Difference between revisions of "Ventilation and COVID-19"
| Line 22: | Line 22: | ||
There is still little strong evidence of common long-range airborne transmission in the sense of droplet nucleation, as with TB and measles<ref>World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 16-24 February 2020 [Internet]. Geneva: World Health Organization; 2020 Available from: [https://www.who.int/docs/default- source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf https://www.who.int/docs/default- source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf]</ref>. Where evidence of airborne transmission has been reported, this can be seen in the context of opportunistic long-range droplet spread<ref> Wenzhao Chen, Nan Zhang, Jianjian Wei, Hui-LingYen, and Yuguo Li, “Short-range airborne route dominates exposure of respiratory infection during close contact,” medRxiv preprint, https://doi.org/10.1101/2020.03.16.20037291</ref>. A discussion contextualizing the reported cases of airborne transmission is discussed below. | There is still little strong evidence of common long-range airborne transmission in the sense of droplet nucleation, as with TB and measles<ref>World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 16-24 February 2020 [Internet]. Geneva: World Health Organization; 2020 Available from: [https://www.who.int/docs/default- source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf https://www.who.int/docs/default- source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf]</ref>. Where evidence of airborne transmission has been reported, this can be seen in the context of opportunistic long-range droplet spread<ref> Wenzhao Chen, Nan Zhang, Jianjian Wei, Hui-LingYen, and Yuguo Li, “Short-range airborne route dominates exposure of respiratory infection during close contact,” medRxiv preprint, https://doi.org/10.1101/2020.03.16.20037291</ref>. A discussion contextualizing the reported cases of airborne transmission is discussed below. | ||
| − | ==== van Doremalen et al (NEMJ 2020) ==== | + | ====van Doremalen et al (NEMJ 2020)==== |
The van Doremalen SARS-CoV-2 survival study<ref name="van Doremalen">Neeltje van Doremalen, Trenton Bushmaker, Dylan H. Morris, Myndi G. Holbrook, Amandine Gamble, Brandi N. Williamson, Azaibi Tamin, Jennifer L. Harcourt, Natalie J. Thornburg, Susan I. Gerber, James O. LloydSmith, Emmie de Wit, and Vincent J. Munster, “Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1,” The New England Journal of Medicine (2020), DOI: 10.1056/NEJMc2004973 [https://www.nejm.org/doi/pdf/10.1056/NEJMc2004973?articleTools=true]</ref> is often incorrectly reported to have shown that SARS-CoV-2 can remain viable in air for extended periods. No evidence for long range airborne viability has yet been found outside of lab settings. SARS-CoV-2 virus found dispersed at long range has not been cultured to prove viability and many studies have failed to detect it directly in air in quantities substantial enough to culture<ref>Faridi, S. et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 725, 1–5 (2020).</ref><ref>Liu, Y. et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature (2020) doi:10.1038/s41586-020-2271-3.</ref>. Correlations between culture viability, particle size and the real world infectious quantum were not described in this study<ref name="van Doremalen" /> as it was not the study's intention to claim COVID-19 was airborne. A more recent pre-publication article has made similar findings<ref>Fears SC, Klimstra WB, Duprex P, Hartman A, Weaver SC, Plante KS, et al. Persistence of severe acute respiratory syndrome coronavirus 2 in aerosol suspensions. Emerg Infect Dis. 2020 Sep [''date cited'']. <nowiki>https://doi.org/10.3201/eid2609.201806</nowiki></ref> but this has significant problems with equipment standardization and repeatability. More importantly, similar lab studies have also demonstrated a 3h airborne survival for viral strains such as Ebola not considered to be airborne<ref>Robert Comparison of the Aerosol Stability of 2 Strains of Zaire ebolavirus From the 1976 and 2013 Outbreaks Robert J. Fischer, Trenton Bushmaker, Seth Judson, Vincent J. Munster | The van Doremalen SARS-CoV-2 survival study<ref name="van Doremalen">Neeltje van Doremalen, Trenton Bushmaker, Dylan H. Morris, Myndi G. Holbrook, Amandine Gamble, Brandi N. Williamson, Azaibi Tamin, Jennifer L. Harcourt, Natalie J. Thornburg, Susan I. Gerber, James O. LloydSmith, Emmie de Wit, and Vincent J. Munster, “Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1,” The New England Journal of Medicine (2020), DOI: 10.1056/NEJMc2004973 [https://www.nejm.org/doi/pdf/10.1056/NEJMc2004973?articleTools=true]</ref> is often incorrectly reported to have shown that SARS-CoV-2 can remain viable in air for extended periods. No evidence for long range airborne viability has yet been found outside of lab settings. SARS-CoV-2 virus found dispersed at long range has not been cultured to prove viability and many studies have failed to detect it directly in air in quantities substantial enough to culture<ref>Faridi, S. et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 725, 1–5 (2020).</ref><ref>Liu, Y. et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature (2020) doi:10.1038/s41586-020-2271-3.</ref>. Correlations between culture viability, particle size and the real world infectious quantum were not described in this study<ref name="van Doremalen" /> as it was not the study's intention to claim COVID-19 was airborne. A more recent pre-publication article has made similar findings<ref>Fears SC, Klimstra WB, Duprex P, Hartman A, Weaver SC, Plante KS, et al. Persistence of severe acute respiratory syndrome coronavirus 2 in aerosol suspensions. Emerg Infect Dis. 2020 Sep [''date cited'']. <nowiki>https://doi.org/10.3201/eid2609.201806</nowiki></ref> but this has significant problems with equipment standardization and repeatability. More importantly, similar lab studies have also demonstrated a 3h airborne survival for viral strains such as Ebola not considered to be airborne<ref>Robert Comparison of the Aerosol Stability of 2 Strains of Zaire ebolavirus From the 1976 and 2013 Outbreaks Robert J. Fischer, Trenton Bushmaker, Seth Judson, Vincent J. Munster | ||
| − | J Infect Dis. 2016 Oct 15; 214(Suppl 3): S290–S293. Published online 2016 Oct 4. doi: 10.1093/infdis/jiw193 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5050463/</ref>. This makes the direct application of this lab study in real-world settings problematic. | + | J Infect Dis. 2016 Oct 15; 214(Suppl 3): S290–S293. Published online 2016 Oct 4. doi: 10.1093/infdis/jiw193 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5050463/</ref>. This makes the direct application of this lab study in real-world settings problematic. Therefore, the understanding of the mechanisms of COVID-19 transmission is still largely reliant on what is understood of SARS (SARS-CoV-1)<ref>Isao Arita, Kazunobu Kojima, and Miyuki Nakane, “Transmission of severe acute respiratory syndrome,” Emerging. Infectious Diseases 9 No. 9 (2003):1183-84, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3016764/].</ref>. |
| − | + | ==== Guangzhou Restaurant Outbreak (2020)<ref name=":0">Lu, J., Gu, J., Li, K., Xu, C., Su, W., Lai, Z....Yang, Z. (2020). COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. ''Emerging Infectious Diseases'', ''26''(7), 1628-1631. <nowiki>https://dx.doi.org/10.3201/eid2607.200764</nowiki>.[https://wwwnc.cdc.gov/eid/article/26/7/20-0764_article]</ref> ==== | |
| + | [[File:Guangzhou Restaurant COVID-19 2020.png|thumb|Plan of COVID-19 outbreak in Guangzhou Restaurant 2020<ref name=":0" />]] | ||
| + | The 2020 outbreak of COVID-19 in a restaurant in Guangzhou raises some important questions around the airborne spread of the disease. This study shows that the transmission range of COVID-19 may exceed the generally prescribed separation distance of 1m under certain conditions, but fails to do so convincingly. Confounding issues that are not addressed adequately in the articles conclusion include: | ||
| − | + | * the high probability of asymptomatic or pre-symptomatic spread of the virus from members of the index case's family<ref>How Coronavirus Infected Some, but Not All, in a Restaurant, Chang, K (2020) https://www.nytimes.com/2020/04/20/health/airflow-coronavirus-restaurants.html</ref> | |
| + | * the difference in exposure times between tables C-B and E-F are not addessed | ||
| + | * | ||
| − | < | + | |
| + | ==== Amoy Gardens SARS Outbreak (2003)<ref name=":1" /> ==== | ||
| + | Studies, which indicate the Amoy Gardens building's SARS outbreaks' transmission was via the airborne route<ref name=":1" />, commonly reference the prevailing wind between buildings. It should be noted that, since these buildings are about 60m apart the environmental dilution and concentration decay effects are so strong it is not feasible that an infectious dose persists at that range. Similarly, the possibility that air can commute out of one window and into another needs to account for these dilution effects before assumptions of transmission can be drawn. These studies do not sufficiently account for dilution, infectious doses and pathogen survival rates. A more feasible hypothesis is that the Amoy Gardens intra-building spread was through re-aerosolisation of contaminated waste water coming from the faulty plumbing system. Similar outbreaks have more recently been found<ref name=":2" /> | ||
| + | |||
| + | ==== Other studies ==== | ||
| + | Studies which have found real-world SARS-CoV-2 in air, ducting and on extraction fans have so far failed to prove that the virus found was still viable<ref>Santarpia et al, “Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center,. medRxiv preprint (2020), [https://doi.org/10.1101/2020.03.23.20039446]</ref><ref>Po Ying Chia et al, 2020 (Preprint) “Detection of Air and Surface Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Hospital Rooms of Infective Patients,” medRxiv preprint (2020), https://doi.org/10.1101/2020.03.29.20046557 [https://www.medrxiv.org/content/10.1101/2020.03.29.20046557v2.full.pdf]</ref>. Air sampling studies have failed to detect viable SARS-CoV-2 <ref>Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. ''JAMA.'' 2020;323(16):1610–1612. doi:10.1001/jama.2020.3227</ref>. | ||
| + | |||
| + | It has been suggested that high temperature and humidity would reduce the spread of the virus<ref>Chin, A. W. H. et al. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe 0–4 (2020) doi:10.1016/s2666-5247(20)30003-3.</ref><ref>Pyankov, O. V., Bodnev, S. A., Pyankova, O. G. & Agranovski, I. E. Survival of aerosolized coronavirus in the ambient air. J. Aerosol Sci. 115, (2018).</ref>. The temperature ranges suggested (>50°C) are beyond what anyone could endure in an ICU but the humidity ranges of between 40-60% are achievable. The high humidity slows the nucleation of the viral droplet and increases its settling speed, thereby reducing its range. | ||
====High Risk Settings (ICU)==== | ====High Risk Settings (ICU)==== | ||
Much of the work being done to understand the transmission mechanism of COVID-19 is focused on community transmission. It is important to remember that transmission risk in an ICU will not be the same as in homes and workplaces. The conditions and procedures in ICUs could promote transmission - see WHO 2020 below<ref name="WHO 2020">WHO 2020, Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations</ref>. Firstly, in a COVID ICU unit, the contamination source strength is much higher than other spaces since infected patients are congregated there. These are presumably ill patients with high viral shedding. Secondly, procedures like intubation are understood to release high quantities of aerosolized particles, unlike with general talking or coughing. Additionally, viral shedding through talking and coughing can be more readily mitigated than from intubation. | Much of the work being done to understand the transmission mechanism of COVID-19 is focused on community transmission. It is important to remember that transmission risk in an ICU will not be the same as in homes and workplaces. The conditions and procedures in ICUs could promote transmission - see WHO 2020 below<ref name="WHO 2020">WHO 2020, Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations</ref>. Firstly, in a COVID ICU unit, the contamination source strength is much higher than other spaces since infected patients are congregated there. These are presumably ill patients with high viral shedding. Secondly, procedures like intubation are understood to release high quantities of aerosolized particles, unlike with general talking or coughing. Additionally, viral shedding through talking and coughing can be more readily mitigated than from intubation. | ||
===Fecal-Oral Transmission=== | ===Fecal-Oral Transmission=== | ||
| − | Fecal oral route of transmission is acknowledged for COVID-19<ref>Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020;20(4):411-2.</ref> and considerations for waste water management are discussed [[SARS-CoV-2 is found in faecal matter|here]] and [https://doi.org/10.1016/j.scitotenv.2020.139076 here]<ref>Kitajima et al,SARS-CoV-2 in wastewater: State of the knowledge and research needs,Science of The Total Environment,Volume 739,2020,139076,ISSN 0048-9697,<nowiki>https://doi.org/10.1016/j.scitotenv.2020.139076</nowiki></ref> | + | Fecal oral route of transmission is acknowledged for COVID-19<ref>Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020;20(4):411-2.</ref> and considerations for waste water management are discussed [[SARS-CoV-2 is found in faecal matter|here]] and [https://doi.org/10.1016/j.scitotenv.2020.139076 here]<ref>Kitajima et al,SARS-CoV-2 in wastewater: State of the knowledge and research needs,Science of The Total Environment,Volume 739,2020,139076,ISSN 0048-9697,<nowiki>https://doi.org/10.1016/j.scitotenv.2020.139076</nowiki></ref>. This transmission route indirectly affects ventilation system design as special consideration should be given to common scenarios where the aerosolisation of contaminated wastewater is a possibility such as in bathrooms, sluice rooms and slurry pumping. These spaces should be well-ventilated and kept under negative pressure relative to adjacent spaces. |
| − | |||
| − | This transmission route indirectly affects ventilation system design as special consideration should be given to common scenarios where the aerosolisation of contaminated wastewater is a possibility such as in bathrooms, sluice rooms and slurry pumping. These spaces should be well-ventilated and kept under negative pressure relative to adjacent spaces. | ||
| − | ==== | + | ====Amoy Gardens SARS studies<ref name=":1">McKinney KR, Gong YY, Lewis TG. Environmental transmission of SARS at Amoy Gardens. ''J Environ Health''. 2006;68(9):26-52.</ref>==== |
| − | Studies, which indicate the Amoy Gardens building's SARS outbreaks' transmission was via the airborne route, commonly reference the prevailing wind between buildings. It should be noted that, since these buildings are about 60m apart the environmental dilution and concentration decay effects are so strong it is not feasible that an infectious dose persists at that range. Similarly, the possibility that air can commute out of one window and into another needs to account for these dilution effects before assumptions of transmission can be drawn. These studies do not sufficiently account for dilution, infectious doses and pathogen survival rates. A more feasible hypothesis is that the Amoy Gardens intra-building spread was through re-aerosolisation of contaminated waste water coming from the faulty plumbing system. Similar outbreaks have more recently been found<ref>Bhowmick, G.D., Dhar, D., Nath, D. et al. Coronavirus disease 2019 (COVID-19) outbreak: some serious consequences with urban and rural water cycle. npj Clean Water 3, 32 (2020). https://doi.org/10.1038/s41545-020-0079-1</ref> | + | Studies, which indicate the Amoy Gardens building's SARS outbreaks' transmission was via the airborne route<ref name=":1" />, commonly reference the prevailing wind between buildings. It should be noted that, since these buildings are about 60m apart the environmental dilution and concentration decay effects are so strong it is not feasible that an infectious dose persists at that range. Similarly, the possibility that air can commute out of one window and into another needs to account for these dilution effects before assumptions of transmission can be drawn. These studies do not sufficiently account for dilution, infectious doses and pathogen survival rates. A more feasible hypothesis is that the Amoy Gardens intra-building spread was through re-aerosolisation of contaminated waste water coming from the faulty plumbing system. Similar outbreaks have more recently been found<ref name=":2">Bhowmick, G.D., Dhar, D., Nath, D. et al. Coronavirus disease 2019 (COVID-19) outbreak: some serious consequences with urban and rural water cycle. npj Clean Water 3, 32 (2020). https://doi.org/10.1038/s41545-020-0079-1</ref> |
==Institutional Guidance== | ==Institutional Guidance== | ||
| Line 71: | Line 80: | ||
{{Expand}} | {{Expand}} | ||
| − | ==Air-Conditioning, | + | ==Air-Conditioning, Ventilation and COVID-19== |
It is important to differentiate between ventilation and air-conditioning when discussion indoor contamination. When the term ventilation is used, it describes any system that induces decontaminated, fresh or outdoor-air to enter a space by the application of supply or extraction systems. Diluting ventilation is the most commonly used regime. Other modes of contaminant removal include displacement and local exhaust ventilation systems, each of which requires its own nuanced discussion as they pertain to infection control. | It is important to differentiate between ventilation and air-conditioning when discussion indoor contamination. When the term ventilation is used, it describes any system that induces decontaminated, fresh or outdoor-air to enter a space by the application of supply or extraction systems. Diluting ventilation is the most commonly used regime. Other modes of contaminant removal include displacement and local exhaust ventilation systems, each of which requires its own nuanced discussion as they pertain to infection control. | ||
| Line 82: | Line 91: | ||
"In these resource limited settings, it needs to be carefully considered whether resources are allocated to clinical capacity or to possibly unnecessary ventilation when the benefits of these criteria may be comparatively marginal." | "In these resource limited settings, it needs to be carefully considered whether resources are allocated to clinical capacity or to possibly unnecessary ventilation when the benefits of these criteria may be comparatively marginal." | ||
| − | Without good viability studies of the viral particles found in ventilation systems, no firm guidance can be offered regarding the rate of reduction for SARS-CoV-2 viability with time and distance. Until that time it would be prudent to assume that the virus should only be considered as airborne under special and rare conditions, based on the guidance of the WHO. This would determine that we have different filtration and ventilation approaches between COVID-ICUs, general indoor public spaces and spaces with a potential for high density occupation. | + | Without good viability studies of the viral particles found in air or ventilation systems, no firm guidance can be offered regarding the rate of reduction for SARS-CoV-2 viability with time and distance. Until that time it would be prudent to assume that the virus should only be considered as airborne under special and rare conditions, based on the guidance of the WHO, and these conditions should be avoided. This would determine that we have different filtration and ventilation approaches between COVID-ICUs, general indoor public spaces and spaces with a potential for high density occupation. Engineers should not be tempted to assume or argue that all indoor spaces bear the same risk profile. |
For high-risk spaces it may be prudent to implement temporary measures to limit transmission risk to the minimum possible. In order of priorities, engineering interventions include: | For high-risk spaces it may be prudent to implement temporary measures to limit transmission risk to the minimum possible. In order of priorities, engineering interventions include: | ||
Revision as of 09:11, 16 July 2020
Contents
Context
This article aims to to contextualize COVID-19 related ventilation guidelines in a field of developing clinical evidence. This is done with the hope of empowering the reader to scrutinize proposed interventions within this context and employ appropriate and efficient solutions. The information and guidance in this article is the developing opinion of the author and does not represent any regulatory or institutional mandate or authority. The evidence supporting this opinion is evolving and therefore the opinion is similarly subject to change. The reader is encouraged to return to this article frequently to review any changes additions or updates highlighted in the history tab above.
Discussion and contributions are similarly welcomed in the discussion tab above.
Background
Transmission routes
SARS-CoV-2 has caused many to revisit their understanding of droplet and airborne transmission. These two transmission mechanisms form a continuum, but the following is generally accepted:
- Infectious particles <5μm in size can remain suspended and viable for many hours and these contribute to the risk of airborne transmission.
- Droplet transmission involves larger particles which can also spread through the air for some distance, but the range of transmission is generally considered to be less than 2 meters where after particles fall out of the breathing zone. It is important to remember that within this 2 m distance these larger droplets are essentially 'airborne' and diluting ventilation systems have little effect on reducing the risk of near-range droplet transmission[1].
Droplet precautions, therefore, include standard precautions like PPE, hand washing and distancing, while airborne precautions include negative pressure isolation, respiratory protection, special exhaust or filtration regimes, etc.
Diseases seldom obey only one mode of transmission (obligatory transmission) but often have preferences (preferential transmission) while occasionally exploiting circumstances which provide rare opportunities for transmission (opportunistic routes). SARS-COV-2 is understood to be preferentially droplet and contact spread (a form of droplet spread where droplets can settle on fomites) with possible rare and opportunistic airborne spread, although an extensive outbreak review revealed no indication of airborne spread[2].
Airborne Transmission
There is still little strong evidence of common long-range airborne transmission in the sense of droplet nucleation, as with TB and measles[3]. Where evidence of airborne transmission has been reported, this can be seen in the context of opportunistic long-range droplet spread[4]. A discussion contextualizing the reported cases of airborne transmission is discussed below.
van Doremalen et al (NEMJ 2020)
The van Doremalen SARS-CoV-2 survival study[5] is often incorrectly reported to have shown that SARS-CoV-2 can remain viable in air for extended periods. No evidence for long range airborne viability has yet been found outside of lab settings. SARS-CoV-2 virus found dispersed at long range has not been cultured to prove viability and many studies have failed to detect it directly in air in quantities substantial enough to culture[6][7]. Correlations between culture viability, particle size and the real world infectious quantum were not described in this study[5] as it was not the study's intention to claim COVID-19 was airborne. A more recent pre-publication article has made similar findings[8] but this has significant problems with equipment standardization and repeatability. More importantly, similar lab studies have also demonstrated a 3h airborne survival for viral strains such as Ebola not considered to be airborne[9]. This makes the direct application of this lab study in real-world settings problematic. Therefore, the understanding of the mechanisms of COVID-19 transmission is still largely reliant on what is understood of SARS (SARS-CoV-1)[10].
Guangzhou Restaurant Outbreak (2020)[11]
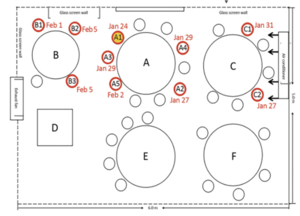
The 2020 outbreak of COVID-19 in a restaurant in Guangzhou raises some important questions around the airborne spread of the disease. This study shows that the transmission range of COVID-19 may exceed the generally prescribed separation distance of 1m under certain conditions, but fails to do so convincingly. Confounding issues that are not addressed adequately in the articles conclusion include:
- the high probability of asymptomatic or pre-symptomatic spread of the virus from members of the index case's family[12]
- the difference in exposure times between tables C-B and E-F are not addessed
Amoy Gardens SARS Outbreak (2003)[13]
Studies, which indicate the Amoy Gardens building's SARS outbreaks' transmission was via the airborne route[13], commonly reference the prevailing wind between buildings. It should be noted that, since these buildings are about 60m apart the environmental dilution and concentration decay effects are so strong it is not feasible that an infectious dose persists at that range. Similarly, the possibility that air can commute out of one window and into another needs to account for these dilution effects before assumptions of transmission can be drawn. These studies do not sufficiently account for dilution, infectious doses and pathogen survival rates. A more feasible hypothesis is that the Amoy Gardens intra-building spread was through re-aerosolisation of contaminated waste water coming from the faulty plumbing system. Similar outbreaks have more recently been found[14]
Other studies
Studies which have found real-world SARS-CoV-2 in air, ducting and on extraction fans have so far failed to prove that the virus found was still viable[15][16]. Air sampling studies have failed to detect viable SARS-CoV-2 [17].
It has been suggested that high temperature and humidity would reduce the spread of the virus[18][19]. The temperature ranges suggested (>50°C) are beyond what anyone could endure in an ICU but the humidity ranges of between 40-60% are achievable. The high humidity slows the nucleation of the viral droplet and increases its settling speed, thereby reducing its range.
High Risk Settings (ICU)
Much of the work being done to understand the transmission mechanism of COVID-19 is focused on community transmission. It is important to remember that transmission risk in an ICU will not be the same as in homes and workplaces. The conditions and procedures in ICUs could promote transmission - see WHO 2020 below[20]. Firstly, in a COVID ICU unit, the contamination source strength is much higher than other spaces since infected patients are congregated there. These are presumably ill patients with high viral shedding. Secondly, procedures like intubation are understood to release high quantities of aerosolized particles, unlike with general talking or coughing. Additionally, viral shedding through talking and coughing can be more readily mitigated than from intubation.
Fecal-Oral Transmission
Fecal oral route of transmission is acknowledged for COVID-19[21] and considerations for waste water management are discussed here and here[22]. This transmission route indirectly affects ventilation system design as special consideration should be given to common scenarios where the aerosolisation of contaminated wastewater is a possibility such as in bathrooms, sluice rooms and slurry pumping. These spaces should be well-ventilated and kept under negative pressure relative to adjacent spaces.
Amoy Gardens SARS studies[13]
Studies, which indicate the Amoy Gardens building's SARS outbreaks' transmission was via the airborne route[13], commonly reference the prevailing wind between buildings. It should be noted that, since these buildings are about 60m apart the environmental dilution and concentration decay effects are so strong it is not feasible that an infectious dose persists at that range. Similarly, the possibility that air can commute out of one window and into another needs to account for these dilution effects before assumptions of transmission can be drawn. These studies do not sufficiently account for dilution, infectious doses and pathogen survival rates. A more feasible hypothesis is that the Amoy Gardens intra-building spread was through re-aerosolisation of contaminated waste water coming from the faulty plumbing system. Similar outbreaks have more recently been found[14]
Institutional Guidance
WHO
The WHO's advice regarding SARS-CoV-2 transmission during clinical interventions is as follows:
"In the context of COVID-19, airborne transmission may be possible in specific circumstances and settings in which procedures or support treatments that generate aerosols are performed; i.e., endotracheal intubation, bronchoscopy, open suctioning, administration of nebulized treatment, manual ventilation before intubation, turning the patient to the prone position, disconnecting the patient from the ventilator, non-invasive positive-pressure ventilation, tracheostomy, and cardiopulmonary resuscitation." - WHO 2020[20]
While the WHO's position acknowledges the increased risk of transmission in overcrowded and under-ventilated spaces, the appropriate response is not to increase prescribed general ventilation rates, but rather to avoid overcrowding and maintain ventilation systems correctly.
US-CDC
The CDC's advice regarding SARS-CoV-2 transmission is still nearly identical to its guidance for SARS-CoV-1:
"The primary transmission of COVID-19 is from person-to-person through respiratory droplets. These droplets are released when someone with COVID-19 sneezes or coughs. COVID-19 can also be spread when you are in close contact with someone who is sick (e.g., shaking hands or talking). A physical distance of at least 1 meter (3ft) between persons is suggested by the World Health Organization (WHO) to avoid infection, although some WHO member states have recommended maintaining greater distances whenever possible. Respiratory droplets can land on objects or surfaces around the person when they cough or talk, and people can then become infected with COVID-19 from touching these objects or surfaces and then touching their eyes, nose or mouth. Recent data suggests that there can be transmission of COVID-19 through droplets of those with mild symptoms or those who do not feel ill" [23][24]
The US-CDC's recommendations regarding inpatient accommodation for SARS includes the comment,
"Experience in some settings in Taiwan and Toronto demonstrated that cohorting SARS patients, without use of AIIRs, effectively interrupted transmission"[25]
The CDC's guidance is consistent with the full context of hierarchical risk-based infection control and is suitably cognizant of variously resourced settings.
"Airborne Infection Isolation Rooms (AIIRs) (See definition of AIIR in appendix) should be reserved for patients who will be undergoing aerosol generating procedures (See Aerosol Generating Procedures Section)."[26]
This nuanced approach is difficult to tease out of the guidance from engineering societies.
ASHRAE
While the US-CDC and WHO maintains that the airborne transmission is possible but not common or of primary concern, ASHRAE (being an association dedicated to ventilation engineering) focuses on the airborne component.
"Transmission of SARS-CoV-2 through the air is sufficiently likely that airborne exposure to the virus should be controlled. Changes to building operations, including the operation of heating, ventilating, and air-conditioning systems, can reduce airborne exposures"[27]
ASHRAE makes useful distinctions between guidance for healthcare[28], residential [29][30], commercial [31] and schools[32], but doesn't significantly address risk categories specifically in healthcare or resource limited settings.
REHVA
REHVA's temporary guidance is limited to commercial and public buildings[33]. Similar to ASHRAE, REHVA focusses on engineering controls for airborne transmission. REHVA acknowledges importance of droplet precautions and the lack of quality evidence for airborne transmission, but draws the conclusion that SARS-CoV-2 RNA found in ventilation ducting implies airborne transmission, even though these real world studies have not yet proven viability of these particles. REHVA also draws the airborne conclusion from the van Doremalen study[5] out of its intended comparative context.
IUSS (2014)
The IUSS Building Engineering Services Guidelines[34], which is mandated for new buildings by provincial departments of health by reference in Government Notice R116[35], describes risk based ventilation criteria which are broadly appropriate for COVID-19, if not excessive. This guideline was developed with control measures for the current TB epidemic in mind. These measures would be more than appropriate for most healthcare spaces. The guidance recommends no recirculation of air between theatres and adjacent spaces but does not prohibit cascading from surgeries to adjacent spaces. Therefore, confirmed COVID-19 patients should only be treated in negative pressure operating rooms that comply with the guidelines.
SANS 10400-O (2011)
Please help to expand this page. |
Air-Conditioning, Ventilation and COVID-19
It is important to differentiate between ventilation and air-conditioning when discussion indoor contamination. When the term ventilation is used, it describes any system that induces decontaminated, fresh or outdoor-air to enter a space by the application of supply or extraction systems. Diluting ventilation is the most commonly used regime. Other modes of contaminant removal include displacement and local exhaust ventilation systems, each of which requires its own nuanced discussion as they pertain to infection control.
Air-conditioning in contrast, refers to only the mechanical cooling or heating system, sometimes installed directly in a space (Spit-AC), to offer thermal comfort and sometimes humidity control. In-room air-conditioning systems that circulate air directly within a space with no dilution or extraction can directly offer no reduction in airborne contaminant levels. In some instances they can even assist in the distribution of contaminants.
Openable windows can be considered as ventilation apertures and, in most cases, offer highly effective ventilation. Unfortunately, this is sometimes at the expense of indoor comfort. Even though long range droplet transmission of SARS-CoV-2 is relatively low in comparison to short range transmission, encouraging occupants to open windows will reduce that risk. Allowing occupants to use air-conditioning to either heat or cool a space while windows are open can improve levels of open window compliance which is more important than limiting AC use for reducing long range transmission. An additional strategy to both improve open window compliance and reduce AC usage would be to relax strict corporate dress codes as this can improve thermal comfort levels seasonally.
Engineering Response
Ventilation society guidance understandably bears the risk of being biased toward over-prescribing solutions over which engineers have the greatest understanding and control. It is within this context that the valuable guidance published online by REHVA and ASHRAE should be considered. Revamping existing ventilation systems in resource-constrained healthcare settings to meet admittedly overly-cautious guidance should not be conducted without an informed investment case.
"In these resource limited settings, it needs to be carefully considered whether resources are allocated to clinical capacity or to possibly unnecessary ventilation when the benefits of these criteria may be comparatively marginal."
Without good viability studies of the viral particles found in air or ventilation systems, no firm guidance can be offered regarding the rate of reduction for SARS-CoV-2 viability with time and distance. Until that time it would be prudent to assume that the virus should only be considered as airborne under special and rare conditions, based on the guidance of the WHO, and these conditions should be avoided. This would determine that we have different filtration and ventilation approaches between COVID-ICUs, general indoor public spaces and spaces with a potential for high density occupation. Engineers should not be tempted to assume or argue that all indoor spaces bear the same risk profile.
For high-risk spaces it may be prudent to implement temporary measures to limit transmission risk to the minimum possible. In order of priorities, engineering interventions include:
- decongest indoor spaces to the minimum possible occupancy levels
- open windows to outside when occupational health, safety and security are not compromised
- increase HVAC fresh air rates to maximum possible levels
- reduce HVAC recirculation levels to minimum possible levels
- flush buildings with fresh air before and after daily occupancy
The following matrix is intended to guide our design responses for a sample of space types
| Space Type | Risk | Initial Risk | Engineering Response | Residual Risk |
|---|---|---|---|---|
| ICU | Transmission in ICU | Severe |
|
Low |
| Transmission to Adjacent spaces | Low |
|
Low | |
| Surgeries | Transmission in Theatre | Severe |
|
Low |
| Transmission to Adjacent spaces | Moderate |
|
Low | |
| COVID Wards | Transmission within COVID-19 Ward | Low |
|
Low |
| Transmission to Adjacent spaces | High |
|
Low | |
| General wards | Transmission within and from Ward | Low |
|
Low |
| Emergency centre | Transmission within EC | High |
|
Moderate |
| Hospital Waiting Areas | Transmission within waiting room | High |
|
Moderate |
| Other public waiting spaces | Transmission within waiting room | Moderate |
|
Moderate |
Conclusion
Therefore, assuming ventilation systems in South Africa have been designed in accordance with the IUSS guidance, there should be little reason to change their configuration or pressurization unless general areas are repurposed as airborne precaution rooms. Risk assessments should be conducted for ICUs and COVID-19 wards immediately adjacent to public waiting areas or other high traffic areas, with corrective actions including but not limited to reducing occupancy times and rates for these areas.
Notes and References
- ↑ Liu, L., Li, Y., Nielsen, P. V., Wei, J. & Jensen, R. L. Short-range airborne transmission of expiratory droplets between two people. Indoor Air 1–11 (2016) doi:10.1111/ina.12314.
- ↑ https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations
- ↑ World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 16-24 February 2020 [Internet]. Geneva: World Health Organization; 2020 Available from: source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf https://www.who.int/docs/default- source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- ↑ Wenzhao Chen, Nan Zhang, Jianjian Wei, Hui-LingYen, and Yuguo Li, “Short-range airborne route dominates exposure of respiratory infection during close contact,” medRxiv preprint, https://doi.org/10.1101/2020.03.16.20037291
- ↑ 5.0 5.1 5.2 Neeltje van Doremalen, Trenton Bushmaker, Dylan H. Morris, Myndi G. Holbrook, Amandine Gamble, Brandi N. Williamson, Azaibi Tamin, Jennifer L. Harcourt, Natalie J. Thornburg, Susan I. Gerber, James O. LloydSmith, Emmie de Wit, and Vincent J. Munster, “Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1,” The New England Journal of Medicine (2020), DOI: 10.1056/NEJMc2004973 [1]
- ↑ Faridi, S. et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 725, 1–5 (2020).
- ↑ Liu, Y. et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature (2020) doi:10.1038/s41586-020-2271-3.
- ↑ Fears SC, Klimstra WB, Duprex P, Hartman A, Weaver SC, Plante KS, et al. Persistence of severe acute respiratory syndrome coronavirus 2 in aerosol suspensions. Emerg Infect Dis. 2020 Sep [date cited]. https://doi.org/10.3201/eid2609.201806
- ↑ Robert Comparison of the Aerosol Stability of 2 Strains of Zaire ebolavirus From the 1976 and 2013 Outbreaks Robert J. Fischer, Trenton Bushmaker, Seth Judson, Vincent J. Munster J Infect Dis. 2016 Oct 15; 214(Suppl 3): S290–S293. Published online 2016 Oct 4. doi: 10.1093/infdis/jiw193 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5050463/
- ↑ Isao Arita, Kazunobu Kojima, and Miyuki Nakane, “Transmission of severe acute respiratory syndrome,” Emerging. Infectious Diseases 9 No. 9 (2003):1183-84, [2].
- ↑ 11.0 11.1 Lu, J., Gu, J., Li, K., Xu, C., Su, W., Lai, Z....Yang, Z. (2020). COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. Emerging Infectious Diseases, 26(7), 1628-1631. https://dx.doi.org/10.3201/eid2607.200764.[3]
- ↑ How Coronavirus Infected Some, but Not All, in a Restaurant, Chang, K (2020) https://www.nytimes.com/2020/04/20/health/airflow-coronavirus-restaurants.html
- ↑ 13.0 13.1 13.2 13.3 McKinney KR, Gong YY, Lewis TG. Environmental transmission of SARS at Amoy Gardens. J Environ Health. 2006;68(9):26-52.
- ↑ 14.0 14.1 Bhowmick, G.D., Dhar, D., Nath, D. et al. Coronavirus disease 2019 (COVID-19) outbreak: some serious consequences with urban and rural water cycle. npj Clean Water 3, 32 (2020). https://doi.org/10.1038/s41545-020-0079-1
- ↑ Santarpia et al, “Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center,. medRxiv preprint (2020), [4]
- ↑ Po Ying Chia et al, 2020 (Preprint) “Detection of Air and Surface Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Hospital Rooms of Infective Patients,” medRxiv preprint (2020), https://doi.org/10.1101/2020.03.29.20046557 [5]
- ↑ Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. 2020;323(16):1610–1612. doi:10.1001/jama.2020.3227
- ↑ Chin, A. W. H. et al. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe 0–4 (2020) doi:10.1016/s2666-5247(20)30003-3.
- ↑ Pyankov, O. V., Bodnev, S. A., Pyankova, O. G. & Agranovski, I. E. Survival of aerosolized coronavirus in the ambient air. J. Aerosol Sci. 115, (2018).
- ↑ 20.0 20.1 WHO 2020, Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations
- ↑ Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020;20(4):411-2.
- ↑ Kitajima et al,SARS-CoV-2 in wastewater: State of the knowledge and research needs,Science of The Total Environment,Volume 739,2020,139076,ISSN 0048-9697,https://doi.org/10.1016/j.scitotenv.2020.139076
- ↑ https://www.cdc.gov/sars/about/faq.html
- ↑ https://www.cdc.gov/sars/about/faq.html
- ↑ US-CDC,2005, https://www.cdc.gov/sars/guidance/i-infection/healthcare.html
- ↑ Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic (updated July 9, 2020)[6]
- ↑ Q: Does ASHRAE’s guidance agree with guidance from WHO and CDC?[7]
- ↑ ASHRAE healthcare C19 guidance (ASHRAE 2020) [8]
- ↑ ASHRAE residential c19 guidance (ASHRAE 2020)[9]
- ↑ COVID 19 guidance for multifamily building owners-managers (ASHRAE 2020)[10]
- ↑ ASHRAE commercial C19 guidance (ASHRAE 2020)[11]
- ↑ ASHRAE Schools C19 guidance (ASHRAE 2020)[https://www.ashrae.org/file%20library/technical%20resources/covid-19/ashrae-schools-c19-guidance.pdf
- ↑ REHVA COVID-19 guidance document, April 3, 2020[12]
- ↑ Building Engineering Services (2014)[13]
- ↑ Government Notice R116 (17 Feb 2014)[14]