilities should be located remotely from patient areas to allow for:
- airborne infection control
- a “break-away” venue to rest following patient contact periods away from the demands of the work environment
Staff facilities should be readily accessible to the duty areas. The purpose of this kitchen is to prepare beverages for members of the staff at tea breaks and lunch breaks, and to provide a place for washing and storing crockery and stocks of tea, coffee, sugar, milk and cleaning materials under lock and key. The kitchen area/room should be equipped with a sink, lock-up cupboards, bar fridge, and an instant boiling water dispenser (“Hydroboil” or similar approved).
Staff lockers should be provided for each non-central service member of staff for storing personal belongings.
Procedure room
The procedure room can be provided for the taking of blood and other specimens (except sputum). Clinical hand-wash basin with elbow taps to be provided. Work tops at standing height. Lock-up cupboards and a patient couch with good lighting. The electrocardiogram and the emergency trolley can be stored in this room.
Store rooms
Store rooms for provisions and consumables, surgical stores, equipment (such as wheelchairs, crutches and health technology) should be provided. These stores must be ventilated and fitted with shelves selected for appropriate storage of goods. Where electrical equipment is stored, electrical socket points may be required to ensure battery charging.
Medical store
A lockable room for store for the safekeeping of ward stock and scheduled drugs, infusions etc. is required. This must room must be cool (as close to 18 °C with passive means as possible), dry and dark (that is its electrical lighting should be independently controlled). It should be provided with a cabinet, worktop and adjustable shelving.
Matron’s office
The office should be a standard office with the normal requirements (desk, telephone, computer and network points, cupboards and a clinical hand-wash basin).
Mortuary
If a nearby referral healthcare establishment is available, a bier room may suffice. Alternatively a small mortuary may be provided. Refer to IUSS:GNS Mortuary.
Patient Support
Care should be taken to avoid enclosed congregate settings (such as waiting areas) where possible. Where these are required, they should be regarded as high risk for airborne contamination.
Visitor’s area
This area must be separate from the ward, should have a meeting room for several families, veranda and garden. Seating and tables must be built in. The visitor facility can be shared between male and female patients. Access control must be provided for visitors.
Visitor’s ablution
To be attached to visitor’s area. At least one unisex accessible toilet is to be provided.
Dining facilities
In acute settings, patients may be served meals in bed. A hall to accommodate patients is recommended in long-term care facilities. This room should provide tables and chairs for all patients, a small kitchenette, fridge, microwave, stove and an instant boiling water dispenser (“Hydroboil” or similar approved). These areas should have ample access to the outside. This room can be interlinked with games and TV rooms (if provided).
Business centre
This room should provide access to computers with Internet connectivity, space and chairs.
Resource centre/ media room/ library
This room should be like a small lounge providing space for books easy chairs and big table and chairs for occupational therapy activities.
Games room
This room should provide space for e.g. snooker, table tennis, and board games. This can be interlinked with other patient support areas (e.g. dining and TV room).
TV room
Separate from dining and games room, this room should have a TV, DVD and lounge suites. To be interlinked with Games and Dining Rooms.
Kitchenette
In addition to central kitchen services, an area may be provided in which patients can prepare their own meals and wash dishes. This area should be provided with a stove/oven, microwave, fridge, an instant boiling water dispenser (“Hydroboil” or similar approved), double sink, dishwasher. Lock-up cupboards and counter top working areas. Lock-up cupboards will provide store space for crockery and consumables.
Patient laundry
In addition to the central laundry services, provision may be made for a laundry for patient use only. This room should provide a washing machine and washing trough, and have direct access to a drying yard.
Other recreation
Patients are encouraged to spend much time outdoors during convalescence. Consideration should be made to providing pleasant garden and planting areas, possible vegetable gardens, and permanent weather-proof seats. An outdoor covered patio with braai facilities connected to dining area should be provided. An outdoor uncovered patio connected to the games/ TV room area may be provided. Storm-water management around the proposed building and affected grounds should be considered.
Allied healthcare services
National policy recognises the importance of have a holistic psycho-social approach to patient care. Therefor provision should be made for allied health services preferably by practitioners on site, visiting practitioners or, alternatively at a nearby referral facility. Refer to IUSS:GNS Adult rehabilitation services for further guidance.
Occupational therapy
Occupational therapists (OTs) and assistant OTs deliver a service to TB patients. It may be challenging to motivate patients especially when they are sick and are treated with many drugs, which have severe side effects. OT aims to increase skills by training in several crafts, cooking classes etc.
Audiology
Audiology services are required as a common side-effect of TB treatment is hearing loss. A baseline hearing test ought to be performed upon patient admission and followed up with regular tests to determine the effects of the drugs on hearing. If hearing is affected, drugs regimens can be adapted. Sharing of audiology equipment with referral facilities may be problematic as conventionally audio booths are enclosed to control noise and may be inadequately adapted for airborne infection risk. It is highly recommended that dedicated mobile audiometers which do not require booths (see KUDUwave, or equivalent) are secured for TB facilities. These can be supported by telemedicine so that reduced on-site involvement of audiologist is possible. Where the use of mobile audiometers is not possible or appropriate, it is recommended that the audiology test booth used be ventilated and flushed with fresh air for 20 minutes between uses.
Physiotherapy
Physiotherapists and assistant physiotherapists deliver services to patients as required. This typically includes lung function tests, mobility exercises and assistance in sputum production where patients have difficulty.
Clinical psychology
Clinical psychologist sees patients on an individual basis, have climate groups and supervise the six lay counsellors in their work.
Social services
Social workers assist patients with social and economic issues which include the obtaining of grants, identity documents and family counselling.
Support services
School
Provision of school services may be negotiated with the relevant Provincial Department of Basic Education. Separate teaching and learning facilities may be provided.
Kitchen
Kitchen services may be outsourced or prepared on site. Refer to IUSS: GNS Catering Services
Laundry
General laundry services can be provided on site, off site or can be shared (where co-located). Refer to IUSS:GNS Laundry and linen. In addition to general laundry services some TB institutions encourage patients to wash their own clothing. Where this is the case, hand washing, washing machine, drying machines and/or drying yards should be provided.
Facilities management
Waste management
On-site disposal, storage and collection of waste need consideration. Refer to IUSS:GNS Waste disposal.
Maintenance services - building
Building maintenance services for both planned and unplanned maintenance (for example works foreman, electrician, painter, plumber, and carpenter) will be needed to provide service on site either on a full-time, part time or visiting basis depending on the size of the facility and institutional arrangement. Maintenance workshops and storage space may be required for this.
Clinical engineering
Gardening services
Gardening and grounds maintenance services may be provided on-site or outsourced. It is recommended that planting and landscaping is arranged near to building openings to discourage loitering nearby for infection prevention and control.
Cleaning services
Cleaning services may be outsourced. However storage of cleaning equipment, materials and staff facilities for cleaners is required to be provided on site.
Administration
Office accommodation is to be provided in accordance with the following reference: Department of Public Works, 2005. Space planning norms and standards for office accommodation used by organs of state. (Government notice 1665). Cape Town South Africa: Government Gazette.
Other
Co-located institutions/ activities
Medical researchers, NGOs and other organisations may provide services to and be co-located with the facility.
Overnight stay
Family member overnight accommodation is not routinely provided but may be desirable, particularly in rural settings.
Commercial support (tuck shop, ATM)
Tuck shop facilities and banking services may be provided - if viable - on site for staff and patients. This is highly recommended as otherwise infectious patients leave the site in order to attend to these requirements.
Staff accommodation
Staff accommodation for nursing and or/clinical staff may be required by provincial policy, and may be recommended in most cases, especially in rural settings. Separation on site of staff quarters and patient facilities on site should allow for staff safety and privacy, whilst remaining within comfortable walking distance of the patient facilities. Refer to IUSS:GNS Health facility residential
Case studies
List of case studies
- Areas comparison of long-term XDR TB care facilities at:
- Bongani Hospital, Mpumalanga
- Tshepong Hospital, North West
- Modimolle Hospital, Limpopo
- Modimolle TB Hospital
- site layout
- patient rooms
- natural ventilation design
- Catherine Booth TB Hospital, KwaZulu-Natal
- Roof ventilation and windows concept drawings
- Two-bed patient rooms plan
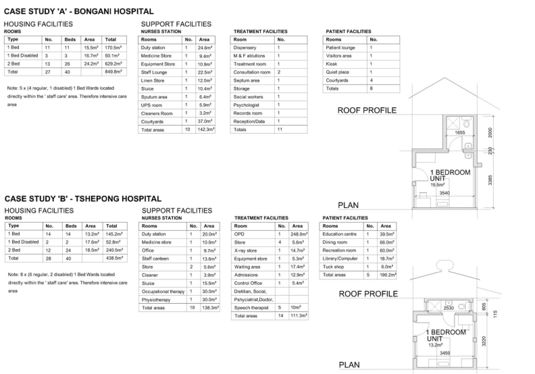
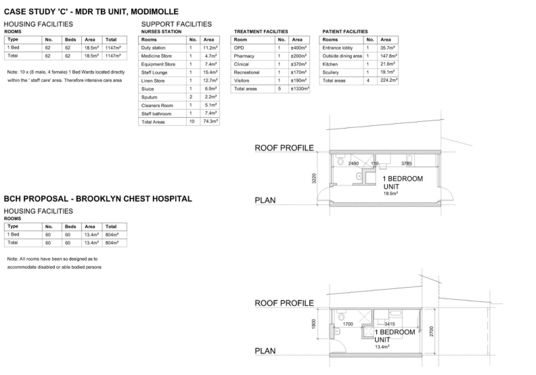

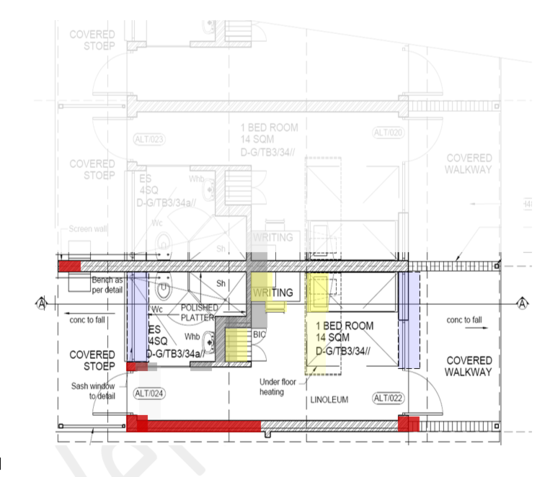
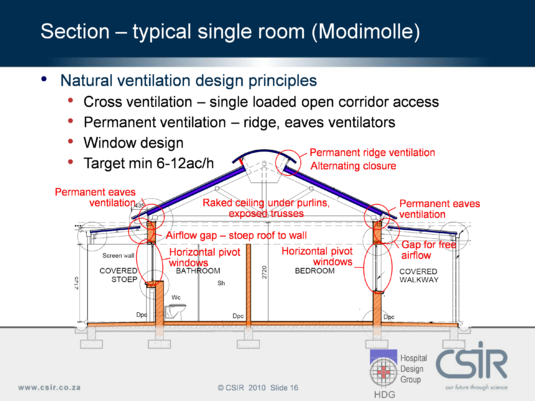
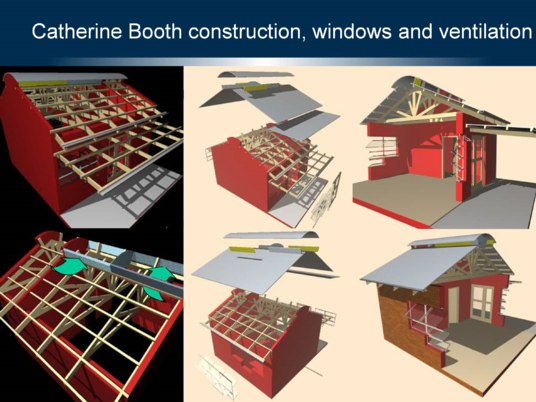
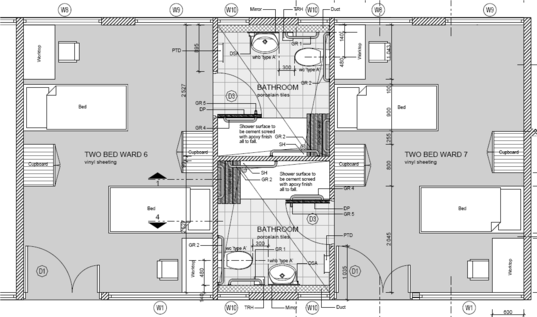
Bibliography
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 2004. ANSI/ASHRAE standard 55-2004 Thermal environmental conditions for human occupancy. Atlanta USA: ASHRAE.
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 1999. ANSI/ASHRAE standard 52.2-1999 Method of testing general ventilation air cleaning devices for removal efficiency by particle size. Atlanta USA: ASHRAE.
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 1989. ASHRAE standard 62 Ventilation for acceptable indoor air quality. Atlanta USA: ASHRAE.
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 2003. HVAC design manual for hospitals and clinics. Atlanta USA: ASHRAE.
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), 2009. ANSI/ASHRAE/ASHE standard 170-2008 ventilation of health care facilities. Atlanta USA: ASHRAE.
Basu, S., Andrew ,J.R., Poolman, E.M., Gandhi, N.R., Shah, N.S., Moll, A., Moodley, P., Galvani, A.P. and Friedland, G.H, 2007. Prevention of nosocomial transmission of extensively drug-resistant tuberculosis in rural South African district hospitals: an epidemiological modelling study. Lancet, 370(9597), pp. 1500 - 1507.
Behrman, A., Buchta, W.G., Budnick, L.D., Hodgson, M.J., Raymond, L.W., Russi, M., Spillmann, S.J. and Swift, M.D., 2013. Protecting health care workers from tuberculosis. Journal of Occupational and Environmental Medicine, 55(8), pp.985-988.
British Standards Institution (BSI), 2009. EN 1822-1:2009 High efficiency air filters (EPA, HEPA and ULPA) Classification, performance testing, marking. London: BSI.
British Standards Institution (BSI), 2009. EN 1822-2:2009 High efficiency air filters (EPA, HEPA and ULPA): Aerosol production, measuring equipment, particle counting statistics. London: BSI.
British Standards Institution (BSI), 2009. EN 1822-3:2009 High efficiency air filters (EPA, HEPA and ULPA) Testing flat sheet filter media. London: BSI.
British Standards Institution (BSI), 2009. EN 1822-4:2009 High efficiency air filters (EPA, HEPA and ULPA): Determining leakage of filter elements (scan method). London: BSI.
Brown G.Z. and Huang L. Natural Ventilation in Northwest Buildings [Journal] // ASHRAE Journal 48(1). - 2006. - 48. - pp. 47-52.
Brown, G.Z. and Huang, L. 2006. Natural ventilation in Northwest buildings. ASHRAE Journal, 48, pp. 47-52.
Carroll, K.B., Secombe, C.J. and Pepys, J., 1976. Asthma due to non-occupational exposure to toluene (tolylene) di-isocyanate. Clinical Allergy, 6(2), pp.99–104.
Centers for Disease Control and Prevention (CDC), 1990. Guidelines for preventing the transmission of mycobacterium tuberculosis in health-care Settings, with special focus on HIV-related issues. (Morbidity and Mortality Weekly Report (MMWR) Vol. 39 No. RR-17). Atlanta, GA: CDC.
Centers for Disease Control and Prevention (CDC), 2005. Guidelines for preventing the transmission of mycobacterium tuberculosis in health-care settings. (Morbidity and Mortality Weekly Report (MMWR) Vol. 54 No. RR-17). Atlanta, GA: CDC.
Centres for Disease Control and Prevention (CDC), 2013. Fact sheet: TB elimination: Extensively drug-resistant tuberculosis (XDR TB). [online] Available at: http://www.cdc.gov/tb/publications/factsheets/drtb/xdrtb.pdf [Accessed 21 January 2014].
Chartered Institution of Building Services Engineers (CIBSE), 1997. CIBSE applications manual AM10 natural ventilation in non-domestic buildings. London: CIBSE.
Chartered Institution of Building Services Engineers (CIBSE), 2000. CIBSE applications manual AM13 mixed mode ventilation. London: CIBSE.
Culver, D.A, Gordon, S.M. and Mehta, A.C., 2003. Infection control in the bronchoscopy suite: a review of outbreaks and guidelines for prevention. American Journal of Respiratory and Critical Care Medicine; 167(8), pp.1050-6.
Department of Health and Human Services (DHHS) and National Institute for Occupational Safety and Health (NIOSH), 2009. Environmental control for tuberculosis: Basic upper-room ultraviolet germicidal irradiation guidelines for healthcare settings. Atlanta, GA: DHHS.
Department of Public Works, 2005. Space planning norms and standards for office accommodation used by organs of state. (Government notice 1665). Cape Town South Africa: Government Gazette.
Dugger, C.W., 2008. In South Africa, TB patients behind barbed wire. The New York Times, [online] 24 March. Available at: http://www.nytimes.com/2008/03/24/world/africa/24iht-saf.4.11377837.html?pagewanted=all&_r=0 [Accessed 26 March 2014].
First, M.W., Nardell, E.A., Chaisson, W. and Riley, R., 1999. Guidelines for the application of upper-room ultraviolet germicidal irradiation for the prevention of airborne contagion- part I: Basic principles. ASHRAE Transactions 105(1).
First, M.W., Nardell, E.A., Chaisson, W. and Riley, R., 1999b. Guidelines for the application of upper-room ultraviolet germicidal irradiation for the prevention of airborne contagion- part II: Design and operation guidance. ASHRAE Transactions 105(1).
Gandhi, N.R., Shah, N.S., Andrews, J.R., Vella, V., Moll, A.P., Scott, M., Weissman, D., Marra, C., Lalloo, U.G., and Friedland, G.H. and Tugela Ferry Care and Research Collaboration, 2010. HIV coinfection in multidrug and extensively drug-resistant tuberculosis results in high early mortality. American Journal of Respiratory and Critical Care Medicine, 181(1),pp.80-86.
Hamilton, K. and Yau, J., 2004. The global tug-of-war for health care workers. Washington USA: Migration Policy Institute. Available at: http://www.migrationinformation.org/feature/display.cfm?ID=271 [Accessed 4 February 2014].
Hinds, W.C., 1999. Aerosol technology: Properties, behaviour and measurement of airborne particles.2nd ed. New York: John Wiley & Sons.
International Organisation for Standardisation (ISO), 2005. ISO 14644-3 Cleanrooms and associated controlled environments - Part 3: Test methods. Switzerland: ISO.
International Radiation Protection Association (IRPA), 1985. Guidelines on Limits of Exposure to Ultraviolet Radiation of Wavelengths between 180 nm and 400 nm (Incoherent Optical Radiation). Health Physics, 39, pp. 331–340.
Joshi, R., Reingold, A.L., Menzies, D., and Pai, M., 2006. Tuberculosis among health-care workers in low- and middle-income countries: A systematic review. PLoS Medicine, 3(12).
Ko Gwangpyo, First Melvin W and Burge Harriette A The Characterization of Upper-Room Ultraviolet Germicidal Irradiation in Inactivating Airborne Microorganisms [Journal] // Environmental Health Perspectives - Harvard School of Public Health. - Boston : EBSCO, January 2002. - 1 : Vol. 110. - pp. 95-101. - Harvard School of Public Health.
Ko, G., First, M.W. and Burge, H.A., 2002. The characterization of upper-room ultraviolet germicidal irradiation in inactivating airborne microorganisms. Environmental Health Perspectives, 110(1), pp.95- 101.
Lawn, S.D., Bekker, L.G., Middelkoop, K., Myer, L. and Wood, R., 2006. Impact of HIV infection on the epidemiology of tuberculosis in a peri-urban community in South Africa: the need for age-specific interventions. Clinical Infectious Diseases, 42(7), pp.1040-1047.
London, L., 2009. Confinement for extensively drug-resistant tuberculosis: balancing protection of health systems, individual rights and the public’s health. International Journal of Tuberculosis and Lung Disease, 13(10), pp.1200-9.
Menzies, D., Joshi, R., Pai, M., 2007. Risk of tuberculosis infection and disease associated with work in health care settings. The International Journal of Tuberculosis and Lung Disease. 11(6), pp.593-605.
Molhave, L., 1987. The sick buildings-A subpopulation among the problem buildings. In: Seifert, B.; Esdorn, H.; Fischer, M.; Rueden, H.; Wegner, J., eds. Indoor Air ’87, 4th international conference on indoor air quality and climate. West Berlin Germany, August 1987. Berlin Germany: Institute for water, soil and hygiene.
Molhave, L., Bach, B. and Pedersen, O.F., 1986. Human reactions to low concentrations of volatile organic compounds. Environment International, 12(1-4), pp.167–175.
Morey, P.R., Hodgson, M.J., Sorenson, W.G., Kullman, G.J., Rhodes, W.W. and Visvesvara, G.S., 1984. Environmental studies in moldy office buildings: Biological agents, sources and preventive measures. In: Annual American conference of governmental industrial hygiene, Vol. 10, 1984, pp.21-35.
Naidoo, S. and Jinabhai, C.C., 2006. TB in health care workers in KwaZulu-Natal, South Africa. The International Journal of Tuberculosis and Lung Disease, 10(6),pp.676-682.
Nardell, E.A., 1995. Interrupting transmission from patients with unsuspected tuberculosis: a unique role for upper room ultraviolet air disinfection. American journal of Infection Control, 23(2),pp.156 64.
National Department of Health (NDoH), 2007. The draft national infection prevention and control policy for TB, MDRTB and XDRTB. South Africa: NDoH.
National Department of Health, 2007. Management of drug-resistant tuberculosis: Policy guidelines. [pdf] South Africa: NDoH. Available at: http://www.search.gov.za [Accessed 26 March 2014].
National Department of Health, n.d. Tuberculosis strategic plan for South Africa, 2007-2011. [pdf] South Africa: NDoH. Available at: http://www.search.gov.za/info/search.jsp. [Accessed 26 March 2014].
National Institute for Occupational Health and Safety (NIOSH) and U.S Department of Health, Education and Welfare, 1972. Occupational exposure to ultraviolet radiation. [pdf] Atlanta, GA: Department of Health, Education and Welfare. Available at: http://www.cdc.gov/niosh/pdfs/7311009a.pdf [Accessed 26 March 2014].
Parsons, S.A., Abbott, G.R., De Jager, P., Conradie, D.C.U. and Bole, S., 2010. Researched solutions for long-term accommodation units for drug-resistant tuberculosis patients in South Africa. In: CSIR, Science real and relevant conference. CSIR International Convention Centre Pretoria, South Africa, 2010. Pretoria: CSIR.
Price Waterhouse Coopers LLP in association with the University of Sheffield and Queen Margaret University College Edinburgh, 2004. The role of hospital design in the recruitment, retention and performance of NHS nurses in England. [pdf] Belfast UK: Commission for Architecture and the Built Environment (CABE). Available at: http://webarchive.nationalarchives.gov.uk/20110118095356/http:/www.cabe.org.uk/files/the-role-of-hospital-design-appendices.pdf [Accessed 13 February 2014].
Riley, R.L, Mills, C.C, O’Grady, F., Sultan, L.U., Wittstadt, F. and Shivpuri, D.N., 1962. Infectiousness of air from a tuberculosis ward. Ultraviolet irradiation of infected air: comparative infectiousness of different patients. The American Review of Respiratory Disease, 85, pp.511-25.
Riley, R.L. and Nardell, E.A., 1989. Clearing the air: The theory and application of ultraviolet air disinfection. The American Review of Respiratory Disease, 139(5), pp.1286– 1294.
Riley, R.L. and O’Grady, F., 1961. Airborne infection: Transmission and control. New York USA: The Macmillan Company.
Riley, R.L., 1974. Airborne infection. The American Journal of Medicine, 57, pp.466-475.
Riley, R.L., Knight, M. and Middlebrook, G., 1976. Ultraviolet susceptibility of BCG and virulent tubercle bacilli. The American Review of Respiratory Disease, 113(4), pp.413–418.
Samet, J.M., Marbury, M.C. and Spengler, J.D., 1988. Health effects and sources of indoor air pollution. Part II. The American Review of Respiratory Disease, 137(1), pp.221–242.
Sanjaya, N.S. and Mark, J.F., 2004. Detention for tuberculosis: public health and the law. Medical Journal of Australia, 180(11), pp.573–576.
Singh, J.A., Upshur, R., and Padayatchi, N., 2007. XDR-TB in South Africa: No time for denial or complacency. PLoS Medicine, 4(1). January 2007; 4(1), 19-25.
Singh, T, van Reenen, T, de Jager, P, Poluta, M, Stoltz, A, 2015. UVGI Disinfection Of Room Air: An Evidence Based Guideline for Design, Implementation and Maintenance, Available at: http://www.tb-ipcp.co.za/index.php/tools-resources/documents-paper-and-articles [Accessed 26 Aug 2015]
South African Bureau of Standards, 2011. SANS 10400-O:2011 The application of the national building regulations Part O: Lighting and ventilation. Pretoria South Africa: SABS Standards Division.
Southern African Legal Information Institute (SAFLII), 2008. Minister of health of the province of the Western Cape v Goliath and others. (Case number 13741/07). [pdf] Cape Town: SAFLII. Available at http://www.saflii.org/za/cases/ZAWCHC/2008/41.pdf [Accessed 27 March 2014].
The Occupational Health and Safety Act 1993. s.8(1). Cape Town South Africa: Government Gazette.
The South African Pharmacy Council, 2010. Good pharmacy practise in South Africa. 4th ed. Arcadia Pretoria: South African Pharmacy Council.
Ulrich, R.S., Zimring, C., Zhu, X., DuBose, J., Seo, H.B., Choi, Y.S., Quan, X. and Joseph, A., 2008. A review of the research literature on evidence-based healthcare design. Health Environments Research & Design, 1(3), pp.61-125.
WHO Natural Ventilation for Infection Control in Health-Care Settings [Book]. - 2009.
World Health Organisation (WHO), 2008. Intergrated health services- what and why? (Technical brief No. 1.). Geneva: WHO.
World Health Organisation (WHO), 2009a. Natural ventilation for infection control in health-care settings [pdf] Geneva Switzerland: WHO Press. Available at: http://whqlibdoc.who.int/publications/2009/9789241547857_eng.pdf [Accessed 13 February 2014].
World Health Organisation (WHO), 2010. Workload indicators of staffing need: User’s manual. Geneva: WHO.
World Health Organisation (WHO), 2013. Global tuberculosis report. Geneva: WHO.
Xu Peng [et al.] Efficacy of ultraviolet germicidal irradiation of upper-room air in inactivatingairborne bacterial spores and mycobacteria in full-scale studies [Journal] // Athmospheric Environment 37. - 2003. - pp. 405-419.
Xu, P., Peccia, J., Fabian, P., Martyny, J.W., Fennelly, K.P., Hernandez, M. and Miller, S.L., 2003. Efficacy of ultraviolet germicidal irradiation of upper-room air in inactivating airborne bacterial spores and mycobacteria in full-scale studies. Atmospheric Environment, 37 (2003), pp.405–419.
Abbreviations
| ACGIH | American Conference of Governmental Hygienists |
| ACH | Air changes per hour |
| AIA | American Institute of Architects |
| AIIR | Airborne infection isolation room |
| ASHRAE | American Society of Heating, Refrigerating and Air-Conditioning Engineers |
| CDC | Centers for Disease Control and Prevention (US agency) |
| CSIR | Council for Scientific and Industrial Research |
| CSSD | central sterile supply department |
| DR | drug-resistant |
| DR TB | drug-resistant TB |
| EIA | environmental impact assessment |
| IAQ | indoor air quality |
| ICT | information communications technology |
| IPC | infection prevention and control |
| IRPA | International Radiation Protection Agency |
| LEV | local exhaust ventilation |
| MDR TB | multi-drug-resistant TB |
| NDoH | National Department of Health |
| NGO | non-governmental organisation |
| NHLS | National Health Laboratory Service (SA agency) |
| NHI | National Health Insurance |
| NIOSH | National Institute of Occupational Safety and Health (US agency) |
| OHS | occupational health and safety |
| OPD | outpatient department |
| OT | occupational therapy / occupational therapist |
| PAC | Portable air cleaner |
| PHC | primary healthcare |
| PMV | predicted mean vote |
| PPE | personal protective equipment |
| QASA | Quadra-para Association of South Africa |
| REL | recommended exposure limit |
| RH | relative humidity |
| RSE | relative spectral effectiveness |
| SAHNORMS | South African hospital norms |
| SDP | site development plan |
| TB | tuberculosis |
| TLV | threshold limit values |
| UVA | ultraviolet “A” (wavelength 400 nm–315 nm) |
| UVB | ultraviolet “B” (wavelength 315 nm–280 nm) |
| UVC | ultraviolet “C” (wavelength 280 nm–100 nm) |
| UVGI | ultraviolet germicidal irradiation |
| WHO | World Health Organisation |
| XDR TB | extreme (or extensively) drug-resistant TB |
Annexure 1. Indoor sputum booth
Application
This document contains a set of drawings and specifications presenting prototype concept of a Sputum Booth developed at the CSIR. These are intended for the clinical applications. Further information can be obtained from the Architectural Engineering Group of the Building Scient and Technology Unit of the CSIR.
Background
This document presents technical drawings and specifications of the concept a sputum induction and collection booth designed for TB infection control in clinical settings. The prototype was developed by the Architectural Engineering Group, Building Science & Technology Programme, Division of Built Environment, CSIR. The development process of this facility was described in a separate report: “Development of a prototype of the Sputum Booth; CDC project”, November 2013.
The related work was carried out in terms of the international research project funded by the Centre for Disease Control (CDC).

Suggestions improvements on concept booth
Upon the completion of the prototype unit, a few areas were identified for further improvements. These relate to the following:
- The mass of the unit is still too high for safe and resiliant transport. Solutions for weight reduction should be soughtExternal fold away handels could be included in the design for easier handling of the unit.
- The overall length of the booth could be reduced by about 150 mm. This would still provide enough space to accommodate a person in a wheelchair.
- The costs and mass of future units could be reduced by replacing the aluminium sandwich panelling with polymer sheeting
- The fan-filter unit could be constructed such that is an integral structural component of the booth, reducing size and weight of the overall unit.
- Incorporating an additional flexible one-way membrane behind the screen of the pre filter would limit the reversed airflow back into the booth when the booth is non-operational or during transportation.
Arduino wiring code for door interlock timer
/*Begin*/
/*
Sputum booth door lock control Sample code 08/11/2013
Written by: Tobias van Reenen (CSIR)
This Arduino Uno sketch controls a 12V magnetic door lock for a mechanically ventilated sputum booth
The door in this sketch remains normally locked and is released on the press of the external and internal door release buttons
The internal door release button will always unlock the door while the external button will only release the door after it has remained locked
for the predetermined length of time. This is in order to allow the booth ventilation system to adequately flush the booth between occupants.
The following wiring connections are made:
Arduino________Interface
GND ------------------ gnd
5.0v------------------ Vcc
Magnet power---------- +12V & -12V
8 -------------------- Release Button (Internal)
9 -------------------- Unlock Button (External)
10 ------------------- Unlock LED (Green)
11 ------------------- Locked LED (Red)
12 ------------------- Door Magnet Relay
*/
//Initiate variables
int doorLOCK = 12; //5v relay pin, switching 12V Magnet
int lockedLED = 11; //redLED
int unlockLED = 10; //greenLED
int unlockButton = 9; //External Button requesting an door unlock. Cannot override timer --requires 10k pull-up resistor & 5V Vcc
int releaseButton = 8; //Internal button requesting a door release. Overrides timer --requires 10k pull-up resistor & 5V Vcc
float unlockDELAY = 3000; //3 seconds
float lockDELAY = 30000; //30 seconds
float unlockTimeStamp;
float lockTimeStamp;
int pressed = 0;
int unpressed = 1;
int UNLOCK = 1;
int LOCK = 0; //using normally closed relay config
int ON = 1;
int OFF = 0;
void setup() {
pinMode(doorLOCK,OUTPUT);
pinMode(lockedLED,OUTPUT);
pinMode(unlockLED,OUTPUT);
pinMode(unlockButton,INPUT);
pinMode(releaseButton,INPUT);
Serial.begin(9600);
Serial.println("restart");
digitalWrite(unlockLED,OFF);
digitalWrite(lockedLED,ON);
}
void loop() {
Serial.print("unlock: ");
Serial.print(digitalRead(unlockButton));
Serial.print(" release: ");
Serial.print(digitalRead(releaseButton));
Serial.print(" unlockLED: ");
Serial.println(digitalRead(unlockLED));
if (digitalRead(releaseButton) == pressed){ //check for release button press
while (digitalRead(releaseButton) == pressed){ //holds code until button released
unlockDOOR(); // unlock door function
}
}
if (digitalRead(unlockButton) == pressed){ //check for unlock button press
if (digitalRead(unlockLED) == ON){ //only unlocks door if unlock LED is lit
while (digitalRead(unlockButton) == pressed){//holds code until button released
unlockDOOR();
}
} //unlock door function
}
if (millis()> (unlockTimeStamp+unlockDELAY)){ //counts down unlock delay and then locks door again
Serial.print("CountDown: "); Serial.println((lockDELAY+unlockTimeStamp+unlockDELAY-millis())/1000);
if ((digitalRead(unlockButton) == unpressed)&&(digitalRead(releaseButton) == unpressed)){
if (digitalRead(doorLOCK)!=LOCK){ //checks for unlock button hold before locking door
lockDOOR(); //lock door function
}
}
}
if (millis()> (lockTimeStamp+lockDELAY)){
digitalWrite(unlockLED, ON);
}
}
void unlockDOOR(){
Serial.println("unlocking...");
unlockTimeStamp = millis(); // initiate unlock counter
digitalWrite(lockedLED,OFF);
digitalWrite(unlockLED,OFF);
digitalWrite(doorLOCK,UNLOCK);
}
void lockDOOR(){
Serial.print("locking... ");
lockTimeStamp = millis();
digitalWrite(doorLOCK,LOCK);
digitalWrite(lockedLED,ON);
digitalWrite(unlockLED,OFF);
Serial.print("unlockLED: ");
Serial.println(digitalRead(unlockLED));
}
/*end*/
Drawings
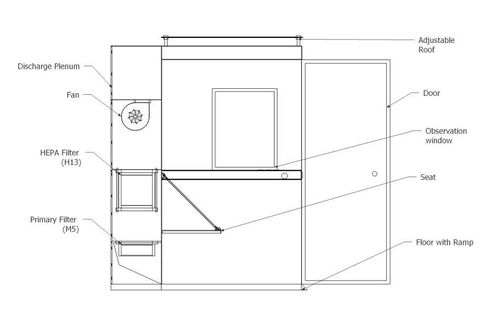
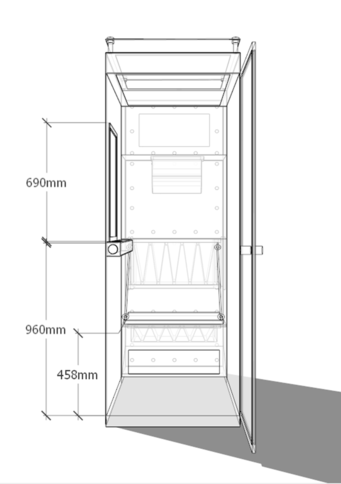

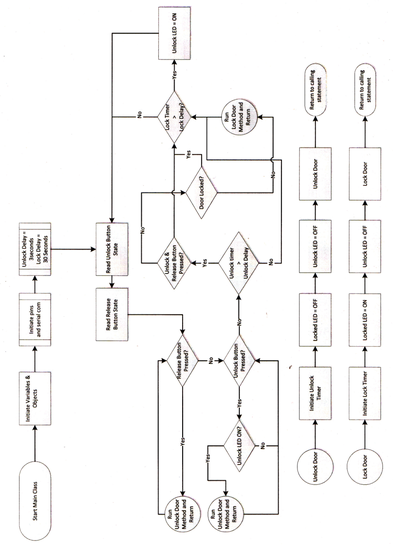
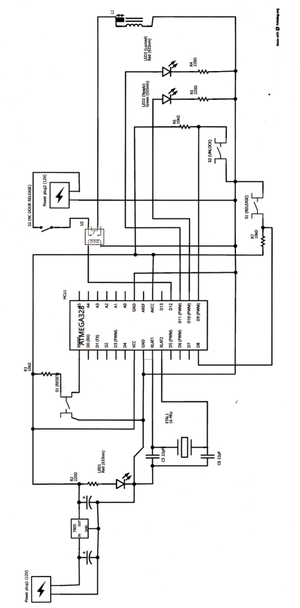
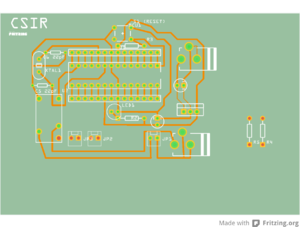
Annexure 2. Pre-fabricated outdoor sputum booth
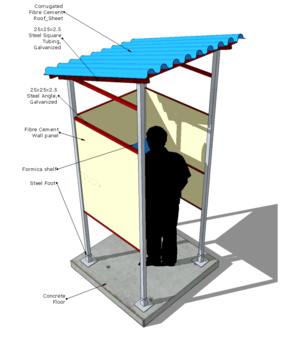
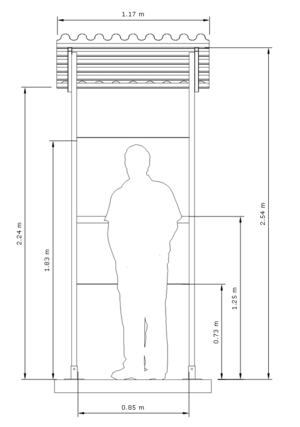
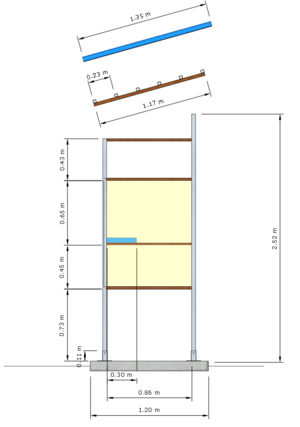
Annexure 3. Brickwork outdoor sputum booth