Adult Inpatient Services: Difference between revisions
mNo edit summary |
→Airborne infection isolation and protective environments: Changes made to burns unit requirements - negative pressure permitted as per BES guide |
||
| (128 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
= | ='''Policy and Service Context'''= | ||
==Policy context== | |||
<div style="margin-left:0;margin-right:0cm;"> | |||
Adult inpatient units provide suitable accommodation for the patient where diagnosis, medical and nursing care, and treatment can be provided effectively and economically. | |||
The adult inpatient unit is the clinical unit in a hospital where patient bed space and clinical treatment space is combined. This combination allows the unit to provide patients with an effective, economical therapeutic unit for clinical diagnosis, medical treatment, and nursing care. | The adult inpatient unit is the clinical unit in a hospital where patient bed space and clinical treatment space is combined. This combination allows the unit to provide patients with an effective, economical therapeutic unit for clinical diagnosis, medical treatment, and nursing care. | ||
The inpatient unit environment needs to meet the requirements for safe nursing and clinical practice, adhere to health and safety standards, and meet recognised infection control principles, while maintaining the principle of patient privacy and dignity. | The inpatient unit environment needs to meet the requirements for safe nursing and clinical practice, adhere to health and safety standards, and meet recognised infection control principles, while maintaining the principle of patient privacy and dignity. | ||
This document provides guidance on inpatient unit spaces and it should be read in conjunction with the full IUSS set of standards pertaining to an inpatient unit. Variations to the set standard for inpatient units will be noted where indicated. | This document provides guidance on inpatient unit spaces and it should be read in conjunction with the full IUSS set of standards pertaining to an inpatient unit. Variations to the set standard for inpatient units will be noted where indicated. | ||
Specialised guidelines for inpatient units for paediatrics, infectious diseases, i.e. tuberculosis, intensive care, obstetrics, rehabilitation, burns care, oncology and mental health care will be addressed in separate IUSS documents. | Specialised guidelines for inpatient units for paediatrics, infectious diseases, i.e. tuberculosis, intensive care, obstetrics, rehabilitation, burns care, oncology and mental health care will be addressed in separate IUSS documents. | ||
The business case and the health brief define the correct package of services and the required bed distribution per facility based on the Provincial Strategic Transformation Plan and the government policy document:Government Notice R. 185, 2 March 2012, National Health Act 61/2003Regulations: '''Categories of hospitals''': No.35101 | ==Service context== | ||
</div>The business case and the health brief define the correct package of services and the required bed distribution per facility based on the Provincial Strategic Transformation Plan and the government policy document:Government Notice R. 185, 2 March 2012, National Health Act 61/2003Regulations: '''Categories of hospitals''': No.35101 | |||
Table 1: Inpatient unit allocation per category of hospitalL | |||
{| class="wikitable" | {| class="wikitable" | ||
!District hospital | !District hospital | ||
!Regional hospital | !Regional hospital | ||
| Line 81: | Line 80: | ||
| | | | ||
|} | |} | ||
'''<nowiki>*To be dealt with in separate documents </nowiki>''' | '''<nowiki>*To be dealt with in separate documents </nowiki>'''<div style="margin-left:0;margin-right:0cm;"> | ||
===Determining inpatient unit size=== | |||
=== | Operationally successful inpatient units range from 28 to 32 beds per unit. The unit is subdivided into bed units that will provide for efficient management of patient acuity and flexibility. This guideline recommends 28 to 32 beds per inpatient unit. | ||
All inpatient units should function as stand-alone units. These units contain one, two or four bed-, with six-bed configurations only being permissible in certain instances. | All inpatient units should function as stand-alone units. These units contain one, two or four bed-, with six-bed configurations only being permissible in certain instances. | ||
The inpatient unit should be planned to operate at an optimal occupancy level considering the model of care to be provided, staffing strategies, staff availability and operational aspects. | The inpatient unit should be planned to operate at an optimal occupancy level considering the model of care to be provided, staffing strategies, staff availability and operational aspects.- <div style="margin-left:0cm;margin-right:0cm;"> | ||
< | ===Hours of operation=== | ||
=== | |||
<div style="margin-left:0cm;margin-right:0cm;">All inpatient units and emergency admissions will operate 24 hours a day, seven days a week. Day patients will be treated for 8 or 12 hours a day or as stipulated in the health brief. </div> | <div style="margin-left:0cm;margin-right:0cm;">All inpatient units and emergency admissions will operate 24 hours a day, seven days a week. Day patients will be treated for 8 or 12 hours a day or as stipulated in the health brief. </div> | ||
=== | ===Patient visitors=== | ||
<div style="margin-left:0cm;margin-right:0cm;">The hospital determines the visiting policy. Patient visitors may be limited by age, number and allocated visiting times. </div> | <div style="margin-left:0cm;margin-right:0cm;">The hospital determines the visiting policy. Patient visitors may be limited by age, number and allocated visiting times. </div> | ||
=== | ===Personnel=== | ||
<div style="margin-left:0cm;margin-right:0cm;">Each unit will be assigned nursing and housekeeping staff for a 24-hour operational cycle. Nursing staff work in shifts and provide day and night nursing support. Medical and clinical support staff members provide clinical interventions according to the clinical profile of the inpatient unit and the need of the individual patient. | <div style="margin-left:0cm;margin-right:0cm;">Each unit will be assigned nursing and housekeeping staff for a 24-hour operational cycle. Nursing staff work in shifts and provide day and night nursing support. Medical and clinical support staff members provide clinical interventions according to the clinical profile of the inpatient unit and the need of the individual patient. | ||
Facility management, such as food services, linen services, cleaning services and maintenance support, is performed on a daily, weekly or intermittent basis. | |||
Visiting, teaching and volunteering activities may also take place within the inpatient unit space. | |||
</div> | |||
===Operational policies=== | |||
<div style="margin-left:0cm;margin-right:0cm;">Operational policies influence the planning, design and functioning of an adult inpatient facility and must be considered early in the design process. The national and provincial departments of health prescribe operational and clinical policies in the interest of quality of care and infection control. All individual facilities will also have their own policies and procedures to be accommodated in the planning of a new facility or upgrading of an existing facility. | |||
The following policies are relevant to inpatient units: | |||
<div style="margin-left:0cm;margin-right:0cm;">Operational policies influence the planning, design and functioning of an adult inpatient facility and must be considered early in the design process. The national and provincial departments of health prescribe operational and clinical policies in the interest of quality of care and infection control. All individual facilities will also have their own policies and procedures to be accommodated in the planning of a new facility or upgrading of an existing facility. | </div> | ||
{| style="border-spacing:0;width:12.555cm;" | {| style="border-spacing:0;width:12.555cm;" | ||
|- style="border:none;padding-top:0.044cm;padding-bottom:0cm;padding-left:0cm;padding-right:0cm;" | |- style="border:none;padding-top:0.044cm;padding-bottom:0cm;padding-left:0cm;padding-right:0cm;" | ||
| Line 151: | Line 147: | ||
|- | |- | ||
|} | |} | ||
='''Planning and Design'''= | |||
= | ==Overview== | ||
Adult inpatient units provide suitable accommodation for the patient where diagnosis, medical and nursing care, and treatment can be provided effectively and economically | |||
This document attempts to illustrate the desired planning principles and design considerations for adult inpatient units. | |||
Part B contains planning and design guidance, design considerations, functional relationships between hospital departments with respect to adult inpatient accommodation (inpatient units), and relationships within the inpatient unit itself. | |||
Workflow diagrams are provided to explain the flow of patients, clinical staff, support goods and services, maintenance staff, as well as the public. Workflow diagrams within departments are provided to assist in understanding the intradepartmental relationships that support the functional flow in the inpatient unit to ensure productive service delivery. | |||
The detailed room diagrams with accompanied norms and standards are provided to clarify understanding of the different space requirements and room specific specifications for an adult inpatient unit. | |||
<div style="margin-left: | ==Design and planning principles== | ||
<div style="margin-left:0cm;margin-right:0.654cm;">Hospital design principles are dealt with in a separate IUSS document and must be read in conjunction with this document when planning adult inpatient units. </div> | |||
===General design and planning principles=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0.654cm;">The following planning principles need to be emphasised: | ||
*Inpatient accommodation forms the core of a hospital and has functional relationships with most departments | |||
*Patients enter the facility as inpatients, day patients or outpatients. | |||
*The planning of the inpatient units should support planning principles that promote a holistic healing environment with, where possible, clear external views, consideration of noise levels, natural ventilation, as much morning sun or light as possible, and spaces that would create a pleasant healing environment. | |||
*The design should reduce noise in the facility | |||
*The design should make maximum use of natural light and views for patients and staff. | |||
*The healthcare patient environment should be clinically safe and effective. | |||
*The design should maximise patient safety and reduce the risk of errors and accidents. | |||
*The work environment should be ergonomically safe and risk free. | |||
*The design should avoid large sprawling layouts that are both resource and cost intensive. | |||
*Workflow should be efficient and support effective resource utilisation. | |||
*Appropriate space norms and room design should be implemented. | |||
*The unit should comply with quality assurance principles. | |||
*The unit should have communication and information systems that will support patient management and administration. | |||
*Layouts should reflect the service needs of the patients in the inpatient unit. | |||
*Beds should be clustered to facilitate staff efficiency, meal relief and optimal patient supervision, particularly at night when staffing levels are lower. | |||
*The design should facilitate the delivery of care at the patient’s bedside or be proximal to the bedside whenever possible. This includes suitable services and supplies at the bedside. | |||
*The environment should be aesthetically pleasing for patients and should assist staff in performing the required activities in the most efficient and supportive environment. | |||
*Staff should not have to walk far to obtain supplies and equipment. | |||
*The design should balance requirements for clinical need, and capital and recurrent budget considerations. | |||
*The orientation of the inpatient units and aspect of inpatient accommodation should be prioritised in the development of the master plan. The orientation of the inpatient units should preferably face north or northeast, but a southern orientation is acceptable. | |||
*If the prevailing wind direction is south, east and west orientations of inpatient units are discouraged. | |||
*The placement of inpatient units must ensure patient privacy. Visitors, staff and service traffic through the inpatient units should be avoided. | |||
*Inpatient units can be organised on the same level over a large floor area or they may be stacked into a multistorey block separate from diagnostic and treatment facilities, but closely linked. This allows more consistent planning of inpatient accommodation, increases flexibility in the way that beds can be organised, and enables maintenance and refurbishment to be carried out more easily. | |||
*All pipes for sanitary requirements should be placed on external walls. Service support facilities and top-up of stores or pharmaceuticals and food delivery should be accessible to the inpatient units without compromising privacy or noise levels. | |||
*The design should enable greater levels of observation in response to increased patient acuity. | |||
*There should be enough space for activity at the bedside and other activities in the inpatient unit. | |||
*There should be adequate storage space for bulky equipment. | |||
*The area should be accessible to physically and sensory impaired people. | |||
*The design should that make it possible to communicate administrative or clinical information from the bedside. | |||
*The design should consider staff members’ and patients’ privacy for clinical treatment, bodily functions, personal care, and personal discussions and telephone calls</div>The planners of the required space should ask the following questions: | |||
*Personnel – How many people are there at any given time in a specific place to perform a specific task or procedure? | |||
*Activities – What procedures should be performed? | |||
*Equipment – What equipment is required that will occupy the space? | |||
*Security – What access control measures does the hospital management determine? | |||
===Human resources=== | |||
= | <div style="margin-left:0cm;margin-right:0cm;">The need for effective human resource utilisation is an important consideration. The nursing and cleaning staff will be working shifts. Staff working in the inpatient unit will depend on the number of beds or the size of the inpatient unit. This is especially true for the nursing staff, as their numbers are calculated per patient (or bed). The staff establishment (organogram) must be included when planning staffrooms, administration spaces, and ablutions </div> | ||
===Nursing models of care=== | |||
= | <div style="margin-left:0cm;margin-right:0cm;">The models of care may vary from department to department and have an impact on design. Clinically complex patients who require higher staff levels may benefit from smaller bed units to assist with the management of noise levels, supplies and equipment handling, as well as the facilitation of communication and emergency support. | ||
Nursing care is the main activity that allows the effective and efficient functioning of the inpatient unit. The inpatient unit design should therefore ensure maximum patient observation and contact, with short travel distances for the staff. | |||
Inpatient units should have no less than two single-bed units or more than four single-bed units per 32-bed inpatient unit. | |||
</div> | |||
===Unit management and administration=== | |||
<div style="margin-left:0cm;margin-right:0cm;">The unit manager’s office and clinical administration space should be positioned near the entrance to the inpatient unit for the purposes of management, client liaison and supervision. | |||
If there is a ward clerk, he or she needs to be placed at the entrance to the ward and preferably at a small reception counter or at the nurses’ station. If the ward clerk is placed at the nurses’ station, additional space must be provided to accommodate the activities of the ward clerk. | |||
The province’s policy with regard to staff facilities should indicate whether an inpatient unit staffroom or a shared restroom between inpatient units would be preferred. Staff toilets should be provided in each inpatient unit. | |||
</div> | |||
===Teaching and training=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">Hospitals are associated with the teaching of health professionals, especially in regional and tertiary facilities. The operational narrative for the project should consider the specific teaching requirements. Where teaching space is required in an inpatient unit in regional and district hospitals, the staffroom should be made larger to accommodate the lecturer and the students. Time management can ensure that the staffroom is utilised fully by scheduling the meetings or lectures to occur at times other than staff handover, tea or meal times. In tertiary hospitals where there will be larger groups for teaching, seminar rooms should be provided adjacent to the inpatient units. These can be shared on each floor or between two inpatient units. </div> | ||
===Access and circulation=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">The workplace design should minimise public access. Ideally, visitors should have access through one main entrance. Security should be placed at this entrance if necessary. However, support services such as emergency response teams should have maximum access to all areas of the workplace to facilitate their intervention in emergencies. | ||
Service staff may access the ward through a second entrance, but it should be monitored for both safety and security. Waste should exit separately. | |||
</div> | |||
=== | ===Infection control=== | ||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;"><u>''(Refer to the IUSS Infection Prevention and Control document.)''</u>The primary objective of hospital design is to place the patient at no risk of infection while he or she is hospitalised or in the hospital environment. Particular attention should be paid to patients with infectious diseases (TB in particular), immunocompromised patients, and paediatric patients. | ||
Infection control considerations must include all healthcare workers. All areas of the facility shall be designed, constructed, furnished and equipped in keeping with the principles of infection control | |||
The following aspects contribute to effective infection prevention and control and are relevant within the context of an inpatient unit: | |||
*Hand hygiene facilities should be provided in all patient care areas, clinical areas and nurses’ stations. | |||
*Hand hygiene facilities should be provided in areas where careful attention to hygiene is essential, such as kitchens, sluice rooms, utilities, medicine areas, bathrooms, toilets and change rooms. | |||
*Hand basins must be visible to staff on entering and leaving the room. In addition, antibacterial hand rub dispensers should be provided at the entrance to each inpatient unit. Hand-wash facilities should also be placed in the main passage of the inpatient unit and next to the nurses’ station. | |||
*Facilities should be provided to isolate infectious patients. | |||
*The following facilities should also be provided: | |||
**Linen handling | |||
**Separation of clean and dirty work flows | |||
**Storage | |||
**Waste management | |||
**Ventilation | |||
**Surface finishes | |||
*Careful aseptic technique and the observance of ‘standard precautions’ | |||
*The administrative infection control measures and protocols of the hospital should be followed and implemented in the design</div> | |||
===Airborne infection isolation and protective environments=== | |||
= | <div style="margin-left:0cm;margin-right:0cm;">In adult inpatient accommodation, special environments need to be created for patients who are immunocompromised and at high risk of contracting airborne infection and for infectious patients posing a risk of transmitting airborne infections. These two groups of patients require protective environment rooms and isolation rooms respectively. Where patients are both at high risk of contracting an infection and are themselves highly infectious, positive pressure protective isolation rooms may be required. For the isolation of highly pathogenic and infectious or contagious diseases, such as viral haemorrhagic fevers, ward-level isolation may not provide sufficient protection, and high-security isolation with access to laboratories that comply with the requirements for Advisory Committee on Dangerous Pathogens (ACDP) Hazard Group 4 pathogens would be required. | ||
Protecting staff and visitors from infectious diseases is an important aspect of airborne infection isolation (AII). It should not be assumed that a well-designed and functional ventilation system provides sufficient protection for these persons. Personal protective equipment such as N95 or FFP2 respirators should be provided to all staff and visitors entering AII rooms. Where these persons are expected to enter such environments regularly, these persons should have themselves fit tested for respirator use. | |||
Ceilings in AII and '''protective environment''' (PE) rooms shall be impervious monolithic structures to ensure excellent sealing and airtightness. Ceiling voids above these rooms, especially PE rooms, can be particularly hazardous spaces. | |||
All swing doors shall be equipped with door closers to ensure that they remain shut when not in use. Hold-open devices are not recommended for these doors. Sliding doors are also not recommended as these pose difficulties in maintaining an adequate seal. | |||
<div style="margin-left: | It is recommended that isolation rooms be provided with outside views where possible, without presenting a biosecurity risk. Privacy blinds should be installed, but these should not present a hygiene risk or hinder the nursing staff view of the patient.</div>[[File:Negative_pressure_isolation.png|alt=|none|thumb|444x444px|Figure 1: Negative pressure isolation]]<div style="margin-left:0cm;margin-right:0cm;"> | ||
'''Negative pressure isolation''' is only required for patients presenting with airborne infections, for example, measles, Severe Acute Respiratory Syndrome (SARS), and TB. These infections spread primarily through the respiratory route where the infectious particles have a diameter of less than 5 µm. The unit for measuring ventilation is air changes per hour (ACH). In accordance with the national building regulations, isolation rooms shall be single occupancy with ventilation rates in excess of 12 ACH (including en suite bathrooms and anterooms). Where airborne contamination control in these rooms is achieved through dilution, these rooms shall have near perfect mixing with air change efficiencies approaching 50%. This implies that the ventilation efficiency in the isolation room shall be 50% as efficient as plug flow. Contamination removal effectiveness around the patient can be improved by placing an extraction point near the head of the bed. Airflow patterns within the room shall be developed so that the air shall flow from the passage door and air inlet terminal, across the patient and towards the bathroom and extraction points. | |||
Convergent fluctuations of only 5 Pa in each of two adjacent rooms can potentially reduce the pressure differential between the rooms by 10 Pa. For this reason, pressure differentials of 15 Pa between rooms are recommended. Lower pressure differentials are easier to achieve, but offer less safety under normal operational fluctuations condition. | |||
The use of visual air pressure monitors between the passage and the isolation room is required. This enables a constant visual indication of the airflow direction between the isolation room and adjacent areas. These monitors should indicate the pressure magnitude, direction and out-of-specification failure limits. All major ventilation system components serving these areas should be clearly marked with the room identification, system identification and a biohazard sign. | |||
Supply and extraction systems should be interlocked so that a failure of the exhaust air system shuts the air supply off, preventing the isolation room from going into an overpressure status. It is acceptable to install a balanced-blade pressure stabiliser to ensure that the room does not experience extremes of pressure under supply fan failure, control system failure, or severe transient environmental conditions. However, the inclusion of these devices can increase the design capacity of the system under normal operation. | |||
Additional information regarding engineering services design and planning for airborne precaution rooms can be found in the [http://www.iussonline.co.za/norms-and-standards/cross-cutting-issues/ IUSS Building Engineering Services Guideline][http://www.iussonline.co.za/norms-and-standards/cross-cutting-issues/ .][http://www.iussonline.co.za/norms-and-standards/cross-cutting-issues/][[File:Protective_Environment-Positive_pressure.png|alt=|none|thumb|468x468px|Figure 2:Protective environment – positive pressure]] | |||
A PE room is required for patients who are immunocompromised, but do not initially present with an airborne infectious disease. These rooms require an anteroom to ensure a clean environment in the PE room. Where these are located within open wards, such as high-care units (HCUs) or intensive-care units(ICU), and are held at pressure positive to adjacent rooms, they should include negative pressure anteroom to prevent the potential spread of infection out of the PE room. For burns ward; however, negative pressure isolation with a sink anteroom, which is more negative in pressure, could be prescribed where sufficient separation from susceptible patients in adjacent ICUs cannot be ensured. Where airborne infection risk is suspected in these rooms, staff and visitors entering the PE room should wear respirators prior to entering the anteroom. Additional ventilation measures, such as using at least HEPA (H13) filtered supply air may be required when treating burns or allogeneic patients.[[File:Airborne_infection_protective_isolation.png|alt=|none|thumb|479x479px|Figure 3: Airborne infection protective isolation]]Where patients are immunocompromised and initially suspected of presenting with an infectious airborne disease, they should be located in an '''airborne infection protective isolation''' room. These rooms shall be designed to maintain a negative pressure relative to the anteroom and adjacent rooms, with the exception of the en suite bathroom. These rooms demand very low air permeability with high-quality sealing. The Centres for Disease Control (CDC) Guidelines for Environmental Infection Control in Health Care Facilities (2003) recommend an effective leakage area of less than 0.045 m² for the entire room. Placing this in context, the equivalent gap for a single half-leaf door that has been hung relatively well is calculated in the order of 0.04 m². | |||
Respiratory protection needs not be worn in the anteroom in this scenario, as the anteroom is held at a relative pressure positive to the patient room. | |||
While it may be tempting to develop positive pressure protective isolation rooms that can be adjusted to operate as negative pressure protective isolation rooms for airborne infection control, this practice is strongly discouraged, since it presents the inevitable scenario where the room is operated in an inappropriate mode for the wrong case, which places many people at risk of infection. The operation of neutral pressure rooms as a compromise is also not recommended as the negligible room permeability required for these rooms is not easily achieved or maintained. | |||
</div> | |||
===Ergonomics in design=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">All facilities shall be designed and built in such a way that patients, staff, visitors and maintenance personnel are not exposed to avoidable risks. | ||
Designers should consider the optimum comfort of all situations for staff, patients and visitors. | |||
Refer to: | |||
* | *Alder, D. and Tutt, P. eds., 1992. ''New metric handbook : Planning and design data''. Oxford: Reed Educational and Professional Publishing Ltd. | ||
*Neufert, E. and Neufert, P., 2012. ''Neufert architects’ data.'' 4th ed. New York: John Wiley & Sons. | |||
</div> | |||
===Universal access=== | |||
<div style="margin-left:0cm;margin-right:0cm;"><u>''(Refer to the IUSS Inclusive Environments document.)''</u>Consideration must be given to the wide range of clients, as well as those who are disabled, including the following | |||
=== | *Mobility impaired | ||
*Visually impaired | |||
*Hearing impaired | |||
</div> | |||
===Telecommunication and IT systems support=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">The design of the inpatient unit should include the following: | ||
*Telecommunication system | |||
*Nurse call to all patient areas with central control system | |||
*Paging and personal telephones replacing some aspects of call systems | |||
*Bar coding for supplies, X-rays and records | |||
*Computer network connections in all management and patient administration and information systems: | |||
**Hospital information system (HIS) and electronic patient records | |||
**Patient administration system (PAS) | |||
**Radiology information system (RIS) (digital X-rays) | |||
**Picture archiving communication system (PACS) | |||
**Laboratory with a link to the National Health Laboratory Service (NHLS) | |||
**Pharmacy system | |||
</div> | |||
===Wayfinding and signage=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">Wayfinding and signage must be considered from the inception of the design process. As hospital buildings become more complex, the more difficult it is for patients, visitors, suppliers and staff to navigate their way through the building to and from their intended destination. The layout of signage throughout the hospital must be logical and it must be simple and easy to follow. | ||
It is important to plot the various routes patients, visitors, suppliers and staff may have to travel to get to the inpatient facility from the car park, drop-off points and other departments in the hospital. Once these routes are established, principles can be applied to the design to assist successful wayfinding. | |||
Ways to enhance wayfinding include the following: | |||
*Printed information (pamphlets | |||
*Architectural features and design elements that provide clues as to what the function of the building is and can include landscaping, sculptural features and architectural interior design | |||
*Floor covering, lighting, wall, door and window graphics | |||
*Permanent signage | |||
*Digital devices (e.g. kiosks or information screens) | |||
*Human interaction (e.g. human interaction at help desks) | |||
</div> | |||
The following core principles should be adhered to: | |||
*Design that includes everyone, especially those who are more vulnerable, such as the following: | |||
**The first-time visitor | |||
**The physically challenged | |||
**Those with some form of impairment | |||
**Children | |||
*Utilisation of standardised information systems | |||
*Utilising ‘key hub’ destinations along a complex journey (a person is directed to a primary hub destination then directed on to a secondary hub destination from that point) | |||
*Toponomy, giving names and numbers to places and functions | |||
*A clear, simple wayfinding system | |||
Signage is a critical ‘wayshowing’ component of wayfinding. Information displayed in the signage needs to comply with the following: | |||
*Be organised and presented in a logical, sequential layout | |||
*Contain a maximum of five destinations in the case of directional signs | |||
*Be listed at the top of the hierarchy or highlighted as primary information in the case of key hospital hub destinations | |||
*Be presented lower in the information hierarchy in the case of secondary destinations | |||
*Be grouped and ordered with logic relevant to the destinations listed in the case of destinations on signs, either in alphabetical order according to the direction to the destination in clockwise order or according to the order of the distance to the destination (closer destinations first) | |||
*Connect labels (destinations) to arrows | |||
*Arrow designs should be based on the ISO arrow (ISO 7001) | |||
*Colour coding of floors or as a method of differentiating space may be used, however, people do not always perceive that the colour use has significance. This is worse for people who are colour blind. It is, however, a useful component of the wayfinding system | |||
*Signage should use the following: | |||
**Accessible terminology – common references that everybody understands | |||
**Avoid the use of acronyms and use universally understood symbols | |||
**Provide clear contrast between the information content and its surrounding environment | |||
**A finish that does not detract or obscure the signs intention | |||
[[File:Directional_signage.png|alt=|none|thumb|Figure 4: Directional signage]]Mapping is an important part of wayfinding system. Maps should be located at strategic points throughout the site and allow visitors to orlantate themselves. The maps should be consistent with the signage and the typology needs to be clear.[[File:Photo_1.png|alt=|none|thumb|Photograph 1: Mitchells Plain Hospital, Cape Town: Maps strategically placed per floor]] | |||
<div style="margin-left: | ===In the inpatient facility=== | ||
<div style="margin-left:0cm;margin-right:0cm;">Each department and inpatient unit should be marked individually and clearly. Wayfinding should help patients, visitors and the community to understand the hospital and inpatient unit spaces. The requirement for strict access control in the hospital makes it very important for patients and visitors to be directed along routes accessible to them. | |||
Appropriate signage for all the internal rooms and the external buildings should make use of universal signage and should, take the provincial policy on signage and wayfinding into account as far as possible. Comprehensive signposting shall be provided for all hospitals. Signposting will clearly identify staff, patient and visitor areas. It will also draw attention to restricted areas. | |||
===General=== | |||
Bed numbers shall be shown outside the patient bedroom. These shall be one number per bed. | |||
In bedrooms with more than one bed, all bed numbers or the range of numbers shall be shown on the sign outside each room. In bedrooms with more than one bed, each bed number shall also be displayed at the bed head. | |||
The lettering style Helvetica Medium upper and lower case is generally recommended. Upper case only is recommended for the building’s main entrance sign. | |||
===Room signs=== | |||
Non-illuminated, internal and external room function identification signs that are located on doors require the following considerations: | |||
*The format should allow easy replacement of the sign or sign inset when the room function changes. | |||
*Numbering on the inpatient units should be uniform, starting at the entrance with the first room on the left-hand side. | |||
*Each bed in each unit must be numbered. | |||
===Patient information board=== | |||
A whiteboard, which lists the patients that are currently occupying the beds, should be mounted on the wall behind the nurses’ station. The whiteboard should be a ‘wipe’ board with a suitable surface for nurses to add and erase the information. The information should be indicated as follows with lines drawn to separate each row and column: | |||
Table 2: Example of the patient information board | |||
{| class="wikitable" | |||
!Bed no | |||
!Patient name | |||
!Doctor | |||
!Date in | |||
!Date out | |||
!Notes | |||
|- | |||
|<br /> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
<br /> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
<br /> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
The patient information board should be supplied and fitted by the contractor | |||
</div> | |||
===Ventilation and air management=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">Methods of ventilation are discussed in the [http://www.iussonline.co.za/norms-and-standards/cross-cutting-issues/ IUSS Building Engineering Services] guidance document. | ||
Adequate ventilation throughout the health facility is important as poor ventilation affects patients and staff, and puts them at risk of being infected with nosocomial diseases. It is therefore necessary to ensure that spaces are ventilated so that the quality of the air breathed is improved by diluting the air and removing pollutants that are harmful. The main aim is to provide ventilation that maintains thermal comfort and indoor air quality that reduces the risk of cross-infection. This can be achieved through natural, mechanical or hybrid methods of ventilation. | |||
The chosen method will have a significant effect on the design of the inpatient unit. | |||
</div> | |||
===Day- and night-time illumination=== | |||
*All rooms should be provided with the required electrical illumination | |||
*All patient beds should be provided with a reading light | |||
*Night lights should be provided in passages so that they do not disturb patients | |||
*Emergency lighting is critical in inpatient units such as paediatrics, theatres and ICU | |||
=== | ===Fire detection and alarms=== | ||
<u>''Refer to Fire Regulations and SANS 10400 Regulations''</u> | |||
*All inpatient units should have escape doors in case of fire | |||
*The inpatient units should be provided with smoke detection systems | |||
*Sprinkler systems are not recommended | |||
*Fire extinguishers should be provided and slightly recessed so as not to cause obstruction | |||
*All inpatient units should have an evacuation plan that is aligned with escape routes | |||
===Security=== | |||
<div style="margin-left:0cm;margin-right:0cm;"><u>''(Refer to the IUSS Security Guideline.)''</u> | |||
*Access to and from the inpatient unit | |||
*Spaces that must be secured (medication store) | |||
*Security in individual spaces of the unit | |||
</div> | |||
===Supply and disposal=== | |||
<div style="margin-left:0cm;margin-right:0cm;">Stores, provisions, food, linen and surgical disposables, equipment and waste management will be required as part of the inpatient unit functions. The following list provides an indication of the requirements. | |||
*Laboratory – collection of specimens | |||
*Mobile X-rays | |||
*Central stores – disposables, stationery, cleaning materials and new equipment | |||
*Pharmacy – medicines and drugs, delivery of prescriptions and return of empty recyclable containers | |||
*Central Sterile Services Department (CSSD) – sterile packs, return of opened unused packs and used recyclable equipment | |||
*Linen store – clean linen, return of dirty linen | |||
*Kitchen – patient meals (the size of the kitchen depends on the meal production and delivery processes involved) | |||
*Central Cleaning Depot (CCD) – cleaning equipment | |||
*Refuse – general waste (domestic), pathological waste for incineration, recyclable waste, sharps. | |||
Material handling of inpatient unit supplies includes the following: | |||
* | *To and from the laboratory – the collection of specimens | ||
* | *Mobile X-ray equipment – space around patient beds and parking space for the equipment (a bay off the passage) | ||
* | *From the central stores – delivery of disposables, stationery, cleaning materials and new equipment | ||
* | *To and from the pharmacy – delivery of medicines and drugs, delivery of prescriptions and return of empty recyclable containers, sending of prescriptions to the pharmacy | ||
** | *To and from the CSSD – delivery of sterile packs, return of opened unused packs and used recyclable equipment | ||
* | *To and from the linen store – delivery of clean linen, sluicing of linen and return of dirty linen to the laundry | ||
*To and from the kitchen – delivery of patient meals in a trolley, trolley parking in the inpatient unit and return of the utensils and cutlery in the trolley back to the main kitchen | |||
*CCD – delivery and storage of cleaning equipment | |||
*Refuse – removal of general waste (domestic), pathological waste for incineration, recyclable waste, sharps | |||
*General hospital policies relevant to the various departments, such as linen supply and waste management, should be applied | |||
</div> | |||
===Medication management=== | |||
*Pharmacy staff should be consulted with regard to medication and intravenous fluids storage requirements for each inpatient unit. | |||
*The inpatient unit depends on the pharmacy for pharmaceutical support. This includes inpatient unit medication, scheduled drugs, patient prescriptions and discharge medication. • Security and access control to medication rooms should comply with local legislative Government Gazette No 25872, Pharmacy Act, 2 January 2004 – jurisdiction requirements and the hospital policy. | |||
*The location and design of the medication room should minimise travel distances, noise and disruption to staff undertaking medication-related activities in order to reduce error. All medication should be stored in a temperature-controlled, locked environment. The medicine trolley, inpatient unit stock and patient prescriptions should be stored in a medicine room that should be close to and directly visible from the nurses’ station. | |||
*The management of intravenous fluids should be clarified for the specific facility as to the quantity to be stored within the clean utility room (inpatient unit bulk stock is kept in the surgical and medical storeroom with small quantities kept in the clean utility). | |||
*If additives are introduced to intravenous fluids in the inpatient unit, it should occur in the clean utility room. | |||
=== | [[File:Figure_5.png|alt=|none|thumb|321x321px|Figure 5: Interactive management and control of pharmaceutical substances]]The equipment store is intended for storage of equipment that has to be floor parked or stored on shelves and for equipment that may require the recharging of batteries. The requirements will vary and need to be defined so that appropriate storage space is allocated according to the requirements of the inpatient unit and the needs of the patients and staff.<div style="margin-left:0cm;margin-right:0cm;"> | ||
===Options for dispensing within the inpatient unit=== | |||
Lockable medication trolleys should be stored in the medicine storeroom behind or directly opposite the nurses' station so that the store is in full view of nurses at all times.[[File:Figure_6.png|alt=|none|thumb|Figure 6: Relationship of medicine store]] | |||
===Equipment cleaning=== | |||
'''Medical equipment:''' The operational narrative should guide whether reusable items will be processed in the inpatient unit or whether they will be sent to the CSSD | |||
'''Beds:''' These are cleaned in the inpatient unit | |||
===Storage - equipment=== | |||
The equipment store is intended for storage of equipment that has to be floor parked or stored on shelves and for equipment that may require the recharging batteries. The requirements will vary and need to be defined so that appropriate storage space is allocated according to the requirements of the inpatient unit and the needs of the patients and staff. | |||
The equipment store should be located close to the sluice room, as equipment requires cleaning and disinfecting before storage. | |||
Equipment should be organised so that it is easily accessible by staff when required. Items used regularly, such as an emergency trolley with oxygen cylinders, scales and mobile blood pressure (BP) units may be stored locally in equipment bays. Rarely used items may be stored in a central equipment store. A long rectangular room allows the optimum use of space. | |||
Power outlets (4 to 16) should be provided for the recharging of equipment, depending on the equipment list compiled per level of care. | |||
Equipment, particularly larger equipment that has to be floor parked, needs to be defined so that appropriate storage space may be allocated according to the needs of the patients and staff. | |||
</div> | |||
===Storage – sterile supplies and consumables (sterile and surgical stores)=== | |||
<div style="margin-left:0cm;margin-right:0cm;">Sterile supplies should be handled and stored in a manner that maintains the integrity of packs and prevents contamination from any source, e.g. dust, vermin, sunlight, water and condensation. Sterile or surgical stores should be temperature- and light-controlled and easily cleaned. Sterile supplies (packs) are stored in the clean utility room. Surgical and medical consumables are stored in a stockroom. | |||
Supplies should be stored off the floor, with the lowest shelf at least 300 mm above floor level to avoid mechanical damage during cleaning, and the top shelf no higher than 1 850 mm.[[File:Figure_7.png|alt=|none|thumb|339x339px|Figure 7: Interactive relationship for the management and control of supplies and consumables]] | |||
===Storage of patients' belongings=== | |||
The method of storing patients' belongings depends on hospital policy. However, the following considerations must be taken into account: | |||
*Method of storing patients' belongings separately | |||
*System where contaminated clothing can be washed and decontaminated prior to storing in a patient's kitroom | |||
*Labelling method | |||
*Security | |||
*Type of storage, i.e. cupboards per bed unit, store per ward or central store for the whole hospital managed by a dedicated staff member who registers all items handed in | |||
*Size of the facility: many patients coming from rural areas will carry numerous items (e.g.blankets) with them that need to be stored until they are discharged | |||
</div> | |||
===Waste management=== | |||
<div style="margin-left:0cm;margin-right:0cm;">Management of clinical and related waste must follow infection control policies and regulations with regard to the disposal processes, as well as hospital policy. Household and paper waste should be managed in accordance with the recycling policies of the facility. The inpatient unit should be provided with a dirty utility room for storage of paper, household waste and dirty linen to reduce contamination and to separate clinical and household functions. | |||
Operational policies for waste management and waste minimisation should be supported, particularly with regard to the following: | |||
*Provision and location of dirty utility rooms so that staff do not have to traverse public and administration areas while transporting contaminated waste items | |||
*Provision and location of recycling bins | |||
*Location of sharps container | |||
==Inpatient unit activities== | |||
</div>Inpatient admissions to an inpatient unit need to provide for the following patient activities: | |||
*Clinical diagnostic activities (medical, diagnostic imaging, laboratory, inpatient unit rounds, doctors' visits, going for operations, investigations or rehabilitation) | |||
*Activities of daily living (dressing and undressing, eating, drinking, personal toilet and ablution activities) | |||
*Social activities such as receiving visitors | |||
*Patients might be disabled or might be semi-mobile due to weakness, age, or the disease profile | |||
Table 3: Inpatient unit activities | |||
{| class="wikitable" | |||
|+ | |||
! | |||
!Category | |||
!Activity | |||
|- | |||
|A | |||
|Patient | |||
|Patient Patient may be disabled and wheelchair bound | |||
Patient to dress and undress in vicinity of the bed | |||
Patient to take meals in bed or at the bedside | |||
Patient to read, watch TV or use a computer | |||
Patient to receive treatment and medical care from therapeutic and clinical staff, either lying down or sitting up in bed or in a chair | |||
Patient to wash hands | |||
|- | |||
|B | |||
|Nursing care | |||
|Teaching | |||
Stripping and making beds | |||
Transfer patient from wheelchair or patient trolley manually or by means of a patient-lifting device | |||
Patient observation and clinical (doctor’s) rounds | |||
Transporting patient to theatre on his or her hospital bed Treatment procedures such as intravenous fluids, traction, etc. | |||
Emergency procedures, e.g. patient resuscitation | |||
Coordination of patient care, observation, writing up of clinical notes, entering data into computers, making and receiving phone calls and washing hands | |||
|- | |||
|C | |||
|Medical intervention | |||
|Diagnostic procedures, such as mobile X-rays and ultrasounds, electrocardiograns (ECGs) | |||
Teaching | |||
Treatment procedures such as intravenous fluids, traction, etc. | |||
Emergency procedures, e.g. patient resuscitation | |||
Examination of patients and washing hands | |||
Writing reports and instructions, writing up of clinical notes, entering data into computers | |||
Washing hands | |||
|- | |||
|E | |||
|Rehabilitative intervention: | |||
physiotherapists, social workers, | |||
occupational and speech therapists, | |||
paharmacist and radiographers | |||
|Occupationally specific therapeutic interventions | |||
Patient consulting | |||
Diagnostic procedures, such as mobile X-rays and ultrasounds, ECGs, etc | |||
Washing hands | |||
|- | |||
|F | |||
|Clerical or administrative | |||
|Answering telephones, receiving patients and visitors to the patient unit | |||
Writing reports and collecting and entering data and statistics, ordering food and other consumables | |||
Washing hands | |||
|- | |||
|G | |||
|Ancillarystaff (aide, patient assistant) | |||
|Assisting patients in wheelchair | |||
Entertaining patients | |||
Washing hands | |||
|- | |||
|H | |||
|General staff | |||
|Serving food to patients | |||
General tidying work | |||
Daily cleaning - sweeping, dusting, washing up | |||
Routine cleaning - floors, windows, walls | |||
Washing hands | |||
|- | |||
|I | |||
|Maintenance staff | |||
|Maintenance- replace globes, fix fittings, reseal floors and repair work to maintain the inpatient unit | |||
Washing hands | |||
|- | |||
|J | |||
|Visitors | |||
|Visit patients and socialise in the inpatient unit or day room | |||
Washing hands | |||
|} | |||
==Client expectations== | |||
===Patient expectations=== | |||
*Patient privacy and dignity both in the design of the facility and in the treatment of the patient | |||
*Personal safety and security of the patient’s own possessions | |||
*The provision of patient comfort in the facility, e.g. a clean and uncluttered environment, an outside view, low noise levels in the facility, the availability of technical services (staff call system, reading light) | |||
*Adequate availability and visibility of nursing staff | |||
===Staff expectations=== | |||
*A work environment with reduced walking distances, but increased patient observation with minimum staff (optimal care) | |||
*Improved patient risk management, e.g. availability of technical bed-head services, availability of clinical hand basins in patient and staff areas, the availability of automatic bedpan washers, improved environmental control (with reduced infection risk) | |||
*A safe work environment, e.g. suitable height of shelves and service outlets, non-slip floors, view of unit entrance and exit, access control | |||
*Personal safety and security of possessions, e.g. staff lockers, staffroom. | |||
==Location and inter-departmental relationships== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">Inpatient accommodation (inpatient units) accounts for a large percentage of the surface area in a hospital and, as such, the orientation and placement of the inpatient units should be given priority in the design of a hospital master plan. Figure 8 and Figure 9 illustrate the models of care and significant relationships in a typical hospital. | ||
The design of smaller hospitals may allow the inpatient units to be arranged over the same level. However, inpatient units of larger hospitals may be arranged into multistorey blocks separate from the diagnostic and treatment facilities. This makes it easier to place the inpatient unit block away from noisy areas, ensures patient privacy and safety, and avoids visitors, staff and service traffic through the inpatient units. | |||
Stacking of the inpatient units in multilevel blocks also allows more consistent planning of inpatient accommodation. | |||
The following inter-departmental relationships with the inpatient units are recommended: | |||
*Patient administration and primary circulation should be central to the entrance with the access route to the inpatient facilities off the primary circulation route. | |||
*The obstetric inpatient units should be close to the delivery suite and close to the operating theatre, preferably on the ground floor or with a direct lift access to theatres. | |||
*In district hospitals, operating theatres, HCUs, orthopaedic inpatient units and surgical inpatient units should have a close relationship and preferably be on the same floor. | |||
*Rehabilitation, physiotherapy and occupational therapy should be close to rehabilitation inpatient units and accessible to the outpatients department and the inpatient units. | |||
*Hotel services (cleaning, linen and food services), mortuary services and maintenance units should have a reasonable relationship to the inpatient units. The mortuary, kitchen and laundry should have better access than all other services, especially at night (particularly mortuary services). | |||
*Visitors to the inpatient units should not cross functional access with the services to and from the inpatient units. | |||
</div> | |||
===Staff overnight facilities=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">District hospitals only have overnight facilities in the maternity wards and EU sections. Regional hospitals have overnight facilities for ICUs, EUs, maternity wards, diagnostic radiology and paediatrics with facilities for medical and surgical inpatient units not necessarily in the inpatient unit. Tertiary hospitals may have a separate overnight facility for students and qualified staff in one location or separate locations.[[File:Figure_8.png|alt=|none|thumb|Figure 8: Hospital model of care]]Figure 8 illustrates the position of the inpatient units in relation to the hospital support services and the outpatient services. Inpatient units should be located separately, away from the mainstream, in the hospital complex to enable better privacy and separate the flow path of inpatients from outpatients after entering the main entrance to the hospital. This reduces the volume of traffic in the main passage to the inpatient units and avoids visitors, staff and service traffic through the inpatient units. | ||
*District hospital | |||
**Surgical inpatients are the inpatients most closely associated with the theatres. | |||
*Regional hospital | |||
**Orthopaedic inpatients are the inpatients most closely associated with the theatres. | |||
*Tertiary hospital | |||
**Subspecialist inpatients, such as neurosurgery and cardiology, are the inpatients most closely associated with the theatres. | |||
[[File:Figure_9.png|alt=|none|thumb|Figure 9: Departmental relationships]] | |||
==Flow patterns== | |||
</div> | |||
===Point of entry=== | |||
*Patients or visitors will access the facility through a secure entrance to a parking area or drop-off point from where there should be a clear direction (signage) to the required point of entry. | |||
*Alternatively, a patient will arrive via emergency services to the emergency unit or the maternity services entrance | |||
*Staff members access the facility through a secure staff entrance from a staff parking area or drop-off point.<br /> | |||
[[File:Figure_10.png|alt=|none|thumb|Figure 10: Three main flow paths]][[File:Figure_11.png|alt=|none|thumb|Figure 11: Inpatient flow patterns]]The diagram above illustrates three main inpatient streams that will accommodate acute admissions, maternity admissions and planned admissions. To ensure resource efficiency, the workflow and zoning should support these inpatient streams. | |||
The following flow paths relate to community, inpatients, clinical, visitors and support services to the inpatient units.[[File:Figure_12.png|alt=|none|thumb|Figure 12: Patient-flow diagram]]The workflow between departments has an impact on patient ans staff movement, as well as goods and service deliveries to the wards. Minimum walking distances between departments should be planned in the interest of resource management and traffic reduction through the facility[[File:Figure_13.png|alt=|none|thumb|Figure 13: Clinical flow diagram]]The diagram above indicates the clinical workflow dependencies between the clinical service and departments.[[File:Figure_14.png|alt=|none|thumb|Figure 14: Visitors flow diagram]]Figure 14 indicates the routes that visitors to the inpatient units would follow and Figure 15 shows the access routes for the service departments that would ensure access to the inpatient unit without affecting traffic through patient or clinical areas.[[File:FIGURE_15.png|alt=|none|thumb|Figure 15: Support services workflow diagram]] | |||
=== | ===Separation of clean and dirty flow paths in the inpatient unit=== | ||
Upon arrival arrival at an inpatient unit, a single entry point is preferred in order to control traffic in and out of the inpatient unit. However, infection control principles dictate that clean services should enter at a separate point to where waste and contaminated goods are taken out of the inpatient unit.[[File:Figure_16.jpg|alt=|none|thumb|373x373px|Figure 16: Entrance to and from the inpatient unit]]Patients, visitors and clinical staff, along with clean goods and services (including food deliveries), should enter and exit through the main entrance. Soiled and contaminated goods should exit from the inpatient unit through a separate entrance, preferably positioned at the most distant point from the main entrance. It must be noted that an exit separate to the main entrance is required in terms of fire regulations. This exit may be utilised to take out the contaminated goods. | |||
It is important that deliveries to and from the inpatient unit are managed in such a way that they do not clash with visitors arriving and leaving. Goods and services should be delivered at times other than visiting hours. | |||
==Functional zones== | |||
The inpatient unit functions as a stand-alone unit consisting of six separate functions | |||
Table 4: Inpatient unit functional zones | |||
{| class="wikitable" | |||
!Zone | |||
!Accommodation spaces | |||
|- | |||
|Administration spaces | |||
|Inpatient unit management, nurses' station and other office spaces as required | |||
|- | |||
|Public spaces | |||
|Entrances, circulation and waiting areas | |||
|- | |||
|Patient spaces | |||
|Patient accommodation and ablution facilities, patient day rooms, disabled showers, treatment room. | |||
|- | |||
|Service and support areas | |||
|Inpatient unit kitchen and storage, clean utility, sluice, stores, cleaners' room, linen, cleaning, medicine store, dirty utility and waste management | |||
|- | |||
|Staff spaces | |||
|Staffroom, locker area, ablutions, overnight accommodation* | |||
|- | |||
|Teaching spaces | |||
|Training or meeting room( in district hospital staffrooms could be used) | |||
|} | |||
These zones create the therapeutic environment required for successful healthcare delivery at inpatient unit level.[[File:Figure-17.png|none|thumb|493x493px|Figure 17: Adult inpatient accommodation: Internal zoning and relationships]] | |||
==Functional relationships within the inpatient unit== | |||
<div style=" | <div style="margin-left:0cm;margin-right:0cm;"> | ||
Inpatient unit layouts will vary depending on individual needs per project as outlined in the health and design briefs. However, general principles of design apply and the location of facilities within the inpatient unit should be a logical process optimising the workflow and travel distances for staff from service and storage areas to the patient’s bedside. | |||
The following general principles apply to functional relationships within the inpatient unit: | |||
*The visitors’ waiting room and visitors’ toilet should be outside the entrance to the inpatient unit and may be shared by two inpatient units on the same floor. | |||
*One central entrance to the inpatient unit with access control is preferred. | |||
*The kitchen should be close to the main entrance of the inpatient unit. | |||
*Deliveries and removal of kitchen trolleys should be managed so as not to clash with visiting hours and inpatient unit rounds. | |||
*Nurses’ stations should be positioned centrally with direct visual access to the inpatient unit entrance and in close proximity to the single-bed inpatient units, where the most critical patients would be accommodated. | |||
*The larger bed units for less critical patients could be positioned further away from direct nursing supervision. | |||
*The single-bed units, clean utility, medicine store and treatment room should be positioned near the nurses’ station. | |||
*Areas such as the inpatient unit kitchen and staff areas could be positioned off the main centre of the inpatient unit. | |||
*The clean linen store (or trolley) and sluice room should be close to the bed units to reduce walking distances for the nursing staff. | |||
*Dirty utility rooms should be positioned close to the separate exit door to facilitate collection of the contaminated items and waste, avoiding cross-contamination with clean goods by separating the workflow of clean and dirty paths in the inpatient units. | |||
*Design should minimise the distance between patient bed units, staff workstations and support rooms to facilitate the efficient delivery of patient care and optimal staff utilisation. | |||
*Each bed unit will be serviced by staff and support facilities, therefore access to supplies and means of disposal is essential. One of the primary goals is to minimise the distance between patient units and workstations and support rooms. The inpatient unit should be planned to provide a public/clinical and a utility/service division. | |||
*The unit manager’s office should be positioned for maximum supervision of both clinical and household functions (close to the entrance). | |||
*The clinical administration area and doctor’s office should be near the nurses’ station with access to the clinical spaces. | |||
*The sluice, linen, and storerooms should be positioned central to the patient bed units to reduce walking distances for the nursing and cleaning staff. | |||
No one particular inpatient unit layout has been found to be universally superior. In all cases, the final decision must be a response to the physical constraints of the site, local service needs, and operational policies. | |||
</div> | |||
===Ablution facilities=== | |||
<div style=" | <div style="margin-left:0cm;margin-right:0cm;">For infection control purposes, inpatients, clinical staff and visitors should be provided with separate ablution facilities. Ablution facilities for visitors should be located external to the inpatient unit. | ||
Patient ablution facilities should be en suite directly accessible from the adjacent bed unit. Ablution facilities for clinical staff may be provided in association, but not combined with staffroom areas. Designated toilets for clinical staff should be provided. | |||
</div> | |||
===Key room relationships=== | |||
It is important that key room relationships are maintained such as illustrated in figure 18.[[File:Figure_18.png|alt=|none|thumb|361x361px|Figure 18: Room relationships that promote the principal of ‘clean to dirty’ flow]][[File:Figure_19.png|alt=|none|thumb|363x363px|Figure 19: Room relationships with the inpatient unit (Example 1)]][[File:Figure_20.png|alt=|none|thumb|368x368px|Figure 20: Room relationships with the inpatient unit (Example 2)]] | |||
==List of rooms== | |||
The majority of rooms in ward are standard rooms that may be found in other departments in the health facility. These rooms have been detailed separately in the IUSS: GNS generic room requirement sheets. These sheets must be referred to when planning the rooms. | |||
Table 5 lists the rooms found in the inpatient unit and indicates the rooms that are standard and those that are non-standard. The non-standard rooms that are described in more detail under 'room requirements'. The standard rooms are described in less detail as they are detailed in the IUSS: GNS generic room requirement sheets. | |||
Table 5: Loss of rooms: Standard and non-standard | |||
{| class="wikitable" | |||
|+ | |||
!Room | |||
!Standard | |||
!Non-standard | |||
|- | |||
| colspan="3" |'''Patient areas''' | |||
|- | |||
|Bed unit - Standard patient area: | |||
| | |||
| | |||
|- | |||
|Single-bed unit | |||
|x | |||
| | |||
|- | |||
|Two-bed unit | |||
|x | |||
| | |||
|- | |||
|Four-bed unit | |||
|x | |||
| | |||
|- | |||
|Patient day room(provided in a district hospital) may be shared between wards | |||
|x | |||
| | |||
|- | |||
|Patient ablutions: | |||
| | |||
| | |||
|- | |||
|En suite facility with shower, toilet and hand basin (all should be disability friendly) | |||
|x | |||
| | |||
|- | |||
|Assisted bath where required | |||
|x | |||
| | |||
|- | |||
|Assisted shower | |||
|x | |||
| | |||
|- | |||
| colspan="3" |'''Staff areas''' | |||
|- | |||
|Office - manager | |||
|x | |||
| | |||
|- | |||
|Office - Counselling or doctor (optional) | |||
|x | |||
| | |||
|- | |||
|Nurses' station | |||
|x | |||
| | |||
|- | |||
|Clinical admin area | |||
| | |||
|x | |||
|- | |||
|Office - administration | |||
|x | |||
| | |||
|- | |||
|Staffroom | |||
|x | |||
| | |||
|- | |||
|Staff lockers can be provided in a passage off the main passage leading to the restroom | |||
|x | |||
| | |||
|- | |||
|Toilet - staff (male and female) | |||
|x | |||
| | |||
|- | |||
| colspan="3" |'''Service support areas''' | |||
|- | |||
|Bay - mobile equipment | |||
|x | |||
| | |||
|- | |||
|Bay - Resuscitation trolley | |||
|x | |||
| | |||
|- | |||
|Clean utility ( setting out the sterile packs and treatments) | |||
|x | |||
| | |||
|- | |||
|Cleaners ' station | |||
|x | |||
| | |||
|- | |||
|Dirty utility (refuse and dirty linen) | |||
|x | |||
| | |||
|- | |||
|IT room - consult with information and communication technology (ICT) planners depending on the hospital | |||
| | |||
|x | |||
|- | |||
|Sluice room | |||
|x | |||
| | |||
|- | |||
|Store - Clean linen | |||
|x | |||
| | |||
|- | |||
|Store - Equipment | |||
|x | |||
| | |||
|- | |||
|Store - Kit (patients' clothes and belongings could be in a central area or per inpatient unit - refer to brief) | |||
|x | |||
| | |||
|- | |||
|Store - Medicine | |||
|x | |||
| | |||
|- | |||
|Store - Consumables (surgical and medical) | |||
|x | |||
| | |||
|- | |||
|Treatment room | |||
|x | |||
| | |||
|- | |||
|Inpatient kitchen | |||
|x | |||
| | |||
|- | |||
|Body-holding room | |||
|x | |||
| | |||
|- | |||
|'''Public areas''' | |||
| | |||
| | |||
|- | |||
|Inpatient unit corridor | |||
|x | |||
| | |||
|- | |||
|Entrance | |||
|x | |||
| | |||
|- | |||
|Visitors' waiting area | |||
|x | |||
| | |||
|} | |||
==Room requirements== | |||
===Bed unit – standard patient area=== | |||
<div style="margin-left:0cm;margin-right:0cm;">The bed units are to accommodate patients for the delivery of medical care and treatment. | |||
These guidelines allow space in all bed units for equipment and the activities around each bed and between beds. | |||
</div> | |||
===Location and relationship=== | |||
<div style="margin-left: | <div style="margin-left:0cm;margin-right:0cm;">Bed units should be positioned to provide appropriate supervision from the nurses’ stations and be visible between beds. | ||
En suite bathrooms shall be dedicated to each room and will be directly accessible from the bed unit.[[File:Figure_21.png|alt=|none|thumb|Figure 21: Left-right orientation of a patient bed]]'''Important:''' The reference to the left and right side of the bed should describe the patient's left and right when lying down in the bed facing the ceiling. The bedside locker is placed according to the patient's preference. | |||
===Staff capacity=== | |||
Space is required to adequately accommodate the activities taking place at the patient's bedside and the movement by staff around the bed, which can involve several staff at any one time and may also include the use of equipment at the patient's bedside. | |||
These activities can involve the following: | |||
*Doing clinical observations taking blood, blood pressure and the patient’s temperature | |||
*Assisting with activities of daily living: dressing, feeding and washing | |||
*Treatment procedures, such as intravenous fluids, traction, etc. | |||
*Examining the patient | |||
*Stripping and making beds | |||
*Transferring the patient from a wheelchair or patient trolley manually or by means of a patient-lifting device (patient may arrive in a wheelchair or on a patient trolley) | |||
*Patient observation and clinical (doctor’s) rounds | |||
*Diagnostic procedures, such as X-rays, ultrasounds, ECGs, etc. | |||
*Transporting the patient to the theatre on his or her hospital bed | |||
*Emergency procedures, e.g. patient resuscitation | |||
*Recording of notes at the bedside either manually or on the computer (clinical staff) | |||
*Cleaning and dusting around the bed (clinical staff) | |||
*Maintenance work (maintenance staff) | |||
</div> | |||
===Patient activity=== | |||
*May sit next to the bed | |||
*Receives treatment from therapeutic and clinical staff while lying down or sitting in bed | |||
*Receives visitors | |||
===General requirements=== | |||
The following is required in the bed unit space: | |||
*Space should be provided for a bed and bedside locker next to each bed, preferably on the right. | |||
*Temperature in bed units should be between 20 ˚C to 23 ˚C. | |||
*Positive air pressure should be maintained in bed units. | |||
*Bed curtain rails and curtains should be provided for privacy around each bed. | |||
*Each bed unit should have a disability-friendly en suite shower, toilet and hand basin with a call button for the nurse. | |||
*A clinical hand basin with elbow taps, goose neck and an outlet must be provided in the bed unit. The basin and backsplash should be a moulded unit. A wall-mounted mirror, soap dispenser and paper towel dispenser should be provided with each hand basin. | |||
*Waste bins should be next to but lower than the hand basin. There should be one for medical waste, one for sharps (refer to brief document) and one for general waste. | |||
*There should be adequate lighting provision (natural and artificial light) – daylight is important in the bed unit. | |||
*The patient should have visual privacy without compromising staff control and observation of the patient. | |||
*A standard equipment list per level of care (district, regional or tertiary) should be made available. The list will distinguish between loose equipment to be provided by the client and fixed (mounted) equipment to be provided and installed by the contractor. | |||
===Space requirements=== | |||
Ergonomic studies have established that most activities carried out at the bedside can be accommodated within the dimensions 3 450 mm (width) × 4 100 mm (depth). This represents the clear bed space and does not include space for fixed storage. | |||
One bed unit equals a minimum of two and maximum of four beds per 32-bed inpatient unit in a district or regional hospital. The clinical brief will outline the tertiary hospital requirements. | |||
It is preferable for beds on opposite sides of the room to be offset to provide greater privacy. | |||
Single-bed unit approximately 15 m² minimum<div style="margin-left:0cm;margin-right:0cm;">Two-bed unit approximately 27 m² minimum | |||
Four-bed unit approximately 44 m² (majority of rooms) minimum | |||
Six-bed unit approximately 65 m² minimum[[File:DRAWING_1.png|alt=|none|thumb|362x362px|Drawing 1: Single-bed unit (minimum space dimension requirement)]][[File:DRAWING_2.png|alt=|none|thumb|337x337px|Drawing 2: Two-bed unit (a) (minimum space dimension requirement)]][[File:DRAWING_3.png|alt=|none|thumb|363x363px|Drawing 3: Two-bed unit (b) (recommended space dimension requirement)]][[File:DRAWING_4.png|alt=|none|thumb|360x360px|Drawing 4: Four-bed unit (a) (minimum space dimension requirement)]][[File:DRAWING_5.png|alt=|none|thumb|457x457px|Drawing 5: Four-bed unit (b) (recommended space dimension requirement)]]</div> | |||
===Bed services=== | |||
Services should be provided in wall bed-head units behind and above the bed.[[File:Photograph_2.jpg|alt=|none|thumb|Photograph 2: Example of services in bed-head trunking]]Photograph 2 shows an in-wall bed-head unit with power outlets, oxygen and vacuum outlets(shared between two beds), equipment rail for the mounting of, among other things, suction units, oxygen flow meters, nurse call button and a reading light[[File:DRAWING_6.png|alt=|none|thumb|Drawing 6: Services to district hospital bed]] | |||
Table 6: Bed-head services per level of care | |||
{| class="wikitable" | |||
|+ | |||
! colspan="4" |BED HEAD SERVICE | |||
|- | |||
|'''Service''' | |||
|'''District hospital''' | |||
|'''Regional hospital''' | |||
|'''Tertiary hospital''' | |||
|- | |||
|Oxygen | |||
|One shared between two beds | |||
|One per head | |||
|One per head | |||
|- | |||
|Medical air* | |||
(low pressure) | |||
|One shared between two beds | |||
|One per head | |||
|One per head | |||
|- | |||
|Vacuum | |||
|One shared between two beds | |||
|One per head | |||
|One per head | |||
|- | |||
|Power outlets | |||
(15Amp) | |||
|Four per bed: | |||
One to patient's right side for patient use | |||
Three to patient's left side for medical equipment purposes | |||
|Six per bed: | |||
Two to patient's right side for patient's use | |||
Four to patient's left side for medical equipment purposes | |||
|Six per bed: | |||
Four to patient's left side for medical equipment purposes | |||
|- | |||
|Equipment rail | |||
|One per head | |||
|One per head | |||
|One per head | |||
|- | |||
|Nurse call | |||
|One per head | |||
|One per head | |||
|One per head | |||
|- | |||
|Reading light | |||
|One per head | |||
|One per head | |||
|One per head | |||
|} | |||
<u>''(Refer to IUSS: GNS Building Engineering Services)''</u> | |||
===En suite sanitary facilities=== | |||
====Description and function==== | |||
An en suite bathroom provides facilities for patients to wash, shave, groom, shower and use the toilet, either independently or with assistance. The layout and area must accommodate an assisting nurse, patient lifter or wheelchair. The minimum area for this room is 6 m². | |||
====Location and relationships==== | |||
The en suite bathroom must be adjacent to the bed unit or directly accessible from each unit with the following services, preferably on an external wall: | |||
*Clinical hand basin with a mirror above it, soap dispenser and paper towel dispenser | |||
*Toilet | |||
*Nurse call button connected to the nurses’ station | |||
*An adjustable overhead hand shower head with flexible hose | |||
====General requirements==== | |||
Doors must open outwards from the en suite bathroom and must be fitted with an emergency release function. | |||
The shower must have a shower curtain | |||
The seat must fold up in the shower area and there should be a bench outside the shower (but within the en suite bathroom) for personal belongings. Three durable clothes hooks are to be mounted on the wall above this bench. | |||
Fittings must be mounted in such a way that the water temperature can be adjusted without the patient or nurse getting wet. | |||
The exit door must be fitted with escape hardware to allow staff access in the case of an emergency. | |||
Nurse call and emergency call buttons and indicators should be provided that are tamperproof. | |||
Epoxy grout is to be applied in all tiled areas. | |||
== | Fittings, including grab rails, are to be installed to the toilet and shower area, including towel rails.[[File:Drawing_7.png|alt=|none|thumb|369x369px|Drawing 7: Example of En suite bathroom (combined toilet and shower area) that accommodates wheelchairs]][[File:Drawing_8.png|alt=|none|thumb|371x371px|Drawing 8: Example of En suite bathroom (separate toilet and shower) that does not accommodate wheelchairs]] | ||
===Assisted shower=== | |||
====Description and function==== | |||
An assisted shower room with an enclosed shower cubicle, fitted with a door, to the height of a wheelchair or commode and a central floor drain is required. The shower head should be a hand-held device and the temperature of the water should be controlled. The size of the room should provide a minimum of 6.5 m² to provide space for the staff who will assist the patient. | |||
====Location and relationships==== | |||
The shower should be located immediately adjacent to or should be directly accessible from the passage of the inpatient unit. It should preferably be central to the bed units. | |||
====Services==== | |||
The following should be provided: | |||
* | *A hand basin with tiles above it, a mirror, soap dispenser and paper towel dispenser | ||
*A nurse call button connected to nurses' station | |||
*A hand-held shower head that can be removed from above with a flexible cord | |||
* | |||
* | |||
====Activities==== | |||
There should be sufficient space for two people in the shower area to assist the patient to wash and shower. | |||
=== | ====General requirements==== | ||
The following should be provided: | |||
*A waist-height shower enclosure with a hand-held shower head | |||
*An enclosed seat that can fold up | |||
*Taps of which to the water temperature can be adjusted without the staff assisting the patient getting wet | |||
*A door that is fitted with the escape hardware to allow staff access in the case of an emergency | |||
*Nurse call and emergency call buttons and indicators | |||
*Fittings, including grab rails and towel rails, that can accommodate non-ambukant patients | |||
*A hoist for lifting a patient | |||
[[File:Drawing_9.png|alt=|none|thumb|Drawing 9: Example of Assisted shower]][[File:Photograph_3.jpg|alt=|none|thumb|Photograph 3: Assisted Bath (Optional)]] | |||
===Counselling room=== | |||
====Description and function==== | |||
The counselling room provides a private area for staff to consult with patients and their family | |||
====Services==== | |||
The following should be provided: | |||
*A double-plug outlet | |||
====General requirements==== | |||
The following should be provided: | |||
*The room must create a tranquil, calm atmosphere. The use of color must be subtle - preferebly using pastel colours | |||
*A window with an outside view from this room is advisable | |||
*This room may be shared by two inpatient units | |||
====Furniture==== | |||
The following should be provided: | |||
A table and four chairs | |||
Lounger and comfortable lounge chairs with a side table | |||
===Day room=== | |||
====Description and function==== | |||
The day room provides space for the patient to socialise with other patients and visitors. The room should be a minimum of 12m². This is more applicable in rural district facilities. | |||
====Location and relationships==== | |||
The day room should comply with the following: | |||
*Have an external wall to take advantage of natural light and outlook | |||
*Be located away from bed units, but within close proximity to the nurses’ station to enable staff supervision and observation | |||
*Have direct access off the main inpatient unit passage | |||
====Activities==== | |||
The following should be provided: | |||
*Patients should be able to sit down and may play games, as well as socialise | |||
*Patients should be able to receive visitors | |||
====Services==== | |||
The following should be provided: | |||
*Two double-plug outlets | |||
====General requirements==== | |||
The following should be provided: | |||
*Low windowsill heights should promote views from a seated position. | |||
*Day rooms to be located inside the inpatient unit without outside access, or it may have outside access (to the garden or a balcony). This depends on the inpatient unit type and the need for security. | |||
== | ====Equipment==== | ||
<u>''(Refer to the equipment list.)''</u> | |||
In addition, the following should be provided: | |||
*Table and stackable chairs (to allow space for wheelchair users) | |||
*Water cooler | |||
*Waste paper bin | |||
[[File:DRAWING_10.png|alt=|none|thumb|Drawing 10: Example of Day room for patients]] | |||
===Treatment room=== | |||
====Description and function==== | |||
The treatment room provides a controlled environment, privacy and facilities for carrying out consultations, examinations and the treatment of patients. It should have a minimum size of 15 m². | |||
====Location and relationships==== | |||
The treatment room should be located with other patient care areas, near the clean utility with direct access to the inpatient unit passage. | |||
====Activities==== | |||
The following should be provided: | |||
*Four clinical staff members attending the patient at any given time | |||
*Access to patients from both sides of the couch | |||
*As the patient may be ambulant, in a wheelchair, on a trolley or in a bed, patient transfer may be required to the examination couch | |||
*Private examination and discussion with the patient | |||
*Specimen collection (e.g. bone marrow) | |||
*Wound treatment (applying or renewing dressings) | |||
*Other examinations and treatment activities specific to the medical discipline | |||
*Treatment by a physiotherapist or occupational therapist | |||
*Completing special examination requests and writing reports | |||
====Services==== | |||
The following should be provided: | |||
*A hand basin with elbow taps and a gooseneck outlet with tiles above it, a mirror, soap dispenser and paper towel dispenser | |||
*Four electrical points | |||
*A vacuum | |||
*Data and telephone terminals | |||
*A stainless steel sink | |||
*A good-quality examination light, preferably mounted on the ceiling | |||
*Bed-head service with two power outlets on the right of the patient examination couch and three power outlets on the left, oxygen and vacuum outlets, and an equipment rail for mounting items such as a suction unit, oxygen flow meter and nurse call button | |||
*A wall-mounted X-ray viewing panel where applicable | |||
====General requirements==== | |||
The following should be provided: | |||
*Lockable doors | |||
*A door that is wide enough for a bed to pass through | |||
*Curtains for patient privacy | |||
*A stainless steel worktop with a cupboard underneath it for stock (± 1.0 m) | |||
*Positive pressure | |||
*Temperature in the treatment room maintained at between 20 °C and 23 °C | |||
====Equipment==== | |||
The following should be provided: | |||
*An examination couch | |||
*A double-step foot stool | |||
*A mobile drip stand | |||
*A wall-mounted diagnostic set | |||
*A mobile vital signs monitor (nibp+hr+sao2); | |||
*An emergency oxygen cylinder on a mobile stand | |||
*An ECG machine on a mobile trolley | |||
*A fitted desk unit with a chair | |||
*A pedal bin or kickabout with a bucket | |||
[[File:DRAWING_11.png|alt=|none|thumb|Drawing 11: Treatment room example]] | |||
==Inpatient support requirements== | |||
The following inpatient unit support spaces are listed in alphabetical order | |||
=== | ===Body room=== | ||
====Description and function==== | |||
This room is specifically for holding a deceased patient until the body is collected by the mortuary | |||
*Size 3.5 m x 3.4 m | |||
====Location and relationships==== | |||
This should be located far away from the patients and public areas, and placed close to the service exit or service lift | |||
== | ====Activities==== | ||
Provision should be made for the following: | |||
<div style="margin-left: | *Holding of the deceased patient until collection by the mortuary | ||
*Preparation of the patient by nursing staff in anticipation of the family coming to view the patient | |||
*Viewing of the patient by the family | |||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
====Services==== | |||
The following should be provided: | |||
=== | *Clinical hand basin with elbow taps with gooseneck outlet and tiles above it, with soap dispenser and paper towel dispenser | ||
*Cupboards for storing equipment | |||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
====Considerations==== | |||
The following need to be taken into consideration | |||
<div style="margin-left: | *A quiet area with subdued lighting | ||
*Décor to create a calm atmosphere | |||
*Pastel, gentle colours to be used on walls and in curtains and blinds | |||
*The room may be shared by two wards | |||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
====Equipment==== | |||
The following should be provided: | |||
The patient is usually wheeled in his or her hospital bed, where he or she remains until he or she is collected by the mortuary, when the body is placed on a trolley before leaving | |||
=== | ===Clean utility=== | ||
====Description and function==== | |||
The clean utility is for the storage and preparation of clean and sterile materials and equipment for patient treatment, as well as the secure storage and preparation of medications, including intravenous fluids. A minimum space of 9 m² is required. | |||
====Location and relationships==== | |||
The clean utility should have direct access from the passage of the inpatient unit, with close proximity to the nurses’ station and the treatment room. | |||
====Activities==== | |||
The following should be provided: | |||
*One to two persons at any given time | |||
*Storage of sterile packs from the CSSD | |||
*Storage of liquids from the pharmacy | |||
*Hand washing by staff prior to trolley preparation for bedside treatment or procedures | |||
*Preparation of trolleys for treatment or procedures in the procedure room | |||
*Warming of solutions required during treatments or procedures | |||
=== | ====Services==== | ||
The following should be provided: | |||
* | *A stainless steel clinical, drop-in hand basin with elbow taps and gooseneck outlet | ||
* | *One double 15 Amp plug above counter height | ||
* | *Standard power outlet for liquid warmer: stand-alone or standing on the worktop | ||
====General requirements==== | |||
The following should be provided: | |||
*Lockable doors to the facility | |||
*Lockable cupboard with shelving for sterile packs and storage of vacolitre | |||
*Stainless steel worktop: space for one 600 x 450 mm instrument trolley and two 450 x 450 mm instrument trolleys underneath the worktop | |||
====Equipment==== | |||
The following should be provided: | |||
* | *Pedal bin | ||
*Liquid warmer: stand-alone or standing on the worktop | |||
* | |||
[[File:DRAWING_12.png|alt=|none|thumb|Drawing 12: A clean utility room example]] | |||
=== | ===Cleaner's room=== | ||
====Description and function==== | |||
The cleaning service may be in-house or outsourced, but space should be provided for a cleaner's room. | |||
The cleaning station provides a base for the cleaning staff to store and decant cleaning equipment, materials and cleaning agents, and a cleaner's trolley. A space requirement of 8 m² should be provided. A ratio of 0.8 m² per patient may be used to calculate the area. | |||
The room should be separate from the dirty utility room and the waste disposal room. | |||
====Location and relationships==== | |||
The cleaning station should be close to the exit of the inpatient unit with direct access to the inpatient unit passage | |||
====Activities==== | |||
Provision should be made for the following: | |||
*Usually one housekeeper or cleaner will utilise the area | |||
*Hand-washing by staff before leaving the room | |||
*Report writing | |||
*Water collecting and emptying cleaning buckets | |||
*Hanging wet mops and cloths to dry | |||
====Services==== | |||
The following should be provided: | |||
*A stainless steel hand basin with elbow taps and a gooseneck outlet, and tiles above it with a mirror, soap dispenser and paper towel dispenser | |||
*A drip sink with a hinged bucket grid for cleaning mops ('''not a slop-hopper)''' | |||
==== | ====General requirements==== | ||
The following should be provided: | |||
*Small worktop on which to write | |||
*Hooks on which to hang tops | |||
*A lockable cupboard with shelves for cleaning materials, disinfectants, disposable gloves, soap, cleaning detergents, new mops and brooms, cleaning cloths, paper towels, toilet paper, etc. | |||
*A mop rack | |||
====Equipment==== | |||
The following should be provided: | |||
*Mops | |||
*A cleaning trolley | |||
*A polisher | |||
*Buckets | |||
[[File:Drawing_13_1.png|alt=|none|thumb|Drawing 13: Cleaning station and cleaners trolley]] | |||
DRAWING 13: CLEANING STATION AND CLEANERS TROLLEY | |||
===Clinical workstation=== | |||
==== | ====Description and function==== | ||
This is a work area separate to the nurses’ station. The clinical workstation area is required for clinical staff to make file notes, do patient administration, discuss cases and do research. For planning purposes, a 28- to 32-bed inpatient unit will require a work space for four staff members at a time. | |||
====Location and relationships==== | |||
The space should be positioned close to the nurses’ station, with privacy from inpatient unit activities. | |||
====Activities==== | |||
Provision should be made for the following: | |||
*Making and receiving phone calls | |||
*Writing reports | |||
*Accessing and printing data from a computer | |||
*Recording patient information in patient files and filing printed reports | |||
*Digital radiology screens | |||
*Case discussion and peer support | |||
====Services==== | |||
Provision should be made for the following: | |||
*Two telephones | |||
*Three data points | |||
*An X-ray viewing panel if required | |||
*Power outlets for two computers, a fax machine and a printer | |||
*Power outlet for a digital X-ray monitor and keyboard | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*A suitable workspace for the clinical staff and doctors to do clinical administration at the station with space for computers, telephones, printing and administrative work | |||
*A work surface and space for filing, shelves to accommodate files and stationery with drawers and cupboards | |||
*All surfaces must be impervious and designed for easy cleaning | |||
*Wall-mounted wipeboard and pinboard | |||
====Equipment==== | |||
*Two telephones | |||
*Three data-connected computers and digital X-ray equipment | |||
*Printer | |||
*X-ray viewing | |||
*Power outlets for two computer points and two central monitors | |||
=== | [[File:Drawing_14.png|alt=|none|thumb|372x372px|Drawing 14: Clinical work station example]]<div style="margin-left:0cm;margin-right:0cm;"> | ||
===Dirty utility=== | |||
====Description and function==== | ====Description and function==== | ||
The dirty utility room is the waste disposal room providing for the temporary storage of contaminated waste, sharps, soiled linen and recyclables prior to removal. A minimum area of 8 m² is required. | |||
====Location and relationships==== | ====Location and relationships==== | ||
The dirty utility room must be located at the exit to the inpatient unit to allow for ready access from the service exit. It should preferably be adjacent to the sluice. The dirty utility room should have easy access to hand-washing facilities and must have direct access to the passage of the inpatient unit. | |||
====Activities==== | |||
Provision should be made for the following: | |||
* | *Temporary storage of sluiced and dirty linen | ||
* | *Temporary storage of waste bins | ||
*Temporary storage and collection of canvas bags filled with dirty linen(± four bags a day per inpatient unit) | |||
*Collection of refuse | |||
====Services==== | |||
The following should be provided: | |||
*A hand basin with elbow taps and a gooseneck outlet with tiles above it, soap dispenser and paper towel dispenser | |||
* | |||
=====General requirements===== | |||
The following should be provided: | |||
*Space for dirty linen trolley, as well as sluiced trolley | |||
*Storage space for sharps, medical waste and domestic waste | |||
*Bumper rails to prevent bins from marking walls | |||
*Space for four large medical waste boxes (these may be stackable) | |||
*A bumper rail to protect the behind the trolleys | |||
*Good ventilation | |||
[[File:Drawing_15.png|alt=|none|thumb|Drawing 15: Dirty utility room example]] | |||
=== | ===Inpatient unit kitchen=== | ||
====Description and function==== | ====Description and function==== | ||
The kitchen is used for preparing and heating refreshments, snacks for patients, washing cups, and storing food supplements and snacks. The ward refreshment and food trolley is parked in the kitchen. A minimum area of 8 m² is required, increasing by 1.5 m² for every 10 beds (12 m² per 32 bed inpatient unit) | |||
====Location and relationships==== | ====Location and relationships==== | ||
The kitchen should have easy access to patient areas and the passage of the main inpatient unit | |||
====Activities==== | ====Activities==== | ||
Provision should be made for the following: | |||
*Two people at any given time | |||
*The preparation of hot or cold beverages for patients | |||
* | *Heat refreshments, snacks and some meals | ||
*In some rural, washing utensils and storing them in the inpatient unit kitchen | |||
====Services==== | ====Services==== | ||
Provision should be made for the following: | |||
*A double-bowl sink with drainage and hot and cold water | |||
*A microwave oven | |||
*Four power outlets for the hot-water supply unit, 120 ℓ fridge/freezer combination and microwave, plus one extra point | |||
*Continuous hot-water supply (hydro boil) unit placed over the sink drainage | |||
*A stainless steel hand basin with a paper towel holder and soap dispenser | |||
*A double-bowl sink with drip trays | |||
*Cupboards for keeping detergents, cups, saucers and glasses | |||
====General requirements==== | |||
Provision should be made for the following: | |||
It may be in-house or outsourced | |||
Suitable workspace and floor covering is needed that is easy to maintain | |||
====Equipment==== | |||
Provision should be made for the following: | |||
*Continuous hot-water supply unit | |||
*120 ℓ fridge/freezer combination | |||
*Microwave oven | |||
*Tea trolley | |||
*Food trolley (from main kitchen) | |||
*Bump rail for food and tea trolley | |||
*Refuse bin(e.g pedal bin) | |||
[[File:Drawing_16.png|alt=|none|thumb|Drawing 16: Ward kitchen examples]] | |||
=== | ===IT room (size dependent on the clinical brief and hospital)=== | ||
====Description and function==== | ====Description and function==== | ||
Switch room to house computer services, which are connected to the main server. | |||
====Location and relationships==== | ====Location and relationships==== | ||
Adjacent to the inpatient unit and may be shared by other facilities on the same floor level. | |||
====Services==== | ====Services==== | ||
Provision should be made for the following: | |||
*Data cabling to specialist approval and design | |||
*Power points to be specified by the IT specialist | |||
* | *Access control may be required | ||
* | |||
====General requirements==== | ====General requirements==== | ||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
Provision should be made for the following: | |||
*Size depends on the number of facilities connected to the equipment contained in the room. A minimum of 2m x 2m is recommended | |||
*The planning of this room must be coordinated with the IT consultants and the clinical staff. | |||
===Nurses’ station=== | |||
====Description and function==== | |||
The nurses’ station is the administrative base and communication centre for the inpatient unit and the enquiry point for patients and visitors. It provides a focal point to which all staff, whose time is mostly spent with patients, can return to record data, issue and receive information and receive verbal and written instructions. It provides for the coordination of patient care, observation, writing up of clinical notes, entering data into computers, and making and receiving phone calls. The station must accommodate nurses, an inpatient unit clerk, and, at times, doctors. | |||
The area controls the movement of patients, staff and visitors entering and leaving the unit and can receive mail, flowers and a variety of other items that may be delivered to the unit. The inpatient unit clerk or receptionist is generally located in this area with ready access to files and stationery. One nurses’ station in an inpatient unit, central to the bed units, will allow for the observation of the main patient areas and, where possible, people entering and exiting the inpatient unit | |||
For planning purposes, a 28- to 32-bed inpatient unit will require a nurses’ station of 14 to 18 m². | |||
====Location and relationships==== | |||
Decentralised nurses’ stations may be considered for immediate work associated with patient care: the review of patient notes, files and tests (short work). This is facilitated by the use of electronic record systems and point-of-care management. The floor area of the nurses’ station will vary according to the activities and services required. | |||
====Activities==== | |||
Provision should be made for the following: | |||
*Management of the clinical service requirements | |||
*Access to the electronic patient system | |||
*Making and receiving phone calls | |||
*Writing reports | |||
*Updating the patient bed allocation board | |||
*Accessing and printing data from a computer | |||
*Recording patient information in the patient’s file and filing printed reports | |||
*Controlling the nurses’ call system | |||
*Monitoring service alarms (e.g. fire alarm system) | |||
*Managing the key cupboard | |||
*Managing digital radiology information | |||
*Providing a contact point for doctors and nurses | |||
====Services==== | ====Services==== | ||
Provision should be made for the following: | |||
*Two telephones | |||
*Two data points | |||
*Six power outlets (for two computers and screens, a fax machine and printer) | |||
*Hands-free clinical hand basin, elbow taps, a mirror, paper towel holder, soap dispenser and wall-mounted waste paper bin | |||
*Nurse call system connected to a display panel at the nurses’ workstation or mounted on the wall directly behind the nurses’ station | |||
*Fire alarm/smoke detection panel mounted on the wall directly behind the nurses’ station | |||
*Alarm panel for gas and water mounted on the wall directly behind the nurses’ station | |||
*Power outlet for digital X-ray monitor and keyboard | |||
*Access control (inpatient unit entrance and exit plus dirty utility outside door) | |||
*Emergency power and uninterrupted power supply (UPS) | |||
*Access control panels at the inpatient unit’s entrance and exit, including the outside door of the dirty utility | |||
*Medical gas shut-off valves in visual control and within easy reach of the nursing staff | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Positive air pressure to allow for fresh air and reduce the risk of airborne diseases | |||
*Large workstation with a view of the entrance, and optimal observation of the most acute patients | |||
*Suitable workspace for the inpatient unit clerk (should no separate office be provided) and the nurses to work at the station with space for two computers, two telephones and a printer | |||
*Work surface and space for filing, shelves to accommodate files and stationery with drawers and cupboards, i.e. 20 lever-arch files (for policy documents, etc.) in a cabinet, ten lever-arch files in cupboards below the work station, plus space for 30 different types of forms (all A4) in pigeon holes above the work station | |||
*All surfaces must be impervious and designed for easy cleaning | |||
*Access to pneumatic system for laboratory samples (regional hospitals –dependent on the hospital size; tertiary hospitals as standard) | |||
*Air conditioning : ± 22 °C | |||
*Space for a dictionary and reference books | |||
*A key cupboard mounted on the wall behind the nurses’ station | |||
*Space to store and recharge haemoglobin and glucose meters | |||
*Space to store and recharge diagnostic sets | |||
*Space for the patient allocation board | |||
*Space for an adult scale with length meter | |||
*Space for an emergency trolley | |||
*Space for an oxygen cylinder on a mobile stand | |||
*Space for three observation trolleys or mobile non-invasive blood pressure (NIBP) machines | |||
*Wall-mounted wipe board and pin-board | |||
==== | ====Fittings==== | ||
Provision should be made for the following: | |||
*Counter,with sitting space for at least four people | |||
*Above- and under-worktop storage space for policy manuals, registers and report documentation | |||
*Access to medical gas shut-off valves must be in visual control and within easy reach of the nursing staff | |||
*Space for two telephones, two computers and a printer, the nurse call panel, fire alarm and smoke detection panel, and medical gas and vacuum supply. | |||
====Equipment==== | |||
Provision should be made for the following: | |||
*Patient admission board (whiteboard marked into bed units, the beds in each unit, the patient's name, the doctor's name and comments) | |||
*Key cupboard | |||
*Wall clock | |||
*Pin-board | |||
*Whiteboard (small - stock ordering notes, for instance) | |||
[[File:Drawing_17.png|alt=|none|thumb|Drawing 17: example of Nurses’ station]] | |||
===Patient kitroom=== | |||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
====Description and function==== | ====Description and function==== | ||
The provision of a kitroom could require a central or unit kitroom. The recommended minimum unit size of 6 to 8 m² is suggested. The room is used for the safe storage of patients’ clothes and belongings, excluding valuables and money. | |||
====Location and relationships==== | ====Location and relationships==== | ||
<div style="margin-left: | <div style="margin-left:0.018cm;margin-right:5.443cm;">The kitroom should be provided off the main passage. | ||
====Activities==== | ====Activities==== | ||
Provision should be made for the following: | |||
*Clear plastic bags tagged with patient identification | |||
*Bags to be locked away in mesh wire baskets | |||
*Clearly marked plastic bags to be received with patient's belongings | |||
*Receipt to be provided to the staff member | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*The store should be lockable | |||
*Slated shelving is required | |||
*Mesh wire cupboard | |||
*Good ventilation | |||
===Sluice=== | |||
====Description and function==== | |||
The sluice makes provision for the following: | |||
*Decontamination and storage of patient utensils such as bed pans, urinals and bowls | |||
*Cleaning and holding used medical instruments for collection ans sterilisation at CSSD | |||
*Testing and disposing of patient specimens | |||
A minimum area of 10 m²is required. | |||
====Location and relationships==== | |||
The sluice must be located centrally to the bed units to allow for ready access from the patient areas.The sluice room must have direct access to the inpatient unit passage and close proximity to the dirty utility | |||
====Activities==== | |||
Provision should be made for the following: | |||
*Sluicing, cleaning, disinfecting and storing bed pans, urinals, sputum mugs and wash basins | |||
*Urine testing and temporary storage of laboratory samples | |||
*Washing and temporary storage of medical instruments | |||
*Safe usage, service and maintenance of automatic bedpan washer | |||
*Hand washing by staff upon entering and before leaving the room | |||
====Services==== | |||
Provision should be made for the following: | |||
*A stainless steel clinical hand basin with elbow taps and a gooseneck outlet with tiles above it, soap dispenser and paper towel dispenser | |||
*A double deep-bowl stainless steel sluice sink unit with elbow taps and a gooseneck outlet, as well as a hand-held shower on a flexible hose | |||
*An automatic bedpan washer and power outlet at 1100 AFFL (ensure that the choice of the type of bed pan washer is made early in the design phase to enable adequate provision for drainage) | |||
*A single stainless steel sink with workspace for washing medical instruments | |||
*An extraction air diffuser | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*A stainless steel work surface next to the sluice for urine testing | |||
*A wall-mounted rack for clean bedpans and urinals | |||
*Cupboards fir storage of sputum mugs, detergent for the automatic bedpan washer, urine testing sticks and equipment | |||
*Shelves for wash basins and buckets | |||
* | *Good ventilation | ||
* | *Bumper rail to protect the wall behind the trolleys | ||
* | *Clinical hand basin adjacent to the entry door | ||
* | *Clean medical waste box storage needs to be considered in relation to the sluice | ||
* | |||
====Equipment==== | |||
Provision should be made for the following: | |||
*Bed pans and urinals | |||
*Urine bottles | |||
*Wash bowls | |||
[[File:Photograph_4.png|alt=|none|thumb|401x401px|Photograph 4: Examples of sluice room equipment]]<br />[[File:Drawing_18.png|alt=|none|thumb|Drawing 18: Sluice room example]] | |||
===Store for clean linen=== | |||
====Description and function==== | ====Description and function==== | ||
Provision should be made for the storage of clean linen, blankets and hospital-issued patient attire or patient theatre attire. A minimum size of 8 m² is required. Allocate a minimum of 0.16 m² of linen per patient and make allowance for storing and packing the linen trolley in the room. | |||
Storerooms are best designed in the elongated rectangular shape to allow easy access to all items . | |||
====Location and relationships==== | ====Location and relationships==== | ||
Provision should be made for the following: | |||
*Located within view of the nurses's station | |||
*Easily accessible to all patient areas | |||
*Directly off the main inpatient unit passage | |||
====Activities==== | ====Activities==== | ||
Provision should be made for the following: | |||
*One to two people at any given time | |||
*Counting linen | |||
*Unpacking received linen (mostly in canvas bags) | |||
*Loading clean linen onto the linen trolley | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Lockable door (undercut door for ventilation) | |||
*Perforated or slated shelving Need to make provision for supplies over weekends and private holidays in rural areas | |||
==== | ====Equipment==== | ||
Provision should be made for the following: | |||
*A clean linen trolley | |||
[[File:Drawing_19.png|alt=|none|thumb|Drawing 19: Linen room examples]][[File:Photograph_5.png|alt=|none|thumb|Photograph 5: Examples of linen trolleys and linen storage]] | |||
=== | ===Store for consumables=== | ||
====Description and function==== | ====Description and function==== | ||
Safe storage should be provided for the storage of clinical consumable items, like intravenous fluids and sets, syringes, needles, bandages, etc. Provision should be made for a minimum size of 9 m² per 28- to 32-bed inpatient unit. Allow 0.183 m² stock area per patient. | |||
====Location and relationships==== | |||
The consumables store should be centrally located close to the clean utility and have direct access to the inpatient unit. | |||
==== | ====Activities==== | ||
Provision should be made for the following: | |||
*Two people at any given time | |||
*Storage of consumable items on wall-mounted shelves | |||
*Allow enough space for the transfer of items from a trolley onto the shelves | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*The store should be lockable | |||
*Slated shelving is required | |||
*Sturdy wall-mounted shelving | |||
*The ability to identify and 'partition' stock (risk management) | |||
*Sturdy wooden and moulded plastic pallets on the floor( ±120 mm high) for the storage of intravenous fluids - only stack three boxes high | |||
*Ensure controlled temperature - a maximum of 26 °C | |||
*No items to be stored on the floor | |||
====Equipment==== | ====Equipment==== | ||
Provision should be made for the following: | |||
*Intravenous fluids, sets, syringes, needles, bandages, etc. | |||
[[File:Photograph_6.jpg|alt=|none|thumb|Photograph 6: Consumables stockroom]] | |||
===Equipment store=== | |||
====Description and function==== | |||
The equipment store is used for the safe storage of medical equipment, traction accessories, the parking of mobile IV poles, wheelchairs, lifting poles, bed cradles and commode chairs. Plugs and shelves are available for recharging and storing electrical equipment. A minimum size of 12 to 20 m² is recommended. This will vary in larger hospitals with 400 or more beds. | |||
====Location and relationships==== | |||
</div>The equipment store should be centrally located in a low-traffic area, have direct access to the inpatient unit passage and be close to the sluice as equipment may require cleaning and disinfection before storage. | |||
====Activities==== | |||
Provision should be made for the following: | |||
*One or two people at an one time | |||
*Moving equipment in and out of the store | |||
*Placing equipment on shelves and plugging in to power | |||
====Services==== | ====Services==== | ||
Provision should be made for the following: | |||
* | *Ten power outlets (depending on the facility) above the worktop to recharge equipment batteries | ||
====General requirements==== | ====General requirements==== | ||
Provision should be made for the following: | |||
*The store should be lockable | |||
*A counter top to recharge small equipment | |||
* | *Shelving to store traction units and small equipment | ||
*An open wall area where equipment mounted on trolley can be stored | |||
*A minimum 2.5 m internal width is suggested | |||
*Double door access | |||
====Equipment==== | |||
Equipment will vary according to the level of care. This will also serve as a guideline for the number of power outlets, as well as thee floor and workspace that is required [[File:Drawing_20.png|alt=|none|thumb|Drawing 20: Equipment store example]] | |||
=== | ===Medicine store=== | ||
====Description and function==== | ====Description and function==== | ||
The purpose of the medicine store is the safe storage of scheduled medication. | |||
The | ====Location and relationships==== | ||
It should be in full view of the nurses' station, preferably directly behind the nurses' station. | |||
====Activities==== | ====Activities==== | ||
Provision should be made for the following: | |||
*Two people at any given time | |||
*Placing and removing medicine on shelves, in refrigerators and in-wall mounted drug cupboards | |||
* | *Storing and loading the medicine trolley used during the inpatient unit round | ||
*Counting drugs | |||
* | |||
* | |||
====Services==== | ====Services==== | ||
Provision should be made for the following: | |||
*Clinical hand basin with elbow taps and gooseneck outlet with tiles above it, soap dispenser and paper towel dispenser | |||
*Access control recording everyone going in and out the room | |||
*Power outlet for the refrigerator | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Safe storage of medicine on shelves, in refrigerators and in wall-mounted drug cupboards | |||
*Shelving | |||
*Storage space for the medicine trolley used during the inpatient unit rounds | |||
<div style="margin-left: | ====Equipment==== | ||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
Provision should be made for the following: | |||
* | *Wall-mounted drug cupboard | ||
*Medicine trolley | |||
*Refrigerator with a thermometer and power outlet | |||
* | |||
* | |||
[[File:Drawing_21.png|alt=|none|thumb|Drawing 21: Medicine store example]][[File:Photograph_7.png|alt=|none|thumb|325x325px|Photograph 7: Examples of medicine trolleys]] | |||
==== | ==Staff facilities== | ||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
===Staffroom=== | |||
====Description and function==== | |||
The staffroom is used by the staff for respite and relaxation during tea and meal breaks, especially where it is difficult for staff to use centrally located facilities at night. It may also be used for staff meetings and tutorials. It has facilities for preparing and/or heating refreshments, snacks and meals, washing utensils and disposing of food waste. | |||
A minimum area of 15 m² is required. Size depends on the number of staff members using the facility and the usage of the facility. Allow 1.5 m² per person, assuming that a maximum of 40% of the inpatient unit staff will utilise the room at any one time. | |||
<div style="margin-left:0.018cm;margin-right:0.654cm;">In district and regional hospitals, the staffroom may also be used as a training area. </div> | |||
<div style="margin-left: | |||
====Location and relationships==== | ====Location and relationships==== | ||
The staffroom must be located away from the patient, treatment and visitor areas. | |||
Staff toilets should not be en suite to staffrooms, but should be located close to the staff restroom. | |||
The staff restroom could be shared between two inpatient units, or one space could be provided per floor. | |||
====Activities==== | |||
Provision should be made for the following: | |||
*Four people at a time | |||
*Resting or seated | |||
*Reading and writing | |||
*Eating meals | |||
*Holding meetings | |||
====Services==== | ====Services==== | ||
Provision should be made for the following: | |||
* | *Stainless steel double-bowl sink with drainage and hot and cold water | ||
*Hydro boil positioned over the drainage sink | |||
* | *Four power points for appliances | ||
* | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Facilities for food warming and beverage preparation and storage should be provided | |||
*Wall-mounted cupboard to store cups, glasses and consumables (tea, coffee,milk, etc.) | |||
*Undercounter cupboard to store cutlery and cleaning materials | |||
*Staff toilet should be next to, but not directly off the staffroom | |||
*A relaxed ambiance is essential | |||
====Equipment==== | |||
<div style="margin-left:0cm;margin-right:0cm;"> | |||
Provision should be made for the following: | |||
*Easy chairs | |||
*Table with chairs | |||
*Shelving for books and magazines | |||
*Whiteboard for daily notices (size: 1 m x 1.5 m) | |||
*Pinboard | |||
*Microwave oven - stainless steel, 40 ℓ, 1000 watts | |||
*120 ℓ fridge/ freezer combination | |||
[[File:Drawing_22.png|alt=|none|thumb|Drawing 22: Staffroom example]] | |||
===Staff locker area=== | |||
====Description and function==== | |||
Lockers are to be provided for staff to store their personal possessions. | |||
==== | ====Location and relationships==== | ||
Lockers should be positioned in a passage leading to the staffroom, in the staff room or opposite the nurses' station. This is to ensure that anyone tempering with lockers can be seen immediately. | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Secure storage of personal property | |||
*Locker sixe: 450 wide x 600 deep x 900 high with a bar to hang items on or 450 wide x 600 deep x 450 high, depending on requirements | |||
[[File:Figure_22.jpg|alt=|none|thumb|Figure 22: Typical staff lockers]] | |||
=== | ===Staff toilet=== | ||
====Description and function==== | ====Description and function==== | ||
This is a room containing a toilet and hand basin for staff use. A minimum of 3 m² is recommended. (No urinals should be installed.) | |||
====Location and relationships==== | ====Location and relationships==== | ||
<div style="margin-left:0.018cm;margin-right:0.654cm;">Toilets for staff use should be readily accessible from staff working areas. They should be located central to the inpatient unit. | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Wall-fixed toilet for cleaning underneath | |||
*Bathroom accessories | |||
*Mirrors - height and size is important for those using the facility | |||
*Soap dispensers and hand towel dispensers | |||
*Toilet roll holders in all toilets | |||
= | [[File:Drawing_23.png|alt=|none|thumb|460x460px|Drawing 23: Staff toilet example]] | ||
===Clinical overnight sleeping facilities=== | |||
==== | ====Description==== | ||
Sleeping, rest and ablution facilities are provided for clinical staff working at night who are not required to be permanently on the inpatient unit but must be ‘on call’ should they be required. | |||
====Location==== | |||
These are located close to the unit that the clinical staff are called to. D.g. in the ICU unit, EU, theatres, diagnostic radiology unit, paediatric unit, maternity unit or close to the surgical and medical inpatient units. The facilities should preferably be in a quiet area away from the patient areas. | |||
====Services==== | |||
Provision should be made for the following: | |||
*One data point per bedroom | |||
*One double plug for computers | |||
*One power outlet adjacent to the bed for a bedside lamp | |||
*Toilet, shower and hand basin in shared ablution area | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Cupboard to hang clothes and store personal items | |||
*Wall hooks for coats | |||
====Equipment==== | ====Equipment==== | ||
Provision should be made for the following: | |||
*Bed and bedside table | |||
*Desk to write and work on the computer | |||
*Waste bin | |||
*Easy chair | |||
*Side lamp | |||
[[File:Drawing_24.png|alt=|none|thumb|Drawing 24: example of Clinical overnight sleeping facilities]]<br />[[File:Drawing_25.png|alt=|none|thumb|401x401px|Drawing 25: example of Two clinical overnight sleeping facilities with shared ablutions]] | |||
==Administration Areas== | |||
===Unit management office=== | |||
Department of Public Works, 2005, Space planning norms and standards for office accommodation used by organs of state. (Government notice 1665). Cape Town, South Africa: Government Gazette. | |||
====Description and function==== | ====Description and function==== | ||
Depending on the level of care, offices are provided for nurses managers and, in some instances, for clinical heads of departments. Each office should provide accommodation for a single-person office to be used for clinical purposes. The office should have natural ventilation and a view to the outside. A minimum of 9 m² is recommended for clinical staff and 12 m² for a unit manager. | |||
The | ====Location and relationships==== | ||
The office of the unit manager should be near the entrance to the inpatient unit, central to the nurses' station and located away from the clinical areas and noise | |||
====Activities==== | |||
Provision should be made for the following: | |||
*Unit management writing reports | |||
*Shift handover meetings | |||
*Relative counselling | |||
*Staff management | |||
==== | ====Services==== | ||
Provision should be made for the following: | |||
*IT and data connections | |||
*Three electrical points and data point | |||
*Telephone point | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Desk and two chairs | |||
*Filing cabinet | |||
*Stationery cupboard | |||
*Pinboard | |||
*Lockable office | |||
</div> | |||
==== | ==Public areas== | ||
<div style="margin-left:0.018cm;margin-right:0.654cm;"> | |||
===Public entrance to the inpatient unit=== | |||
====Description and function==== | |||
There should be one main entrance to the inpatient unit. This should be the main access and exit to the inpatient facility. The fire escape should not be used as an entrance. In large facilities, provision is made for 400 beds and more. A general entrance and a service entrance are suggested. | |||
====Services==== | |||
Access control id required | |||
=== | ===Inpatient unit corridor=== | ||
====Description and function==== | ====Description and function==== | ||
Circulation space linking rooms should maximize the use of the space to support turning circles and ease of access. Size depends on where the corridor is located. | |||
====General requirements==== | |||
Natural light in patient areas is desirable.Waiting areas may be shared between inpatient units. Avoid any floor prostrutions that would influence wheels of beds and equipment. The width of a passage must allow at least two beds to pass in opposite directions, within the bumper rail measurement. The recommended minimum width for the main inpatient unit corridor (from bumper rail to bumper rail) is 2400 mm between bumper rails.[[File:Drawing_26.png|alt=|none|thumb|Drawing 26: Hospital passage requirements]] | |||
===Visitors' waiting area=== | |||
==== | ====Description and function==== | ||
An area for visitors and patients to wait prior to or during visits to the inpatient unit is best located outside the perimeter of the inpatient unit and may be shared by more than one unit. | |||
Where visitors' lounge or waiting room is provided, it should be located and designed to accommodate child visitors without disruption to others. A room of 10 m² or 0.5 m² per able-bodied person is recommended, with 1 m² to be included per wheelchair-dependent person. | |||
====Location and relationships==== | |||
The waiting area requires direct access to the circulation corridor and ready access to the public amenities. If a waiting area at unit level is provided, it should be located near the entrance to the unit. An external outlook is preferred with good natural light. | |||
==== | ====Activities==== | ||
Provision should be made for the following: | |||
*Visitors sitting or standing, and children playing | |||
====Services==== | ====Services==== | ||
Provision should be made for the following: | |||
* | *One double plug | ||
====General requirements==== | ====General requirements==== | ||
Provision should be made for the following: | |||
*Natural light is desirable | |||
*Waiting areas may be shared between inpatient units | |||
*A play area for children | |||
*General and disabled-friendly ablutions | |||
====Equipment and furniture==== | |||
Provision should be made for the following: | |||
*Vending machine | |||
*Public phones | |||
*Waste paper or refuse bins | |||
*Chairs | |||
*Side tables | |||
===Public disabled toilet=== | |||
====Description and function==== | |||
A room containing a toilet and a hand basin for use by disabled persons with or without assistance is required. A minimum size of 5 m² is recommended. | |||
====Location and relationships==== | |||
The disabled toilet should have direct access to a waiting or circulation passage. Disabled toilets for public use should be readily accessible for public areas. | |||
====General requirements==== | |||
Provision should be made for the following: | |||
*Toilets at a special height for wheelchair users | |||
*Clinical hand basin with elbow taps accessible for paraplegics while still siting on the toilet | |||
*Wall-fixed toilet for cleaning underneath | |||
*Mirrors - height and size is important for those using the facility | |||
*Soap dispensers and hand towel dispensers - , hands-free | |||
*Toilet roll holders in all toilets | |||
*The door is to be fitted with escape hardware to allow staff access in case of an emergency | |||
==== | [[File:Drawing_27.png|alt=|none|thumb|Drawing 27: Toilet for the disabled]][[File:Photograph_8.jpg|alt=|none|thumb|Photograph 8: Provision for emergency trolley]][[File:Drawing_28.png|alt=|none|thumb|Drawing 28: Clinical hand basin configure]][[File:Drawing_29.png|alt=|none|thumb|Drawing 29: Wheelchair Bay]] | ||
==Engineering Considerations== | |||
</div><u>''Refer to IUSS: GNS Building Engineering Services''</u> | |||
* | *Vacuum, piped oxygen and medical gases | ||
* | *Service panels enclosing oxygen, suction and air outlets | ||
* | *Ventilation | ||
*Fire detection and alarm systems | |||
*Resilience of electrical supplies | |||
*Lighting systems | |||
*Internal drainage | |||
*Nurse call system | |||
*Security system | |||
==Standard Components== | |||
Standard Components (SC) refer to rooms and spaces for which room data sheets, room layout sheets (drawings) and textual descriptions '''have been developed and are available in a separate section of these guidelines. ''' | |||
==List of rooms== | |||
The electrical, mechanical and health technology requirements for each space are given. There are a number of software packages that plot the equipment listed in the library with regard to the design in process. | |||
The value of this type of system is that conflict of design principles can be detected early, such as door openings, spaces and the sizes of rooms in relation to the equipment for the space. (Code Book is a database system that could facilitate the development of a library for future use, Revit is a 3D design program) | |||
Table 7: Example list of rooms for a 32-Bed inpatient unit | |||
{| class="wikitable" | |||
|+ | |||
!Code | |||
!Room | |||
!Quantity | |||
|- | |||
| | |||
| colspan="2" |'''Patient area''' | |||
|- | |||
| | |||
|2-bed unit | |||
|1 | |||
|- | |||
| | |||
|4-bed unit | |||
|7 | |||
|- | |||
| | |||
|En suite bathroom | |||
|10 | |||
|- | |||
| | |||
|Entrance | |||
|1 | |||
|- | |||
| | |||
|Single room | |||
|2 | |||
|- | |||
| | |||
|Patient toilet | |||
|1 | |||
|- | |||
| | |||
|Day room | |||
|1 | |||
|- | |||
| | |||
|Assisted shower | |||
|1 | |||
|- | |||
| | |||
| colspan="2" |'''STAFF AREAS''' | |||
|- | |||
| | |||
|Office - Sister | |||
|1 | |||
|- | |||
| | |||
|Office - Doctor | |||
|1 | |||
|- | |||
| | |||
|Nurse's station | |||
|1 | |||
|- | |||
| | |||
|Staff shower | |||
|1 | |||
|- | |||
| | |||
|Staff toilet | |||
|1 | |||
|- | |||
| | |||
|Staffroom | |||
|1 | |||
|- | |||
| | |||
|Staff locker area | |||
|1 | |||
|- | |||
| | |||
| colspan="2" |'''SUPPORT AREAS''' | |||
|- | |||
| | |||
|Bay - Hand-washing | |||
|10 | |||
|- | |||
| | |||
|Bay - Resuscitation trolley | |||
|1 | |||
|- | |||
| | |||
|Cleaners' room | |||
|2 | |||
|- | |||
| | |||
|Clean utility | |||
|1 | |||
|- | |||
| | |||
|Dirty utility | |||
|1 | |||
|- | |||
| | |||
|IT room | |||
|1 | |||
|- | |||
| | |||
|Sluice - Clean linen | |||
|1 | |||
|- | |||
| | |||
|Store - Equipment | |||
|1 | |||
|- | |||
| | |||
|Store - General | |||
|1 | |||
|- | |||
| | |||
|Store - Patient kit | |||
|1 | |||
|- | |||
| | |||
|Store - Surgical | |||
|1 | |||
|- | |||
| | |||
|Toilet - Disabled/ public | |||
|1 | |||
|- | |||
| | |||
|Visitors waiting area | |||
|1 | |||
|- | |||
| | |||
|Inpatient unit kitchen | |||
|1 | |||
|- | |||
| | |||
|CIRCULATION | |||
|32% | |||
|} | |||
='''List of abbreviations'''= | |||
ACDP Advisory Committee on Dangerous Pathogens | |||
ACH Air changes per hour | |||
AHIA Australian Health Insurance Association | |||
AII Airborne infection isolation | |||
BP Blood pressure | |||
CCD Central Cleaning Depot | |||
CDC Centres for Disease Control | |||
CSSD Central Sterile Services Department | |||
ECG Electrocardiogram | |||
HCU High care unit | |||
HEPA High-efficiency particulate absorption | |||
HIS Hospital information system | |||
ICT Information and communication technology | |||
ICU Intensive care unit | |||
NDoH National Department of Health | |||
NHLS National Health Laboratory Service | |||
NHS National Health Service | |||
NIBP Non-invasive blood pressure | |||
PACS Non-invasive blood pressure | |||
PAS Patient administration system | |||
PE Protective environment | |||
RIS Radiology information system | |||
SARS Severe Acute Respiratory Syndrome | |||
SC Standard components | |||
TB tuberculosis | |||
UPS Uninterrupted power supply | |||
='''References'''= | |||
Centers for Disease Control and Prevention (CDC), 2003. Guidelines for environmental infection control in health-care facilities. (Recommendations of CDC and the healthcare infection control practices advisory committee HICPAC). Atlanta, GA: CDC. | |||
Department of Health, 2011. Adult in-patient accommodation: Planning and design manual. (Version:2951: 2.4: England). London, UK: Department of Health. | |||
Growth Solutions Group (GSG), 2008. Specialist clinics wayfinding guidelines: The outpatient journey. [pdf] Victoria Australia: GSG. Available at: <nowiki>http://docs.health.vic.gov.au/docs/doc/B0C152FCA1338498CA25791700037BF4/$FILE/wayfindin</nowiki> g-guide.pdf [Accessed 31 March 2014]. | |||
NHS Estates, 2005. Ward layouts with single rooms and space for flexibility. The Stationery Office. | |||
Standards Association of Australia (SAA), 2003. AS 1428.1-4: Design for access and mobility. New South Wales Australia: SAA. | |||
The Centre for Health Assets Australasia (CHAA) faculty of the built environment the university of New South Wales (NSW), 2009. Wayfinding for healthcare facilities: Technical series TS-2: Prepared for: NSW health strategic business and development branch. (5th ed). NSW: NSW health department. | |||
International Organisation for Standardisation (ISO), 2014. ISO 7000:2014 Graphical symbols for use on equipment- Registered symbols. Switzerland: ISO. <br /><div style="margin-left:0cm;margin-right:0cm;"><div style="margin-left:0cm;margin-right:0cm;"><div style="margin-left:0cm;margin-right:0cm;"><div style="margin-left:0cm;margin-right:0cm;"><div style="margin-left:1.983cm;margin-right:0cm;"> | |||
<div style="margin-left:0.212cm;margin-right:0cm;"></div> | <div style="margin-left:0.212cm;margin-right:0cm;"></div> | ||
<div style="margin-left:0.212cm;margin-right:0cm;"></div> | <div style="margin-left:0.212cm;margin-right:0cm;"></div> | ||
[[Category:Clinical Services]] | [[Category:Clinical Services]]</div> | ||
[[Category:ICU]] | |||
Latest revision as of 10:38, 15 December 2020
Policy and Service Context
Policy context
Adult inpatient units provide suitable accommodation for the patient where diagnosis, medical and nursing care, and treatment can be provided effectively and economically.
The adult inpatient unit is the clinical unit in a hospital where patient bed space and clinical treatment space is combined. This combination allows the unit to provide patients with an effective, economical therapeutic unit for clinical diagnosis, medical treatment, and nursing care.
The inpatient unit environment needs to meet the requirements for safe nursing and clinical practice, adhere to health and safety standards, and meet recognised infection control principles, while maintaining the principle of patient privacy and dignity.
This document provides guidance on inpatient unit spaces and it should be read in conjunction with the full IUSS set of standards pertaining to an inpatient unit. Variations to the set standard for inpatient units will be noted where indicated.
Specialised guidelines for inpatient units for paediatrics, infectious diseases, i.e. tuberculosis, intensive care, obstetrics, rehabilitation, burns care, oncology and mental health care will be addressed in separate IUSS documents.
Service context
The business case and the health brief define the correct package of services and the required bed distribution per facility based on the Provincial Strategic Transformation Plan and the government policy document:Government Notice R. 185, 2 March 2012, National Health Act 61/2003Regulations: Categories of hospitals: No.35101
Table 1: Inpatient unit allocation per category of hospitalL
| District hospital | Regional hospital | Tertiary hospital | Central hospital | Specialist hospitals |
|---|---|---|---|---|
| General medical | Medical-Internal Medicine | Subspecialty Medical | Super specialties in the disciplines listed for tertiary care, including oncology | Tuberculosis(TB) Mental Health
Rehabilitation Infectious Diseases |
| General surgical | General surgical | Subspecialty Surgical | ||
| Specialty Surgical:
Gynaecology Orthopaedics Ophthalmology |
Subspecialty Surgical:
Gynaecology Orthopaedics Ophthalmology
| |||
| Paediatric | Paediatric | Subspecialty Paediatric | ||
| Maternity | Maternity | Subspecialty Obstetrics | ||
| High careӿ | High careӿ | |||
| Intensive Care Unitӿ | Intensive care underӿ supervision of a specialist intensivist | Specialist intensive careӿ | ||
| Mental Health
Observation Room and 72 hours beds |
Psychiatric
Inpatient Unit |
Specialist psychiatric |
*To be dealt with in separate documents
Determining inpatient unit size
Operationally successful inpatient units range from 28 to 32 beds per unit. The unit is subdivided into bed units that will provide for efficient management of patient acuity and flexibility. This guideline recommends 28 to 32 beds per inpatient unit.
All inpatient units should function as stand-alone units. These units contain one, two or four bed-, with six-bed configurations only being permissible in certain instances.
The inpatient unit should be planned to operate at an optimal occupancy level considering the model of care to be provided, staffing strategies, staff availability and operational aspects.-Hours of operation
Patient visitors
Personnel
Facility management, such as food services, linen services, cleaning services and maintenance support, is performed on a daily, weekly or intermittent basis.
Visiting, teaching and volunteering activities may also take place within the inpatient unit space.
Operational policies
The following policies are relevant to inpatient units:
| • Admissions | • Infection control |
| • Amenities for patients and visitors | • Linen management |
| • Amenities for staff | • Maintenance and engineering |
| • Cleaning | • Medication management |
| • Clinical information | • Operating hours |
| • Communication systems | • Pastoral care |
| • Complaints | • Risk management |
| • Recording of patients data | • Safety and security |
| • Disaster planning | • Sterilising services |
| • Discharge of patients | • Stores and supplies |
| • Equipment storage | • Waste management |
| • Food services | • Others to be determined |
Planning and Design
Overview
Adult inpatient units provide suitable accommodation for the patient where diagnosis, medical and nursing care, and treatment can be provided effectively and economically
This document attempts to illustrate the desired planning principles and design considerations for adult inpatient units.
Part B contains planning and design guidance, design considerations, functional relationships between hospital departments with respect to adult inpatient accommodation (inpatient units), and relationships within the inpatient unit itself.
Workflow diagrams are provided to explain the flow of patients, clinical staff, support goods and services, maintenance staff, as well as the public. Workflow diagrams within departments are provided to assist in understanding the intradepartmental relationships that support the functional flow in the inpatient unit to ensure productive service delivery.
The detailed room diagrams with accompanied norms and standards are provided to clarify understanding of the different space requirements and room specific specifications for an adult inpatient unit.
Design and planning principles
General design and planning principles
- Inpatient accommodation forms the core of a hospital and has functional relationships with most departments
- Patients enter the facility as inpatients, day patients or outpatients.
- The planning of the inpatient units should support planning principles that promote a holistic healing environment with, where possible, clear external views, consideration of noise levels, natural ventilation, as much morning sun or light as possible, and spaces that would create a pleasant healing environment.
- The design should reduce noise in the facility
- The design should make maximum use of natural light and views for patients and staff.
- The healthcare patient environment should be clinically safe and effective.
- The design should maximise patient safety and reduce the risk of errors and accidents.
- The work environment should be ergonomically safe and risk free.
- The design should avoid large sprawling layouts that are both resource and cost intensive.
- Workflow should be efficient and support effective resource utilisation.
- Appropriate space norms and room design should be implemented.
- The unit should comply with quality assurance principles.
- The unit should have communication and information systems that will support patient management and administration.
- Layouts should reflect the service needs of the patients in the inpatient unit.
- Beds should be clustered to facilitate staff efficiency, meal relief and optimal patient supervision, particularly at night when staffing levels are lower.
- The design should facilitate the delivery of care at the patient’s bedside or be proximal to the bedside whenever possible. This includes suitable services and supplies at the bedside.
- The environment should be aesthetically pleasing for patients and should assist staff in performing the required activities in the most efficient and supportive environment.
- Staff should not have to walk far to obtain supplies and equipment.
- The design should balance requirements for clinical need, and capital and recurrent budget considerations.
- The orientation of the inpatient units and aspect of inpatient accommodation should be prioritised in the development of the master plan. The orientation of the inpatient units should preferably face north or northeast, but a southern orientation is acceptable.
- If the prevailing wind direction is south, east and west orientations of inpatient units are discouraged.
- The placement of inpatient units must ensure patient privacy. Visitors, staff and service traffic through the inpatient units should be avoided.
- Inpatient units can be organised on the same level over a large floor area or they may be stacked into a multistorey block separate from diagnostic and treatment facilities, but closely linked. This allows more consistent planning of inpatient accommodation, increases flexibility in the way that beds can be organised, and enables maintenance and refurbishment to be carried out more easily.
- All pipes for sanitary requirements should be placed on external walls. Service support facilities and top-up of stores or pharmaceuticals and food delivery should be accessible to the inpatient units without compromising privacy or noise levels.
- The design should enable greater levels of observation in response to increased patient acuity.
- There should be enough space for activity at the bedside and other activities in the inpatient unit.
- There should be adequate storage space for bulky equipment.
- The area should be accessible to physically and sensory impaired people.
- The design should that make it possible to communicate administrative or clinical information from the bedside.
- The design should consider staff members’ and patients’ privacy for clinical treatment, bodily functions, personal care, and personal discussions and telephone calls
- Personnel – How many people are there at any given time in a specific place to perform a specific task or procedure?
- Activities – What procedures should be performed?
- Equipment – What equipment is required that will occupy the space?
- Security – What access control measures does the hospital management determine?
Human resources
Nursing models of care
Nursing care is the main activity that allows the effective and efficient functioning of the inpatient unit. The inpatient unit design should therefore ensure maximum patient observation and contact, with short travel distances for the staff.
Inpatient units should have no less than two single-bed units or more than four single-bed units per 32-bed inpatient unit.
Unit management and administration
If there is a ward clerk, he or she needs to be placed at the entrance to the ward and preferably at a small reception counter or at the nurses’ station. If the ward clerk is placed at the nurses’ station, additional space must be provided to accommodate the activities of the ward clerk.
The province’s policy with regard to staff facilities should indicate whether an inpatient unit staffroom or a shared restroom between inpatient units would be preferred. Staff toilets should be provided in each inpatient unit.
Teaching and training
Access and circulation
Service staff may access the ward through a second entrance, but it should be monitored for both safety and security. Waste should exit separately.
Infection control
Infection control considerations must include all healthcare workers. All areas of the facility shall be designed, constructed, furnished and equipped in keeping with the principles of infection control
The following aspects contribute to effective infection prevention and control and are relevant within the context of an inpatient unit:
- Hand hygiene facilities should be provided in all patient care areas, clinical areas and nurses’ stations.
- Hand hygiene facilities should be provided in areas where careful attention to hygiene is essential, such as kitchens, sluice rooms, utilities, medicine areas, bathrooms, toilets and change rooms.
- Hand basins must be visible to staff on entering and leaving the room. In addition, antibacterial hand rub dispensers should be provided at the entrance to each inpatient unit. Hand-wash facilities should also be placed in the main passage of the inpatient unit and next to the nurses’ station.
- Facilities should be provided to isolate infectious patients.
- The following facilities should also be provided:
- Linen handling
- Separation of clean and dirty work flows
- Storage
- Waste management
- Ventilation
- Surface finishes
- Careful aseptic technique and the observance of ‘standard precautions’
- The administrative infection control measures and protocols of the hospital should be followed and implemented in the design
Airborne infection isolation and protective environments
Protecting staff and visitors from infectious diseases is an important aspect of airborne infection isolation (AII). It should not be assumed that a well-designed and functional ventilation system provides sufficient protection for these persons. Personal protective equipment such as N95 or FFP2 respirators should be provided to all staff and visitors entering AII rooms. Where these persons are expected to enter such environments regularly, these persons should have themselves fit tested for respirator use.
Ceilings in AII and protective environment (PE) rooms shall be impervious monolithic structures to ensure excellent sealing and airtightness. Ceiling voids above these rooms, especially PE rooms, can be particularly hazardous spaces.
All swing doors shall be equipped with door closers to ensure that they remain shut when not in use. Hold-open devices are not recommended for these doors. Sliding doors are also not recommended as these pose difficulties in maintaining an adequate seal.
It is recommended that isolation rooms be provided with outside views where possible, without presenting a biosecurity risk. Privacy blinds should be installed, but these should not present a hygiene risk or hinder the nursing staff view of the patient.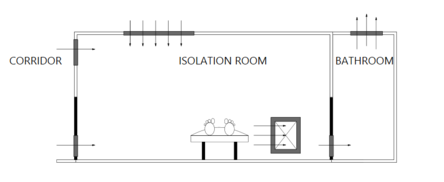
Negative pressure isolation is only required for patients presenting with airborne infections, for example, measles, Severe Acute Respiratory Syndrome (SARS), and TB. These infections spread primarily through the respiratory route where the infectious particles have a diameter of less than 5 µm. The unit for measuring ventilation is air changes per hour (ACH). In accordance with the national building regulations, isolation rooms shall be single occupancy with ventilation rates in excess of 12 ACH (including en suite bathrooms and anterooms). Where airborne contamination control in these rooms is achieved through dilution, these rooms shall have near perfect mixing with air change efficiencies approaching 50%. This implies that the ventilation efficiency in the isolation room shall be 50% as efficient as plug flow. Contamination removal effectiveness around the patient can be improved by placing an extraction point near the head of the bed. Airflow patterns within the room shall be developed so that the air shall flow from the passage door and air inlet terminal, across the patient and towards the bathroom and extraction points. Convergent fluctuations of only 5 Pa in each of two adjacent rooms can potentially reduce the pressure differential between the rooms by 10 Pa. For this reason, pressure differentials of 15 Pa between rooms are recommended. Lower pressure differentials are easier to achieve, but offer less safety under normal operational fluctuations condition.
The use of visual air pressure monitors between the passage and the isolation room is required. This enables a constant visual indication of the airflow direction between the isolation room and adjacent areas. These monitors should indicate the pressure magnitude, direction and out-of-specification failure limits. All major ventilation system components serving these areas should be clearly marked with the room identification, system identification and a biohazard sign.
Supply and extraction systems should be interlocked so that a failure of the exhaust air system shuts the air supply off, preventing the isolation room from going into an overpressure status. It is acceptable to install a balanced-blade pressure stabiliser to ensure that the room does not experience extremes of pressure under supply fan failure, control system failure, or severe transient environmental conditions. However, the inclusion of these devices can increase the design capacity of the system under normal operation.
Additional information regarding engineering services design and planning for airborne precaution rooms can be found in the IUSS Building Engineering Services Guideline.[1]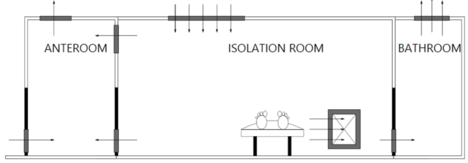
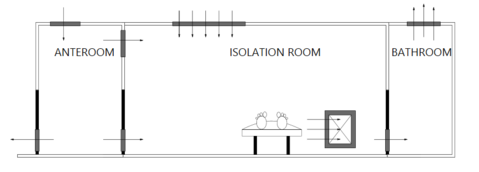
Respiratory protection needs not be worn in the anteroom in this scenario, as the anteroom is held at a relative pressure positive to the patient room.
While it may be tempting to develop positive pressure protective isolation rooms that can be adjusted to operate as negative pressure protective isolation rooms for airborne infection control, this practice is strongly discouraged, since it presents the inevitable scenario where the room is operated in an inappropriate mode for the wrong case, which places many people at risk of infection. The operation of neutral pressure rooms as a compromise is also not recommended as the negligible room permeability required for these rooms is not easily achieved or maintained.
Ergonomics in design
Designers should consider the optimum comfort of all situations for staff, patients and visitors.
Refer to:
- Alder, D. and Tutt, P. eds., 1992. New metric handbook : Planning and design data. Oxford: Reed Educational and Professional Publishing Ltd.
- Neufert, E. and Neufert, P., 2012. Neufert architects’ data. 4th ed. New York: John Wiley & Sons.
Universal access
- Mobility impaired
- Visually impaired
- Hearing impaired
Telecommunication and IT systems support
- Telecommunication system
- Nurse call to all patient areas with central control system
- Paging and personal telephones replacing some aspects of call systems
- Bar coding for supplies, X-rays and records
- Computer network connections in all management and patient administration and information systems:
- Hospital information system (HIS) and electronic patient records
- Patient administration system (PAS)
- Radiology information system (RIS) (digital X-rays)
- Picture archiving communication system (PACS)
- Laboratory with a link to the National Health Laboratory Service (NHLS)
- Pharmacy system
Wayfinding and signage
It is important to plot the various routes patients, visitors, suppliers and staff may have to travel to get to the inpatient facility from the car park, drop-off points and other departments in the hospital. Once these routes are established, principles can be applied to the design to assist successful wayfinding.
Ways to enhance wayfinding include the following:
- Printed information (pamphlets
- Architectural features and design elements that provide clues as to what the function of the building is and can include landscaping, sculptural features and architectural interior design
- Floor covering, lighting, wall, door and window graphics
- Permanent signage
- Digital devices (e.g. kiosks or information screens)
- Human interaction (e.g. human interaction at help desks)
The following core principles should be adhered to:
- Design that includes everyone, especially those who are more vulnerable, such as the following:
- The first-time visitor
- The physically challenged
- Those with some form of impairment
- Children
- Utilisation of standardised information systems
- Utilising ‘key hub’ destinations along a complex journey (a person is directed to a primary hub destination then directed on to a secondary hub destination from that point)
- Toponomy, giving names and numbers to places and functions
- A clear, simple wayfinding system
Signage is a critical ‘wayshowing’ component of wayfinding. Information displayed in the signage needs to comply with the following:
- Be organised and presented in a logical, sequential layout
- Contain a maximum of five destinations in the case of directional signs
- Be listed at the top of the hierarchy or highlighted as primary information in the case of key hospital hub destinations
- Be presented lower in the information hierarchy in the case of secondary destinations
- Be grouped and ordered with logic relevant to the destinations listed in the case of destinations on signs, either in alphabetical order according to the direction to the destination in clockwise order or according to the order of the distance to the destination (closer destinations first)
- Connect labels (destinations) to arrows
- Arrow designs should be based on the ISO arrow (ISO 7001)
- Colour coding of floors or as a method of differentiating space may be used, however, people do not always perceive that the colour use has significance. This is worse for people who are colour blind. It is, however, a useful component of the wayfinding system
- Signage should use the following:
- Accessible terminology – common references that everybody understands
- Avoid the use of acronyms and use universally understood symbols
- Provide clear contrast between the information content and its surrounding environment
- A finish that does not detract or obscure the signs intention
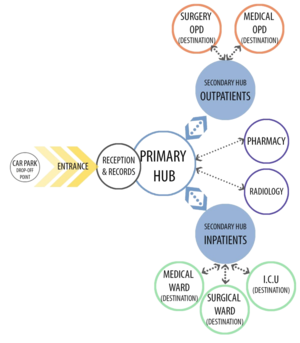

In the inpatient facility
Appropriate signage for all the internal rooms and the external buildings should make use of universal signage and should, take the provincial policy on signage and wayfinding into account as far as possible. Comprehensive signposting shall be provided for all hospitals. Signposting will clearly identify staff, patient and visitor areas. It will also draw attention to restricted areas.
General
Bed numbers shall be shown outside the patient bedroom. These shall be one number per bed. In bedrooms with more than one bed, all bed numbers or the range of numbers shall be shown on the sign outside each room. In bedrooms with more than one bed, each bed number shall also be displayed at the bed head.
The lettering style Helvetica Medium upper and lower case is generally recommended. Upper case only is recommended for the building’s main entrance sign.
Room signs
Non-illuminated, internal and external room function identification signs that are located on doors require the following considerations:
- The format should allow easy replacement of the sign or sign inset when the room function changes.
- Numbering on the inpatient units should be uniform, starting at the entrance with the first room on the left-hand side.
- Each bed in each unit must be numbered.
Patient information board
A whiteboard, which lists the patients that are currently occupying the beds, should be mounted on the wall behind the nurses’ station. The whiteboard should be a ‘wipe’ board with a suitable surface for nurses to add and erase the information. The information should be indicated as follows with lines drawn to separate each row and column:
Table 2: Example of the patient information board
| Bed no | Patient name | Doctor | Date in | Date out | Notes |
|---|---|---|---|---|---|
|
|
|||||
|
|
The patient information board should be supplied and fitted by the contractor
Ventilation and air management
Adequate ventilation throughout the health facility is important as poor ventilation affects patients and staff, and puts them at risk of being infected with nosocomial diseases. It is therefore necessary to ensure that spaces are ventilated so that the quality of the air breathed is improved by diluting the air and removing pollutants that are harmful. The main aim is to provide ventilation that maintains thermal comfort and indoor air quality that reduces the risk of cross-infection. This can be achieved through natural, mechanical or hybrid methods of ventilation.
The chosen method will have a significant effect on the design of the inpatient unit.
Day- and night-time illumination
- All rooms should be provided with the required electrical illumination
- All patient beds should be provided with a reading light
- Night lights should be provided in passages so that they do not disturb patients
- Emergency lighting is critical in inpatient units such as paediatrics, theatres and ICU
Fire detection and alarms
Refer to Fire Regulations and SANS 10400 Regulations
- All inpatient units should have escape doors in case of fire
- The inpatient units should be provided with smoke detection systems
- Sprinkler systems are not recommended
- Fire extinguishers should be provided and slightly recessed so as not to cause obstruction
- All inpatient units should have an evacuation plan that is aligned with escape routes
Security
- Access to and from the inpatient unit
- Spaces that must be secured (medication store)
- Security in individual spaces of the unit
Supply and disposal
- Laboratory – collection of specimens
- Mobile X-rays
- Central stores – disposables, stationery, cleaning materials and new equipment
- Pharmacy – medicines and drugs, delivery of prescriptions and return of empty recyclable containers
- Central Sterile Services Department (CSSD) – sterile packs, return of opened unused packs and used recyclable equipment
- Linen store – clean linen, return of dirty linen
- Kitchen – patient meals (the size of the kitchen depends on the meal production and delivery processes involved)
- Central Cleaning Depot (CCD) – cleaning equipment
- Refuse – general waste (domestic), pathological waste for incineration, recyclable waste, sharps.
Material handling of inpatient unit supplies includes the following:
- To and from the laboratory – the collection of specimens
- Mobile X-ray equipment – space around patient beds and parking space for the equipment (a bay off the passage)
- From the central stores – delivery of disposables, stationery, cleaning materials and new equipment
- To and from the pharmacy – delivery of medicines and drugs, delivery of prescriptions and return of empty recyclable containers, sending of prescriptions to the pharmacy
- To and from the CSSD – delivery of sterile packs, return of opened unused packs and used recyclable equipment
- To and from the linen store – delivery of clean linen, sluicing of linen and return of dirty linen to the laundry
- To and from the kitchen – delivery of patient meals in a trolley, trolley parking in the inpatient unit and return of the utensils and cutlery in the trolley back to the main kitchen
- CCD – delivery and storage of cleaning equipment
- Refuse – removal of general waste (domestic), pathological waste for incineration, recyclable waste, sharps
- General hospital policies relevant to the various departments, such as linen supply and waste management, should be applied
Medication management
- Pharmacy staff should be consulted with regard to medication and intravenous fluids storage requirements for each inpatient unit.
- The inpatient unit depends on the pharmacy for pharmaceutical support. This includes inpatient unit medication, scheduled drugs, patient prescriptions and discharge medication. • Security and access control to medication rooms should comply with local legislative Government Gazette No 25872, Pharmacy Act, 2 January 2004 – jurisdiction requirements and the hospital policy.
- The location and design of the medication room should minimise travel distances, noise and disruption to staff undertaking medication-related activities in order to reduce error. All medication should be stored in a temperature-controlled, locked environment. The medicine trolley, inpatient unit stock and patient prescriptions should be stored in a medicine room that should be close to and directly visible from the nurses’ station.
- The management of intravenous fluids should be clarified for the specific facility as to the quantity to be stored within the clean utility room (inpatient unit bulk stock is kept in the surgical and medical storeroom with small quantities kept in the clean utility).
- If additives are introduced to intravenous fluids in the inpatient unit, it should occur in the clean utility room.
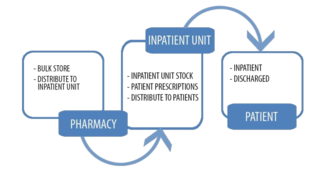
Options for dispensing within the inpatient unit
Lockable medication trolleys should be stored in the medicine storeroom behind or directly opposite the nurses' station so that the store is in full view of nurses at all times.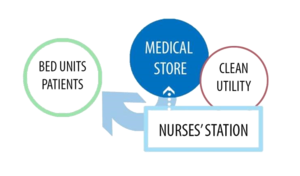
Equipment cleaning
Medical equipment: The operational narrative should guide whether reusable items will be processed in the inpatient unit or whether they will be sent to the CSSD
Beds: These are cleaned in the inpatient unit
Storage - equipment
The equipment store is intended for storage of equipment that has to be floor parked or stored on shelves and for equipment that may require the recharging batteries. The requirements will vary and need to be defined so that appropriate storage space is allocated according to the requirements of the inpatient unit and the needs of the patients and staff.
The equipment store should be located close to the sluice room, as equipment requires cleaning and disinfecting before storage.
Equipment should be organised so that it is easily accessible by staff when required. Items used regularly, such as an emergency trolley with oxygen cylinders, scales and mobile blood pressure (BP) units may be stored locally in equipment bays. Rarely used items may be stored in a central equipment store. A long rectangular room allows the optimum use of space.
Power outlets (4 to 16) should be provided for the recharging of equipment, depending on the equipment list compiled per level of care.
Equipment, particularly larger equipment that has to be floor parked, needs to be defined so that appropriate storage space may be allocated according to the needs of the patients and staff.
Storage – sterile supplies and consumables (sterile and surgical stores)
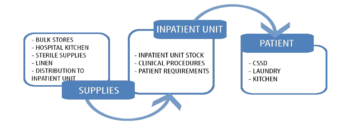
Storage of patients' belongings
The method of storing patients' belongings depends on hospital policy. However, the following considerations must be taken into account:
- Method of storing patients' belongings separately
- System where contaminated clothing can be washed and decontaminated prior to storing in a patient's kitroom
- Labelling method
- Security
- Type of storage, i.e. cupboards per bed unit, store per ward or central store for the whole hospital managed by a dedicated staff member who registers all items handed in
- Size of the facility: many patients coming from rural areas will carry numerous items (e.g.blankets) with them that need to be stored until they are discharged
Waste management
Operational policies for waste management and waste minimisation should be supported, particularly with regard to the following:
- Provision and location of dirty utility rooms so that staff do not have to traverse public and administration areas while transporting contaminated waste items
- Provision and location of recycling bins
- Location of sharps container
Inpatient unit activities
- Clinical diagnostic activities (medical, diagnostic imaging, laboratory, inpatient unit rounds, doctors' visits, going for operations, investigations or rehabilitation)
- Activities of daily living (dressing and undressing, eating, drinking, personal toilet and ablution activities)
- Social activities such as receiving visitors
- Patients might be disabled or might be semi-mobile due to weakness, age, or the disease profile
Table 3: Inpatient unit activities
| Category | Activity | |
|---|---|---|
| A | Patient | Patient Patient may be disabled and wheelchair bound
Patient to dress and undress in vicinity of the bed Patient to take meals in bed or at the bedside Patient to read, watch TV or use a computer Patient to receive treatment and medical care from therapeutic and clinical staff, either lying down or sitting up in bed or in a chair Patient to wash hands |
| B | Nursing care | Teaching
Stripping and making beds Transfer patient from wheelchair or patient trolley manually or by means of a patient-lifting device Patient observation and clinical (doctor’s) rounds Transporting patient to theatre on his or her hospital bed Treatment procedures such as intravenous fluids, traction, etc. Emergency procedures, e.g. patient resuscitation Coordination of patient care, observation, writing up of clinical notes, entering data into computers, making and receiving phone calls and washing hands |
| C | Medical intervention | Diagnostic procedures, such as mobile X-rays and ultrasounds, electrocardiograns (ECGs)
Teaching Treatment procedures such as intravenous fluids, traction, etc. Emergency procedures, e.g. patient resuscitation Examination of patients and washing hands Writing reports and instructions, writing up of clinical notes, entering data into computers Washing hands |
| E | Rehabilitative intervention:
physiotherapists, social workers, occupational and speech therapists, paharmacist and radiographers |
Occupationally specific therapeutic interventions
Patient consulting Diagnostic procedures, such as mobile X-rays and ultrasounds, ECGs, etc Washing hands |
| F | Clerical or administrative | Answering telephones, receiving patients and visitors to the patient unit
Writing reports and collecting and entering data and statistics, ordering food and other consumables Washing hands |
| G | Ancillarystaff (aide, patient assistant) | Assisting patients in wheelchair
Entertaining patients Washing hands |
| H | General staff | Serving food to patients
General tidying work Daily cleaning - sweeping, dusting, washing up Routine cleaning - floors, windows, walls Washing hands |
| I | Maintenance staff | Maintenance- replace globes, fix fittings, reseal floors and repair work to maintain the inpatient unit
Washing hands |
| J | Visitors | Visit patients and socialise in the inpatient unit or day room
Washing hands |
Client expectations
Patient expectations
- Patient privacy and dignity both in the design of the facility and in the treatment of the patient
- Personal safety and security of the patient’s own possessions
- The provision of patient comfort in the facility, e.g. a clean and uncluttered environment, an outside view, low noise levels in the facility, the availability of technical services (staff call system, reading light)
- Adequate availability and visibility of nursing staff
Staff expectations
- A work environment with reduced walking distances, but increased patient observation with minimum staff (optimal care)
- Improved patient risk management, e.g. availability of technical bed-head services, availability of clinical hand basins in patient and staff areas, the availability of automatic bedpan washers, improved environmental control (with reduced infection risk)
- A safe work environment, e.g. suitable height of shelves and service outlets, non-slip floors, view of unit entrance and exit, access control
- Personal safety and security of possessions, e.g. staff lockers, staffroom.
Location and inter-departmental relationships
The design of smaller hospitals may allow the inpatient units to be arranged over the same level. However, inpatient units of larger hospitals may be arranged into multistorey blocks separate from the diagnostic and treatment facilities. This makes it easier to place the inpatient unit block away from noisy areas, ensures patient privacy and safety, and avoids visitors, staff and service traffic through the inpatient units.
Stacking of the inpatient units in multilevel blocks also allows more consistent planning of inpatient accommodation.
The following inter-departmental relationships with the inpatient units are recommended:
- Patient administration and primary circulation should be central to the entrance with the access route to the inpatient facilities off the primary circulation route.
- The obstetric inpatient units should be close to the delivery suite and close to the operating theatre, preferably on the ground floor or with a direct lift access to theatres.
- In district hospitals, operating theatres, HCUs, orthopaedic inpatient units and surgical inpatient units should have a close relationship and preferably be on the same floor.
- Rehabilitation, physiotherapy and occupational therapy should be close to rehabilitation inpatient units and accessible to the outpatients department and the inpatient units.
- Hotel services (cleaning, linen and food services), mortuary services and maintenance units should have a reasonable relationship to the inpatient units. The mortuary, kitchen and laundry should have better access than all other services, especially at night (particularly mortuary services).
- Visitors to the inpatient units should not cross functional access with the services to and from the inpatient units.
Staff overnight facilities
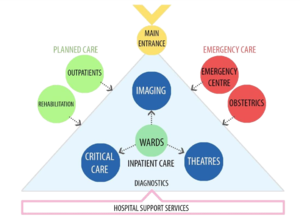
- District hospital
- Surgical inpatients are the inpatients most closely associated with the theatres.
- Regional hospital
- Orthopaedic inpatients are the inpatients most closely associated with the theatres.
- Tertiary hospital
- Subspecialist inpatients, such as neurosurgery and cardiology, are the inpatients most closely associated with the theatres.
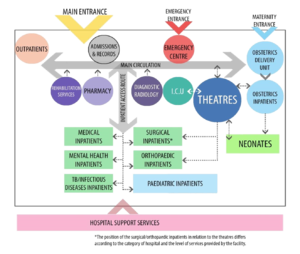
Flow patterns
Point of entry
- Patients or visitors will access the facility through a secure entrance to a parking area or drop-off point from where there should be a clear direction (signage) to the required point of entry.
- Alternatively, a patient will arrive via emergency services to the emergency unit or the maternity services entrance
- Staff members access the facility through a secure staff entrance from a staff parking area or drop-off point.
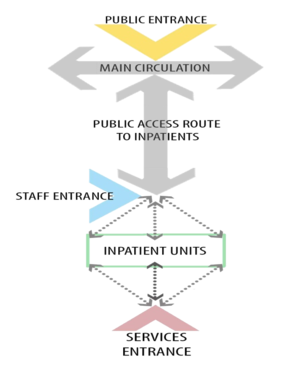
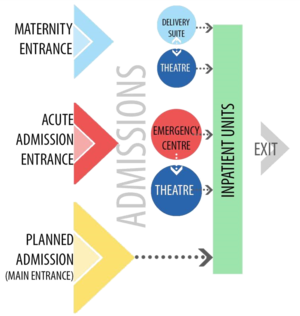
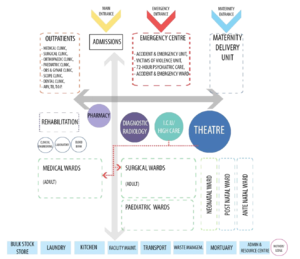
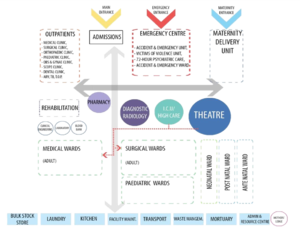
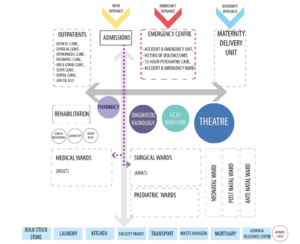
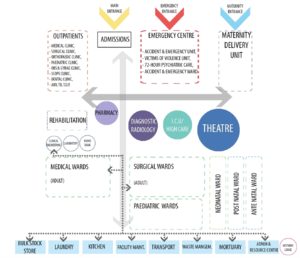
Separation of clean and dirty flow paths in the inpatient unit
Upon arrival arrival at an inpatient unit, a single entry point is preferred in order to control traffic in and out of the inpatient unit. However, infection control principles dictate that clean services should enter at a separate point to where waste and contaminated goods are taken out of the inpatient unit.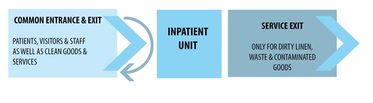
It is important that deliveries to and from the inpatient unit are managed in such a way that they do not clash with visitors arriving and leaving. Goods and services should be delivered at times other than visiting hours.
Functional zones
The inpatient unit functions as a stand-alone unit consisting of six separate functions
Table 4: Inpatient unit functional zones
| Zone | Accommodation spaces |
|---|---|
| Administration spaces | Inpatient unit management, nurses' station and other office spaces as required |
| Public spaces | Entrances, circulation and waiting areas |
| Patient spaces | Patient accommodation and ablution facilities, patient day rooms, disabled showers, treatment room. |
| Service and support areas | Inpatient unit kitchen and storage, clean utility, sluice, stores, cleaners' room, linen, cleaning, medicine store, dirty utility and waste management |
| Staff spaces | Staffroom, locker area, ablutions, overnight accommodation* |
| Teaching spaces | Training or meeting room( in district hospital staffrooms could be used) |
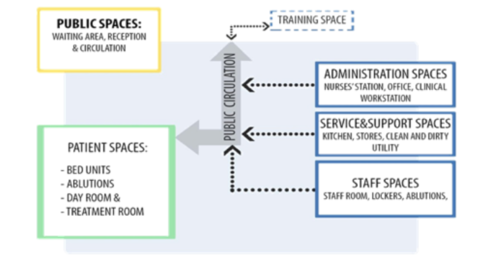
Functional relationships within the inpatient unit
Inpatient unit layouts will vary depending on individual needs per project as outlined in the health and design briefs. However, general principles of design apply and the location of facilities within the inpatient unit should be a logical process optimising the workflow and travel distances for staff from service and storage areas to the patient’s bedside.
The following general principles apply to functional relationships within the inpatient unit:
- The visitors’ waiting room and visitors’ toilet should be outside the entrance to the inpatient unit and may be shared by two inpatient units on the same floor.
- One central entrance to the inpatient unit with access control is preferred.
- The kitchen should be close to the main entrance of the inpatient unit.
- Deliveries and removal of kitchen trolleys should be managed so as not to clash with visiting hours and inpatient unit rounds.
- Nurses’ stations should be positioned centrally with direct visual access to the inpatient unit entrance and in close proximity to the single-bed inpatient units, where the most critical patients would be accommodated.
- The larger bed units for less critical patients could be positioned further away from direct nursing supervision.
- The single-bed units, clean utility, medicine store and treatment room should be positioned near the nurses’ station.
- Areas such as the inpatient unit kitchen and staff areas could be positioned off the main centre of the inpatient unit.
- The clean linen store (or trolley) and sluice room should be close to the bed units to reduce walking distances for the nursing staff.
- Dirty utility rooms should be positioned close to the separate exit door to facilitate collection of the contaminated items and waste, avoiding cross-contamination with clean goods by separating the workflow of clean and dirty paths in the inpatient units.
- Design should minimise the distance between patient bed units, staff workstations and support rooms to facilitate the efficient delivery of patient care and optimal staff utilisation.
- Each bed unit will be serviced by staff and support facilities, therefore access to supplies and means of disposal is essential. One of the primary goals is to minimise the distance between patient units and workstations and support rooms. The inpatient unit should be planned to provide a public/clinical and a utility/service division.
- The unit manager’s office should be positioned for maximum supervision of both clinical and household functions (close to the entrance).
- The clinical administration area and doctor’s office should be near the nurses’ station with access to the clinical spaces.
- The sluice, linen, and storerooms should be positioned central to the patient bed units to reduce walking distances for the nursing and cleaning staff.
No one particular inpatient unit layout has been found to be universally superior. In all cases, the final decision must be a response to the physical constraints of the site, local service needs, and operational policies.
Ablution facilities
Patient ablution facilities should be en suite directly accessible from the adjacent bed unit. Ablution facilities for clinical staff may be provided in association, but not combined with staffroom areas. Designated toilets for clinical staff should be provided.
Key room relationships
It is important that key room relationships are maintained such as illustrated in figure 18.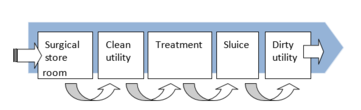
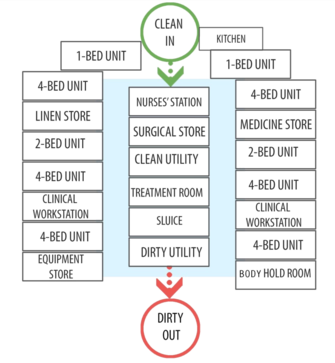
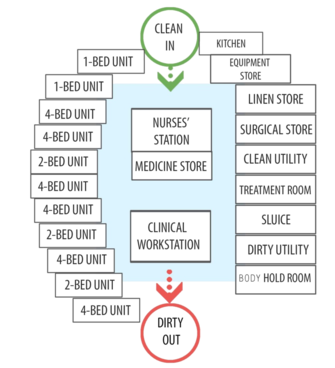
List of rooms
The majority of rooms in ward are standard rooms that may be found in other departments in the health facility. These rooms have been detailed separately in the IUSS: GNS generic room requirement sheets. These sheets must be referred to when planning the rooms.
Table 5 lists the rooms found in the inpatient unit and indicates the rooms that are standard and those that are non-standard. The non-standard rooms that are described in more detail under 'room requirements'. The standard rooms are described in less detail as they are detailed in the IUSS: GNS generic room requirement sheets.
Table 5: Loss of rooms: Standard and non-standard
| Room | Standard | Non-standard |
|---|---|---|
| Patient areas | ||
| Bed unit - Standard patient area: | ||
| Single-bed unit | x | |
| Two-bed unit | x | |
| Four-bed unit | x | |
| Patient day room(provided in a district hospital) may be shared between wards | x | |
| Patient ablutions: | ||
| En suite facility with shower, toilet and hand basin (all should be disability friendly) | x | |
| Assisted bath where required | x | |
| Assisted shower | x | |
| Staff areas | ||
| Office - manager | x | |
| Office - Counselling or doctor (optional) | x | |
| Nurses' station | x | |
| Clinical admin area | x | |
| Office - administration | x | |
| Staffroom | x | |
| Staff lockers can be provided in a passage off the main passage leading to the restroom | x | |
| Toilet - staff (male and female) | x | |
| Service support areas | ||
| Bay - mobile equipment | x | |
| Bay - Resuscitation trolley | x | |
| Clean utility ( setting out the sterile packs and treatments) | x | |
| Cleaners ' station | x | |
| Dirty utility (refuse and dirty linen) | x | |
| IT room - consult with information and communication technology (ICT) planners depending on the hospital | x | |
| Sluice room | x | |
| Store - Clean linen | x | |
| Store - Equipment | x | |
| Store - Kit (patients' clothes and belongings could be in a central area or per inpatient unit - refer to brief) | x | |
| Store - Medicine | x | |
| Store - Consumables (surgical and medical) | x | |
| Treatment room | x | |
| Inpatient kitchen | x | |
| Body-holding room | x | |
| Public areas | ||
| Inpatient unit corridor | x | |
| Entrance | x | |
| Visitors' waiting area | x | |
Room requirements
Bed unit – standard patient area
These guidelines allow space in all bed units for equipment and the activities around each bed and between beds.
Location and relationship

Staff capacity
Space is required to adequately accommodate the activities taking place at the patient's bedside and the movement by staff around the bed, which can involve several staff at any one time and may also include the use of equipment at the patient's bedside.
These activities can involve the following:
- Doing clinical observations taking blood, blood pressure and the patient’s temperature
- Assisting with activities of daily living: dressing, feeding and washing
- Treatment procedures, such as intravenous fluids, traction, etc.
- Examining the patient
- Stripping and making beds
- Transferring the patient from a wheelchair or patient trolley manually or by means of a patient-lifting device (patient may arrive in a wheelchair or on a patient trolley)
- Patient observation and clinical (doctor’s) rounds
- Diagnostic procedures, such as X-rays, ultrasounds, ECGs, etc.
- Transporting the patient to the theatre on his or her hospital bed
- Emergency procedures, e.g. patient resuscitation
- Recording of notes at the bedside either manually or on the computer (clinical staff)
- Cleaning and dusting around the bed (clinical staff)
- Maintenance work (maintenance staff)
Patient activity
- May sit next to the bed
- Receives treatment from therapeutic and clinical staff while lying down or sitting in bed
- Receives visitors
General requirements
The following is required in the bed unit space:
- Space should be provided for a bed and bedside locker next to each bed, preferably on the right.
- Temperature in bed units should be between 20 ˚C to 23 ˚C.
- Positive air pressure should be maintained in bed units.
- Bed curtain rails and curtains should be provided for privacy around each bed.
- Each bed unit should have a disability-friendly en suite shower, toilet and hand basin with a call button for the nurse.
- A clinical hand basin with elbow taps, goose neck and an outlet must be provided in the bed unit. The basin and backsplash should be a moulded unit. A wall-mounted mirror, soap dispenser and paper towel dispenser should be provided with each hand basin.
- Waste bins should be next to but lower than the hand basin. There should be one for medical waste, one for sharps (refer to brief document) and one for general waste.
- There should be adequate lighting provision (natural and artificial light) – daylight is important in the bed unit.
- The patient should have visual privacy without compromising staff control and observation of the patient.
- A standard equipment list per level of care (district, regional or tertiary) should be made available. The list will distinguish between loose equipment to be provided by the client and fixed (mounted) equipment to be provided and installed by the contractor.
Space requirements
Ergonomic studies have established that most activities carried out at the bedside can be accommodated within the dimensions 3 450 mm (width) × 4 100 mm (depth). This represents the clear bed space and does not include space for fixed storage.
One bed unit equals a minimum of two and maximum of four beds per 32-bed inpatient unit in a district or regional hospital. The clinical brief will outline the tertiary hospital requirements.
It is preferable for beds on opposite sides of the room to be offset to provide greater privacy.
Single-bed unit approximately 15 m² minimumFour-bed unit approximately 44 m² (majority of rooms) minimum
Six-bed unit approximately 65 m² minimum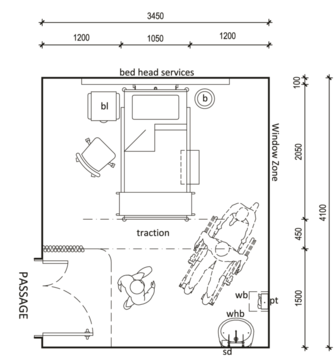
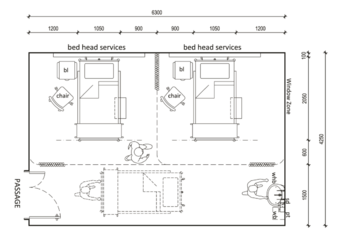
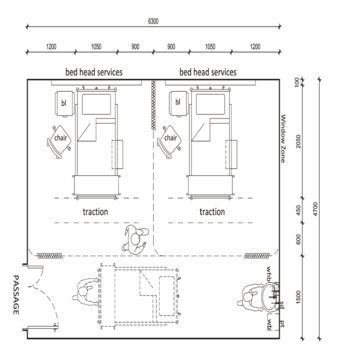
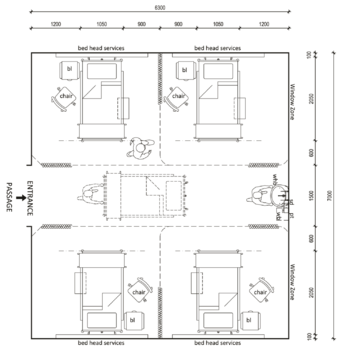
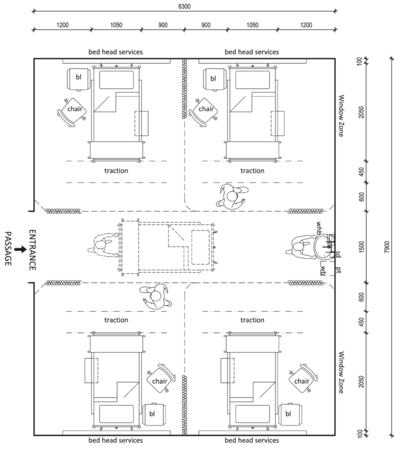
Bed services
Services should be provided in wall bed-head units behind and above the bed.
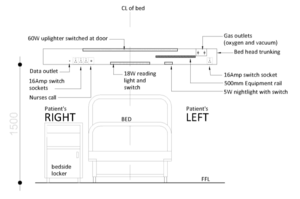
Table 6: Bed-head services per level of care
| BED HEAD SERVICE | |||
|---|---|---|---|
| Service | District hospital | Regional hospital | Tertiary hospital |
| Oxygen | One shared between two beds | One per head | One per head |
| Medical air*
(low pressure) |
One shared between two beds | One per head | One per head |
| Vacuum | One shared between two beds | One per head | One per head |
| Power outlets
(15Amp) |
Four per bed:
One to patient's right side for patient use Three to patient's left side for medical equipment purposes |
Six per bed:
Two to patient's right side for patient's use Four to patient's left side for medical equipment purposes |
Six per bed:
|
| Equipment rail | One per head | One per head | One per head |
| Nurse call | One per head | One per head | One per head |
| Reading light | One per head | One per head | One per head |
(Refer to IUSS: GNS Building Engineering Services)
En suite sanitary facilities
Description and function
An en suite bathroom provides facilities for patients to wash, shave, groom, shower and use the toilet, either independently or with assistance. The layout and area must accommodate an assisting nurse, patient lifter or wheelchair. The minimum area for this room is 6 m².
Location and relationships
The en suite bathroom must be adjacent to the bed unit or directly accessible from each unit with the following services, preferably on an external wall:
- Clinical hand basin with a mirror above it, soap dispenser and paper towel dispenser
- Toilet
- Nurse call button connected to the nurses’ station
- An adjustable overhead hand shower head with flexible hose
General requirements
Doors must open outwards from the en suite bathroom and must be fitted with an emergency release function.
The shower must have a shower curtain
The seat must fold up in the shower area and there should be a bench outside the shower (but within the en suite bathroom) for personal belongings. Three durable clothes hooks are to be mounted on the wall above this bench.
Fittings must be mounted in such a way that the water temperature can be adjusted without the patient or nurse getting wet.
The exit door must be fitted with escape hardware to allow staff access in the case of an emergency.
Nurse call and emergency call buttons and indicators should be provided that are tamperproof.
Epoxy grout is to be applied in all tiled areas.
Fittings, including grab rails, are to be installed to the toilet and shower area, including towel rails.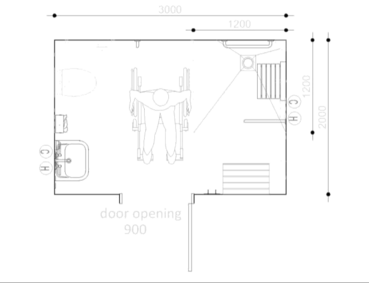
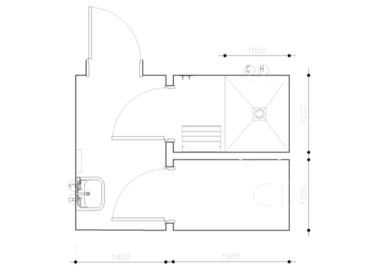
Assisted shower
Description and function
An assisted shower room with an enclosed shower cubicle, fitted with a door, to the height of a wheelchair or commode and a central floor drain is required. The shower head should be a hand-held device and the temperature of the water should be controlled. The size of the room should provide a minimum of 6.5 m² to provide space for the staff who will assist the patient.
Location and relationships
The shower should be located immediately adjacent to or should be directly accessible from the passage of the inpatient unit. It should preferably be central to the bed units.
Services
The following should be provided:
- A hand basin with tiles above it, a mirror, soap dispenser and paper towel dispenser
- A nurse call button connected to nurses' station
- A hand-held shower head that can be removed from above with a flexible cord
Activities
There should be sufficient space for two people in the shower area to assist the patient to wash and shower.
General requirements
The following should be provided:
- A waist-height shower enclosure with a hand-held shower head
- An enclosed seat that can fold up
- Taps of which to the water temperature can be adjusted without the staff assisting the patient getting wet
- A door that is fitted with the escape hardware to allow staff access in the case of an emergency
- Nurse call and emergency call buttons and indicators
- Fittings, including grab rails and towel rails, that can accommodate non-ambukant patients
- A hoist for lifting a patient
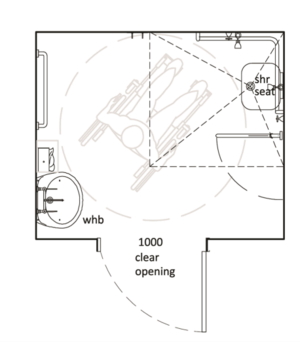

Counselling room
Description and function
The counselling room provides a private area for staff to consult with patients and their family
Services
The following should be provided:
- A double-plug outlet
General requirements
The following should be provided:
- The room must create a tranquil, calm atmosphere. The use of color must be subtle - preferebly using pastel colours
- A window with an outside view from this room is advisable
- This room may be shared by two inpatient units
Furniture
The following should be provided:
A table and four chairs
Lounger and comfortable lounge chairs with a side table
Day room
Description and function
The day room provides space for the patient to socialise with other patients and visitors. The room should be a minimum of 12m². This is more applicable in rural district facilities.
Location and relationships
The day room should comply with the following:
- Have an external wall to take advantage of natural light and outlook
- Be located away from bed units, but within close proximity to the nurses’ station to enable staff supervision and observation
- Have direct access off the main inpatient unit passage
Activities
The following should be provided:
- Patients should be able to sit down and may play games, as well as socialise
- Patients should be able to receive visitors
Services
The following should be provided:
- Two double-plug outlets
General requirements
The following should be provided:
- Low windowsill heights should promote views from a seated position.
- Day rooms to be located inside the inpatient unit without outside access, or it may have outside access (to the garden or a balcony). This depends on the inpatient unit type and the need for security.
Equipment
(Refer to the equipment list.)
In addition, the following should be provided:
- Table and stackable chairs (to allow space for wheelchair users)
- Water cooler
- Waste paper bin
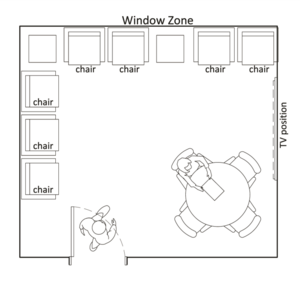
Treatment room
Description and function
The treatment room provides a controlled environment, privacy and facilities for carrying out consultations, examinations and the treatment of patients. It should have a minimum size of 15 m².
Location and relationships
The treatment room should be located with other patient care areas, near the clean utility with direct access to the inpatient unit passage.
Activities
The following should be provided:
- Four clinical staff members attending the patient at any given time
- Access to patients from both sides of the couch
- As the patient may be ambulant, in a wheelchair, on a trolley or in a bed, patient transfer may be required to the examination couch
- Private examination and discussion with the patient
- Specimen collection (e.g. bone marrow)
- Wound treatment (applying or renewing dressings)
- Other examinations and treatment activities specific to the medical discipline
- Treatment by a physiotherapist or occupational therapist
- Completing special examination requests and writing reports
Services
The following should be provided:
- A hand basin with elbow taps and a gooseneck outlet with tiles above it, a mirror, soap dispenser and paper towel dispenser
- Four electrical points
- A vacuum
- Data and telephone terminals
- A stainless steel sink
- A good-quality examination light, preferably mounted on the ceiling
- Bed-head service with two power outlets on the right of the patient examination couch and three power outlets on the left, oxygen and vacuum outlets, and an equipment rail for mounting items such as a suction unit, oxygen flow meter and nurse call button
- A wall-mounted X-ray viewing panel where applicable
General requirements
The following should be provided:
- Lockable doors
- A door that is wide enough for a bed to pass through
- Curtains for patient privacy
- A stainless steel worktop with a cupboard underneath it for stock (± 1.0 m)
- Positive pressure
- Temperature in the treatment room maintained at between 20 °C and 23 °C
Equipment
The following should be provided:
- An examination couch
- A double-step foot stool
- A mobile drip stand
- A wall-mounted diagnostic set
- A mobile vital signs monitor (nibp+hr+sao2);
- An emergency oxygen cylinder on a mobile stand
- An ECG machine on a mobile trolley
- A fitted desk unit with a chair
- A pedal bin or kickabout with a bucket

Inpatient support requirements
The following inpatient unit support spaces are listed in alphabetical order
Body room
Description and function
This room is specifically for holding a deceased patient until the body is collected by the mortuary
- Size 3.5 m x 3.4 m
Location and relationships
This should be located far away from the patients and public areas, and placed close to the service exit or service lift
Activities
Provision should be made for the following:
- Holding of the deceased patient until collection by the mortuary
- Preparation of the patient by nursing staff in anticipation of the family coming to view the patient
- Viewing of the patient by the family
Services
The following should be provided:
- Clinical hand basin with elbow taps with gooseneck outlet and tiles above it, with soap dispenser and paper towel dispenser
- Cupboards for storing equipment
Considerations
The following need to be taken into consideration
- A quiet area with subdued lighting
- Décor to create a calm atmosphere
- Pastel, gentle colours to be used on walls and in curtains and blinds
- The room may be shared by two wards
Equipment
The following should be provided:
The patient is usually wheeled in his or her hospital bed, where he or she remains until he or she is collected by the mortuary, when the body is placed on a trolley before leaving
Clean utility
Description and function
The clean utility is for the storage and preparation of clean and sterile materials and equipment for patient treatment, as well as the secure storage and preparation of medications, including intravenous fluids. A minimum space of 9 m² is required.
Location and relationships
The clean utility should have direct access from the passage of the inpatient unit, with close proximity to the nurses’ station and the treatment room.
Activities
The following should be provided:
- One to two persons at any given time
- Storage of sterile packs from the CSSD
- Storage of liquids from the pharmacy
- Hand washing by staff prior to trolley preparation for bedside treatment or procedures
- Preparation of trolleys for treatment or procedures in the procedure room
- Warming of solutions required during treatments or procedures
Services
The following should be provided:
- A stainless steel clinical, drop-in hand basin with elbow taps and gooseneck outlet
- One double 15 Amp plug above counter height
- Standard power outlet for liquid warmer: stand-alone or standing on the worktop
General requirements
The following should be provided:
- Lockable doors to the facility
- Lockable cupboard with shelving for sterile packs and storage of vacolitre
- Stainless steel worktop: space for one 600 x 450 mm instrument trolley and two 450 x 450 mm instrument trolleys underneath the worktop
Equipment
The following should be provided:
- Pedal bin
- Liquid warmer: stand-alone or standing on the worktop
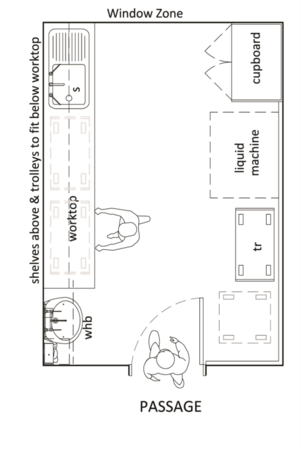
Cleaner's room
Description and function
The cleaning service may be in-house or outsourced, but space should be provided for a cleaner's room.
The cleaning station provides a base for the cleaning staff to store and decant cleaning equipment, materials and cleaning agents, and a cleaner's trolley. A space requirement of 8 m² should be provided. A ratio of 0.8 m² per patient may be used to calculate the area.
The room should be separate from the dirty utility room and the waste disposal room.
Location and relationships
The cleaning station should be close to the exit of the inpatient unit with direct access to the inpatient unit passage
Activities
Provision should be made for the following:
- Usually one housekeeper or cleaner will utilise the area
- Hand-washing by staff before leaving the room
- Report writing
- Water collecting and emptying cleaning buckets
- Hanging wet mops and cloths to dry
Services
The following should be provided:
- A stainless steel hand basin with elbow taps and a gooseneck outlet, and tiles above it with a mirror, soap dispenser and paper towel dispenser
- A drip sink with a hinged bucket grid for cleaning mops (not a slop-hopper)
General requirements
The following should be provided:
- Small worktop on which to write
- Hooks on which to hang tops
- A lockable cupboard with shelves for cleaning materials, disinfectants, disposable gloves, soap, cleaning detergents, new mops and brooms, cleaning cloths, paper towels, toilet paper, etc.
- A mop rack
Equipment
The following should be provided:
- Mops
- A cleaning trolley
- A polisher
- Buckets

DRAWING 13: CLEANING STATION AND CLEANERS TROLLEY
Clinical workstation
Description and function
This is a work area separate to the nurses’ station. The clinical workstation area is required for clinical staff to make file notes, do patient administration, discuss cases and do research. For planning purposes, a 28- to 32-bed inpatient unit will require a work space for four staff members at a time.
Location and relationships
The space should be positioned close to the nurses’ station, with privacy from inpatient unit activities.
Activities
Provision should be made for the following:
- Making and receiving phone calls
- Writing reports
- Accessing and printing data from a computer
- Recording patient information in patient files and filing printed reports
- Digital radiology screens
- Case discussion and peer support
Services
Provision should be made for the following:
- Two telephones
- Three data points
- An X-ray viewing panel if required
- Power outlets for two computers, a fax machine and a printer
- Power outlet for a digital X-ray monitor and keyboard
General requirements
Provision should be made for the following:
- A suitable workspace for the clinical staff and doctors to do clinical administration at the station with space for computers, telephones, printing and administrative work
- A work surface and space for filing, shelves to accommodate files and stationery with drawers and cupboards
- All surfaces must be impervious and designed for easy cleaning
- Wall-mounted wipeboard and pinboard
Equipment
- Two telephones
- Three data-connected computers and digital X-ray equipment
- Printer
- X-ray viewing
- Power outlets for two computer points and two central monitors
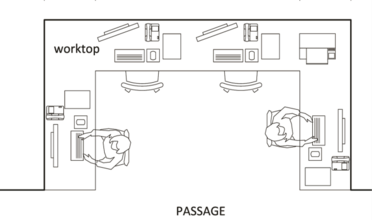
Dirty utility
Description and function
The dirty utility room is the waste disposal room providing for the temporary storage of contaminated waste, sharps, soiled linen and recyclables prior to removal. A minimum area of 8 m² is required.
Location and relationships
The dirty utility room must be located at the exit to the inpatient unit to allow for ready access from the service exit. It should preferably be adjacent to the sluice. The dirty utility room should have easy access to hand-washing facilities and must have direct access to the passage of the inpatient unit.
Activities
Provision should be made for the following:
- Temporary storage of sluiced and dirty linen
- Temporary storage of waste bins
- Temporary storage and collection of canvas bags filled with dirty linen(± four bags a day per inpatient unit)
- Collection of refuse
Services
The following should be provided:
- A hand basin with elbow taps and a gooseneck outlet with tiles above it, soap dispenser and paper towel dispenser
General requirements
The following should be provided:
- Space for dirty linen trolley, as well as sluiced trolley
- Storage space for sharps, medical waste and domestic waste
- Bumper rails to prevent bins from marking walls
- Space for four large medical waste boxes (these may be stackable)
- A bumper rail to protect the behind the trolleys
- Good ventilation
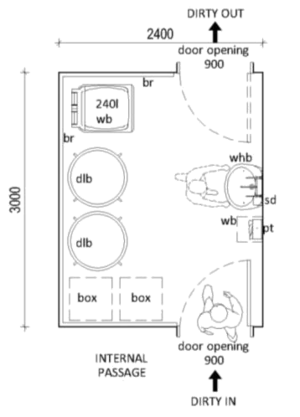
Inpatient unit kitchen
Description and function
The kitchen is used for preparing and heating refreshments, snacks for patients, washing cups, and storing food supplements and snacks. The ward refreshment and food trolley is parked in the kitchen. A minimum area of 8 m² is required, increasing by 1.5 m² for every 10 beds (12 m² per 32 bed inpatient unit)
Location and relationships
The kitchen should have easy access to patient areas and the passage of the main inpatient unit
Activities
Provision should be made for the following:
- Two people at any given time
- The preparation of hot or cold beverages for patients
- Heat refreshments, snacks and some meals
- In some rural, washing utensils and storing them in the inpatient unit kitchen
Services
Provision should be made for the following:
- A double-bowl sink with drainage and hot and cold water
- A microwave oven
- Four power outlets for the hot-water supply unit, 120 ℓ fridge/freezer combination and microwave, plus one extra point
- Continuous hot-water supply (hydro boil) unit placed over the sink drainage
- A stainless steel hand basin with a paper towel holder and soap dispenser
- A double-bowl sink with drip trays
- Cupboards for keeping detergents, cups, saucers and glasses
General requirements
Provision should be made for the following:
It may be in-house or outsourced
Suitable workspace and floor covering is needed that is easy to maintain
Equipment
Provision should be made for the following:
- Continuous hot-water supply unit
- 120 ℓ fridge/freezer combination
- Microwave oven
- Tea trolley
- Food trolley (from main kitchen)
- Bump rail for food and tea trolley
- Refuse bin(e.g pedal bin)

IT room (size dependent on the clinical brief and hospital)
Description and function
Switch room to house computer services, which are connected to the main server.
Location and relationships
Adjacent to the inpatient unit and may be shared by other facilities on the same floor level.
Services
Provision should be made for the following:
- Data cabling to specialist approval and design
- Power points to be specified by the IT specialist
- Access control may be required
General requirements
Provision should be made for the following:
- Size depends on the number of facilities connected to the equipment contained in the room. A minimum of 2m x 2m is recommended
- The planning of this room must be coordinated with the IT consultants and the clinical staff.
Nurses’ station
Description and function
The nurses’ station is the administrative base and communication centre for the inpatient unit and the enquiry point for patients and visitors. It provides a focal point to which all staff, whose time is mostly spent with patients, can return to record data, issue and receive information and receive verbal and written instructions. It provides for the coordination of patient care, observation, writing up of clinical notes, entering data into computers, and making and receiving phone calls. The station must accommodate nurses, an inpatient unit clerk, and, at times, doctors.
The area controls the movement of patients, staff and visitors entering and leaving the unit and can receive mail, flowers and a variety of other items that may be delivered to the unit. The inpatient unit clerk or receptionist is generally located in this area with ready access to files and stationery. One nurses’ station in an inpatient unit, central to the bed units, will allow for the observation of the main patient areas and, where possible, people entering and exiting the inpatient unit
For planning purposes, a 28- to 32-bed inpatient unit will require a nurses’ station of 14 to 18 m².
Location and relationships
Decentralised nurses’ stations may be considered for immediate work associated with patient care: the review of patient notes, files and tests (short work). This is facilitated by the use of electronic record systems and point-of-care management. The floor area of the nurses’ station will vary according to the activities and services required.
Activities
Provision should be made for the following:
- Management of the clinical service requirements
- Access to the electronic patient system
- Making and receiving phone calls
- Writing reports
- Updating the patient bed allocation board
- Accessing and printing data from a computer
- Recording patient information in the patient’s file and filing printed reports
- Controlling the nurses’ call system
- Monitoring service alarms (e.g. fire alarm system)
- Managing the key cupboard
- Managing digital radiology information
- Providing a contact point for doctors and nurses
Services
Provision should be made for the following:
- Two telephones
- Two data points
- Six power outlets (for two computers and screens, a fax machine and printer)
- Hands-free clinical hand basin, elbow taps, a mirror, paper towel holder, soap dispenser and wall-mounted waste paper bin
- Nurse call system connected to a display panel at the nurses’ workstation or mounted on the wall directly behind the nurses’ station
- Fire alarm/smoke detection panel mounted on the wall directly behind the nurses’ station
- Alarm panel for gas and water mounted on the wall directly behind the nurses’ station
- Power outlet for digital X-ray monitor and keyboard
- Access control (inpatient unit entrance and exit plus dirty utility outside door)
- Emergency power and uninterrupted power supply (UPS)
- Access control panels at the inpatient unit’s entrance and exit, including the outside door of the dirty utility
- Medical gas shut-off valves in visual control and within easy reach of the nursing staff
General requirements
Provision should be made for the following:
- Positive air pressure to allow for fresh air and reduce the risk of airborne diseases
- Large workstation with a view of the entrance, and optimal observation of the most acute patients
- Suitable workspace for the inpatient unit clerk (should no separate office be provided) and the nurses to work at the station with space for two computers, two telephones and a printer
- Work surface and space for filing, shelves to accommodate files and stationery with drawers and cupboards, i.e. 20 lever-arch files (for policy documents, etc.) in a cabinet, ten lever-arch files in cupboards below the work station, plus space for 30 different types of forms (all A4) in pigeon holes above the work station
- All surfaces must be impervious and designed for easy cleaning
- Access to pneumatic system for laboratory samples (regional hospitals –dependent on the hospital size; tertiary hospitals as standard)
- Air conditioning : ± 22 °C
- Space for a dictionary and reference books
- A key cupboard mounted on the wall behind the nurses’ station
- Space to store and recharge haemoglobin and glucose meters
- Space to store and recharge diagnostic sets
- Space for the patient allocation board
- Space for an adult scale with length meter
- Space for an emergency trolley
- Space for an oxygen cylinder on a mobile stand
- Space for three observation trolleys or mobile non-invasive blood pressure (NIBP) machines
- Wall-mounted wipe board and pin-board
Fittings
Provision should be made for the following:
- Counter,with sitting space for at least four people
- Above- and under-worktop storage space for policy manuals, registers and report documentation
- Access to medical gas shut-off valves must be in visual control and within easy reach of the nursing staff
- Space for two telephones, two computers and a printer, the nurse call panel, fire alarm and smoke detection panel, and medical gas and vacuum supply.
Equipment
Provision should be made for the following:
- Patient admission board (whiteboard marked into bed units, the beds in each unit, the patient's name, the doctor's name and comments)
- Key cupboard
- Wall clock
- Pin-board
- Whiteboard (small - stock ordering notes, for instance)
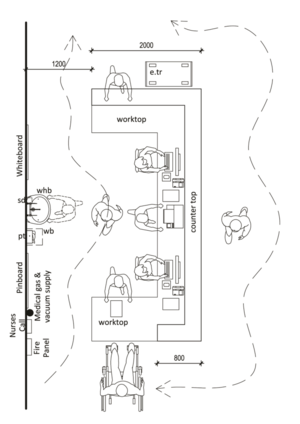
Patient kitroom
Description and function
The provision of a kitroom could require a central or unit kitroom. The recommended minimum unit size of 6 to 8 m² is suggested. The room is used for the safe storage of patients’ clothes and belongings, excluding valuables and money.
Location and relationships
Activities
Provision should be made for the following:
- Clear plastic bags tagged with patient identification
- Bags to be locked away in mesh wire baskets
- Clearly marked plastic bags to be received with patient's belongings
- Receipt to be provided to the staff member
General requirements
Provision should be made for the following:
- The store should be lockable
- Slated shelving is required
- Mesh wire cupboard
- Good ventilation
Sluice
Description and function
The sluice makes provision for the following:
- Decontamination and storage of patient utensils such as bed pans, urinals and bowls
- Cleaning and holding used medical instruments for collection ans sterilisation at CSSD
- Testing and disposing of patient specimens
A minimum area of 10 m²is required.
Location and relationships
The sluice must be located centrally to the bed units to allow for ready access from the patient areas.The sluice room must have direct access to the inpatient unit passage and close proximity to the dirty utility
Activities
Provision should be made for the following:
- Sluicing, cleaning, disinfecting and storing bed pans, urinals, sputum mugs and wash basins
- Urine testing and temporary storage of laboratory samples
- Washing and temporary storage of medical instruments
- Safe usage, service and maintenance of automatic bedpan washer
- Hand washing by staff upon entering and before leaving the room
Services
Provision should be made for the following:
- A stainless steel clinical hand basin with elbow taps and a gooseneck outlet with tiles above it, soap dispenser and paper towel dispenser
- A double deep-bowl stainless steel sluice sink unit with elbow taps and a gooseneck outlet, as well as a hand-held shower on a flexible hose
- An automatic bedpan washer and power outlet at 1100 AFFL (ensure that the choice of the type of bed pan washer is made early in the design phase to enable adequate provision for drainage)
- A single stainless steel sink with workspace for washing medical instruments
- An extraction air diffuser
General requirements
Provision should be made for the following:
- A stainless steel work surface next to the sluice for urine testing
- A wall-mounted rack for clean bedpans and urinals
- Cupboards fir storage of sputum mugs, detergent for the automatic bedpan washer, urine testing sticks and equipment
- Shelves for wash basins and buckets
- Good ventilation
- Bumper rail to protect the wall behind the trolleys
- Clinical hand basin adjacent to the entry door
- Clean medical waste box storage needs to be considered in relation to the sluice
Equipment
Provision should be made for the following:
- Bed pans and urinals
- Urine bottles
- Wash bowls

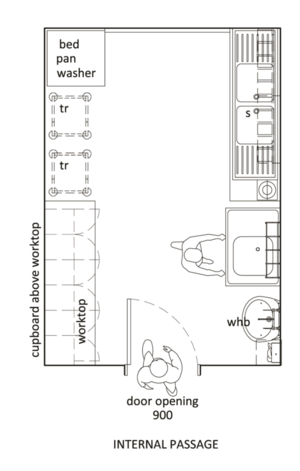
Store for clean linen
Description and function
Provision should be made for the storage of clean linen, blankets and hospital-issued patient attire or patient theatre attire. A minimum size of 8 m² is required. Allocate a minimum of 0.16 m² of linen per patient and make allowance for storing and packing the linen trolley in the room.
Storerooms are best designed in the elongated rectangular shape to allow easy access to all items .
Location and relationships
Provision should be made for the following:
- Located within view of the nurses's station
- Easily accessible to all patient areas
- Directly off the main inpatient unit passage
Activities
Provision should be made for the following:
- One to two people at any given time
- Counting linen
- Unpacking received linen (mostly in canvas bags)
- Loading clean linen onto the linen trolley
General requirements
Provision should be made for the following:
- Lockable door (undercut door for ventilation)
- Perforated or slated shelving Need to make provision for supplies over weekends and private holidays in rural areas
Equipment
Provision should be made for the following:
- A clean linen trolley
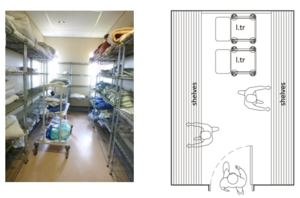

Store for consumables
Description and function
Safe storage should be provided for the storage of clinical consumable items, like intravenous fluids and sets, syringes, needles, bandages, etc. Provision should be made for a minimum size of 9 m² per 28- to 32-bed inpatient unit. Allow 0.183 m² stock area per patient.
Location and relationships
The consumables store should be centrally located close to the clean utility and have direct access to the inpatient unit.
Activities
Provision should be made for the following:
- Two people at any given time
- Storage of consumable items on wall-mounted shelves
- Allow enough space for the transfer of items from a trolley onto the shelves
General requirements
Provision should be made for the following:
- The store should be lockable
- Slated shelving is required
- Sturdy wall-mounted shelving
- The ability to identify and 'partition' stock (risk management)
- Sturdy wooden and moulded plastic pallets on the floor( ±120 mm high) for the storage of intravenous fluids - only stack three boxes high
- Ensure controlled temperature - a maximum of 26 °C
- No items to be stored on the floor
Equipment
Provision should be made for the following:
- Intravenous fluids, sets, syringes, needles, bandages, etc.

Equipment store
Description and function
The equipment store is used for the safe storage of medical equipment, traction accessories, the parking of mobile IV poles, wheelchairs, lifting poles, bed cradles and commode chairs. Plugs and shelves are available for recharging and storing electrical equipment. A minimum size of 12 to 20 m² is recommended. This will vary in larger hospitals with 400 or more beds.
Location and relationships
Activities
Provision should be made for the following:
- One or two people at an one time
- Moving equipment in and out of the store
- Placing equipment on shelves and plugging in to power
Services
Provision should be made for the following:
- Ten power outlets (depending on the facility) above the worktop to recharge equipment batteries
General requirements
Provision should be made for the following:
- The store should be lockable
- A counter top to recharge small equipment
- Shelving to store traction units and small equipment
- An open wall area where equipment mounted on trolley can be stored
- A minimum 2.5 m internal width is suggested
- Double door access
Equipment
Equipment will vary according to the level of care. This will also serve as a guideline for the number of power outlets, as well as thee floor and workspace that is required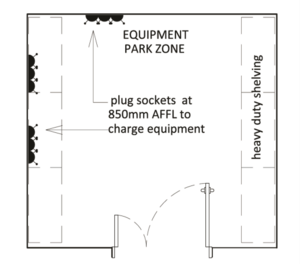
Medicine store
Description and function
The purpose of the medicine store is the safe storage of scheduled medication.
Location and relationships
It should be in full view of the nurses' station, preferably directly behind the nurses' station.
Activities
Provision should be made for the following:
- Two people at any given time
- Placing and removing medicine on shelves, in refrigerators and in-wall mounted drug cupboards
- Storing and loading the medicine trolley used during the inpatient unit round
- Counting drugs
Services
Provision should be made for the following:
- Clinical hand basin with elbow taps and gooseneck outlet with tiles above it, soap dispenser and paper towel dispenser
- Access control recording everyone going in and out the room
- Power outlet for the refrigerator
General requirements
Provision should be made for the following:
- Safe storage of medicine on shelves, in refrigerators and in wall-mounted drug cupboards
- Shelving
- Storage space for the medicine trolley used during the inpatient unit rounds
Equipment
Provision should be made for the following:
- Wall-mounted drug cupboard
- Medicine trolley
- Refrigerator with a thermometer and power outlet


Staff facilities
Staffroom
Description and function
The staffroom is used by the staff for respite and relaxation during tea and meal breaks, especially where it is difficult for staff to use centrally located facilities at night. It may also be used for staff meetings and tutorials. It has facilities for preparing and/or heating refreshments, snacks and meals, washing utensils and disposing of food waste.
A minimum area of 15 m² is required. Size depends on the number of staff members using the facility and the usage of the facility. Allow 1.5 m² per person, assuming that a maximum of 40% of the inpatient unit staff will utilise the room at any one time.
Location and relationships
The staffroom must be located away from the patient, treatment and visitor areas.
Staff toilets should not be en suite to staffrooms, but should be located close to the staff restroom. The staff restroom could be shared between two inpatient units, or one space could be provided per floor.
Activities
Provision should be made for the following:
- Four people at a time
- Resting or seated
- Reading and writing
- Eating meals
- Holding meetings
Services
Provision should be made for the following:
- Stainless steel double-bowl sink with drainage and hot and cold water
- Hydro boil positioned over the drainage sink
- Four power points for appliances
General requirements
Provision should be made for the following:
- Facilities for food warming and beverage preparation and storage should be provided
- Wall-mounted cupboard to store cups, glasses and consumables (tea, coffee,milk, etc.)
- Undercounter cupboard to store cutlery and cleaning materials
- Staff toilet should be next to, but not directly off the staffroom
- A relaxed ambiance is essential
Equipment
Provision should be made for the following:
- Easy chairs
- Table with chairs
- Shelving for books and magazines
- Whiteboard for daily notices (size: 1 m x 1.5 m)
- Pinboard
- Microwave oven - stainless steel, 40 ℓ, 1000 watts
- 120 ℓ fridge/ freezer combination
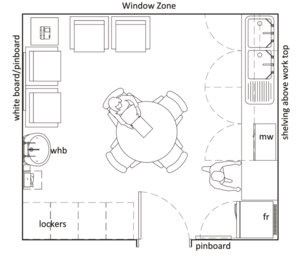
Staff locker area
Description and function
Lockers are to be provided for staff to store their personal possessions.
Location and relationships
Lockers should be positioned in a passage leading to the staffroom, in the staff room or opposite the nurses' station. This is to ensure that anyone tempering with lockers can be seen immediately.
General requirements
Provision should be made for the following:
- Secure storage of personal property
- Locker sixe: 450 wide x 600 deep x 900 high with a bar to hang items on or 450 wide x 600 deep x 450 high, depending on requirements

Staff toilet
Description and function
This is a room containing a toilet and hand basin for staff use. A minimum of 3 m² is recommended. (No urinals should be installed.)
Location and relationships
General requirements
Provision should be made for the following:
- Wall-fixed toilet for cleaning underneath
- Bathroom accessories
- Mirrors - height and size is important for those using the facility
- Soap dispensers and hand towel dispensers
- Toilet roll holders in all toilets
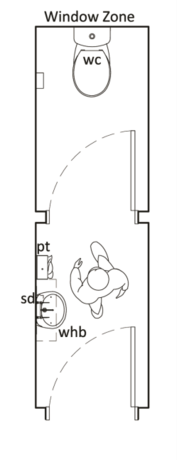
Clinical overnight sleeping facilities
Description
Sleeping, rest and ablution facilities are provided for clinical staff working at night who are not required to be permanently on the inpatient unit but must be ‘on call’ should they be required.
Location
These are located close to the unit that the clinical staff are called to. D.g. in the ICU unit, EU, theatres, diagnostic radiology unit, paediatric unit, maternity unit or close to the surgical and medical inpatient units. The facilities should preferably be in a quiet area away from the patient areas.
Services
Provision should be made for the following:
- One data point per bedroom
- One double plug for computers
- One power outlet adjacent to the bed for a bedside lamp
- Toilet, shower and hand basin in shared ablution area
General requirements
Provision should be made for the following:
- Cupboard to hang clothes and store personal items
- Wall hooks for coats
Equipment
Provision should be made for the following:
- Bed and bedside table
- Desk to write and work on the computer
- Waste bin
- Easy chair
- Side lamp
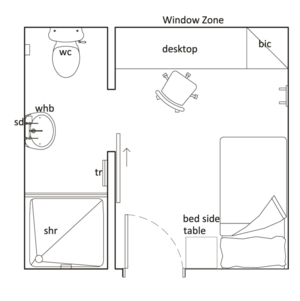
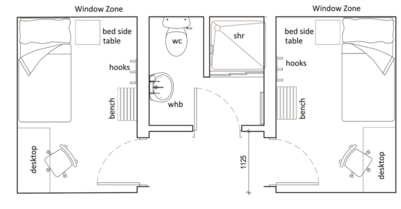
Administration Areas
Unit management office
Department of Public Works, 2005, Space planning norms and standards for office accommodation used by organs of state. (Government notice 1665). Cape Town, South Africa: Government Gazette.
Description and function
Depending on the level of care, offices are provided for nurses managers and, in some instances, for clinical heads of departments. Each office should provide accommodation for a single-person office to be used for clinical purposes. The office should have natural ventilation and a view to the outside. A minimum of 9 m² is recommended for clinical staff and 12 m² for a unit manager.
Location and relationships
The office of the unit manager should be near the entrance to the inpatient unit, central to the nurses' station and located away from the clinical areas and noise
Activities
Provision should be made for the following:
- Unit management writing reports
- Shift handover meetings
- Relative counselling
- Staff management
Services
Provision should be made for the following:
- IT and data connections
- Three electrical points and data point
- Telephone point
General requirements
Provision should be made for the following:
- Desk and two chairs
- Filing cabinet
- Stationery cupboard
- Pinboard
- Lockable office
Public areas
Public entrance to the inpatient unit
Description and function
There should be one main entrance to the inpatient unit. This should be the main access and exit to the inpatient facility. The fire escape should not be used as an entrance. In large facilities, provision is made for 400 beds and more. A general entrance and a service entrance are suggested.
Services
Access control id required
Inpatient unit corridor
Description and function
Circulation space linking rooms should maximize the use of the space to support turning circles and ease of access. Size depends on where the corridor is located.
General requirements
Natural light in patient areas is desirable.Waiting areas may be shared between inpatient units. Avoid any floor prostrutions that would influence wheels of beds and equipment. The width of a passage must allow at least two beds to pass in opposite directions, within the bumper rail measurement. The recommended minimum width for the main inpatient unit corridor (from bumper rail to bumper rail) is 2400 mm between bumper rails.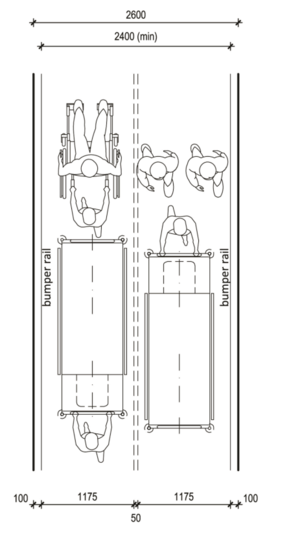
Visitors' waiting area
Description and function
An area for visitors and patients to wait prior to or during visits to the inpatient unit is best located outside the perimeter of the inpatient unit and may be shared by more than one unit.
Where visitors' lounge or waiting room is provided, it should be located and designed to accommodate child visitors without disruption to others. A room of 10 m² or 0.5 m² per able-bodied person is recommended, with 1 m² to be included per wheelchair-dependent person.
Location and relationships
The waiting area requires direct access to the circulation corridor and ready access to the public amenities. If a waiting area at unit level is provided, it should be located near the entrance to the unit. An external outlook is preferred with good natural light.
Activities
Provision should be made for the following:
- Visitors sitting or standing, and children playing
Services
Provision should be made for the following:
- One double plug
General requirements
Provision should be made for the following:
- Natural light is desirable
- Waiting areas may be shared between inpatient units
- A play area for children
- General and disabled-friendly ablutions
Equipment and furniture
Provision should be made for the following:
- Vending machine
- Public phones
- Waste paper or refuse bins
- Chairs
- Side tables
Public disabled toilet
Description and function
A room containing a toilet and a hand basin for use by disabled persons with or without assistance is required. A minimum size of 5 m² is recommended.
Location and relationships
The disabled toilet should have direct access to a waiting or circulation passage. Disabled toilets for public use should be readily accessible for public areas.
General requirements
Provision should be made for the following:
- Toilets at a special height for wheelchair users
- Clinical hand basin with elbow taps accessible for paraplegics while still siting on the toilet
- Wall-fixed toilet for cleaning underneath
- Mirrors - height and size is important for those using the facility
- Soap dispensers and hand towel dispensers - , hands-free
- Toilet roll holders in all toilets
- The door is to be fitted with escape hardware to allow staff access in case of an emergency
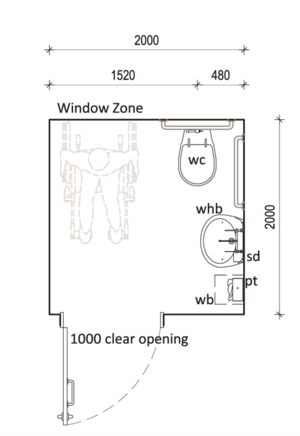


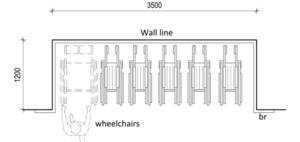
Engineering Considerations
- Vacuum, piped oxygen and medical gases
- Service panels enclosing oxygen, suction and air outlets
- Ventilation
- Fire detection and alarm systems
- Resilience of electrical supplies
- Lighting systems
- Internal drainage
- Nurse call system
- Security system
Standard Components
Standard Components (SC) refer to rooms and spaces for which room data sheets, room layout sheets (drawings) and textual descriptions have been developed and are available in a separate section of these guidelines.
List of rooms
The electrical, mechanical and health technology requirements for each space are given. There are a number of software packages that plot the equipment listed in the library with regard to the design in process.
The value of this type of system is that conflict of design principles can be detected early, such as door openings, spaces and the sizes of rooms in relation to the equipment for the space. (Code Book is a database system that could facilitate the development of a library for future use, Revit is a 3D design program)
Table 7: Example list of rooms for a 32-Bed inpatient unit
| Code | Room | Quantity |
|---|---|---|
| Patient area | ||
| 2-bed unit | 1 | |
| 4-bed unit | 7 | |
| En suite bathroom | 10 | |
| Entrance | 1 | |
| Single room | 2 | |
| Patient toilet | 1 | |
| Day room | 1 | |
| Assisted shower | 1 | |
| STAFF AREAS | ||
| Office - Sister | 1 | |
| Office - Doctor | 1 | |
| Nurse's station | 1 | |
| Staff shower | 1 | |
| Staff toilet | 1 | |
| Staffroom | 1 | |
| Staff locker area | 1 | |
| SUPPORT AREAS | ||
| Bay - Hand-washing | 10 | |
| Bay - Resuscitation trolley | 1 | |
| Cleaners' room | 2 | |
| Clean utility | 1 | |
| Dirty utility | 1 | |
| IT room | 1 | |
| Sluice - Clean linen | 1 | |
| Store - Equipment | 1 | |
| Store - General | 1 | |
| Store - Patient kit | 1 | |
| Store - Surgical | 1 | |
| Toilet - Disabled/ public | 1 | |
| Visitors waiting area | 1 | |
| Inpatient unit kitchen | 1 | |
| CIRCULATION | 32% | |
List of abbreviations
ACDP Advisory Committee on Dangerous Pathogens
ACH Air changes per hour
AHIA Australian Health Insurance Association
AII Airborne infection isolation
BP Blood pressure
CCD Central Cleaning Depot
CDC Centres for Disease Control
CSSD Central Sterile Services Department
ECG Electrocardiogram
HCU High care unit
HEPA High-efficiency particulate absorption
HIS Hospital information system
ICT Information and communication technology
ICU Intensive care unit
NDoH National Department of Health
NHLS National Health Laboratory Service
NHS National Health Service
NIBP Non-invasive blood pressure
PACS Non-invasive blood pressure
PAS Patient administration system
PE Protective environment
RIS Radiology information system
SARS Severe Acute Respiratory Syndrome
SC Standard components
TB tuberculosis
UPS Uninterrupted power supply
References
Centers for Disease Control and Prevention (CDC), 2003. Guidelines for environmental infection control in health-care facilities. (Recommendations of CDC and the healthcare infection control practices advisory committee HICPAC). Atlanta, GA: CDC. Department of Health, 2011. Adult in-patient accommodation: Planning and design manual. (Version:2951: 2.4: England). London, UK: Department of Health.
Growth Solutions Group (GSG), 2008. Specialist clinics wayfinding guidelines: The outpatient journey. [pdf] Victoria Australia: GSG. Available at: http://docs.health.vic.gov.au/docs/doc/B0C152FCA1338498CA25791700037BF4/$FILE/wayfindin g-guide.pdf [Accessed 31 March 2014].
NHS Estates, 2005. Ward layouts with single rooms and space for flexibility. The Stationery Office.
Standards Association of Australia (SAA), 2003. AS 1428.1-4: Design for access and mobility. New South Wales Australia: SAA.
The Centre for Health Assets Australasia (CHAA) faculty of the built environment the university of New South Wales (NSW), 2009. Wayfinding for healthcare facilities: Technical series TS-2: Prepared for: NSW health strategic business and development branch. (5th ed). NSW: NSW health department.
International Organisation for Standardisation (ISO), 2014. ISO 7000:2014 Graphical symbols for use on equipment- Registered symbols. Switzerland: ISO.