Difference between revisions of "Infection Prevention and Control/Surface Decontamination"
| Line 1: | Line 1: | ||
== Decontamination == | == Decontamination == | ||
Decontamination is the process of making an area safe by removing, neutralising or destroying any harmful substances. | Decontamination is the process of making an area safe by removing, neutralising or destroying any harmful substances. | ||
| − | === | + | === Cleaning === |
=== Sterilisation === | === Sterilisation === | ||
=== Disinfection === | === Disinfection === | ||
Revision as of 13:50, 15 May 2020
Contents
- 1 Decontamination
- 2 Surface Decontamination by Cleaning
- 3 Surface Decontamination by Heat
- 4 Surface Decontamination by Chemicals
- 5 Surface Decontamination by Irradiation
- 5.1 Ultraviolet Surface Disinfection for SARS-CoV-2
- 5.2 UV-C: potential for disinfection for SARS-CoV-2
- 5.3 Approaches to UVGI surface disinfection
- 5.4 Case Studies
- 5.5 Elements of a successful UVGI Disinfection Program
- 5.6 Safety
- 5.7 Maintenance and monitoring
- 5.8 UVGI lamps disposal
- 5.9 Training
- 6 Sampling and Validation
- 7 Notes and References
Decontamination
Decontamination is the process of making an area safe by removing, neutralising or destroying any harmful substances.
Cleaning
Sterilisation
Disinfection
Disinfection is the process of reducing the number of infectious agents to the level where they no longer cause disease.
Surface Decontamination by Cleaning
This is a section stub. See the discussion page for development
Surface Decontamination by Heat
This is a section stub. See the discussion page for development
Surface Decontamination by Chemicals
This is a section stub. See the discussion page for development
Surface Decontamination by Irradiation
Ultraviolet Surface Disinfection for SARS-CoV-2
UV-C air disinfection was been explored extensively in the context of TB infection prevention and control by the South African scientific community in association with international experts. National Technical Standards, Protocols, guidelines and testing capacity for application of upper-room UVGI in airborne transmission have been established[1]. This experience has provided important basic knowledge and key insights into the underpinning science and theory as well as application constraints, albeit for a different application.
Context
The coronavirus, SARSs-CoV-2, is understood to be transmitted primarily by contact and droplet spread[2].
Covid-19 is highly contagious and spreads more rapidly than its predecessors Severe Acute Respiratory Syndrome (SARS-Cov-1) and Middle East Respiratory Syndrome (MERS)</ref>[3], so any residual contamination can pose a public health threat[3]. COVID-19 transmission remains controversial as researchers across the globe remain conflicted about droplet and airborne as modes of transmission[3].
Clarifying the transmission routes and survival of viruses on frequently used surfaces is essential for containment of the outbreak. Research has successfully demonstrated that the virus has the potential to be aerosolised[4], and therefore can theoretically opportunistically transmit through the airborne route, it is understood that, except in aerosolising procedures, risk of coronavirus transmission via the airborne route [5] is low.
Similarly, risk via water and wastewater is low [6]. Persistence of the virus on a variety of surfaces has been demonstrated [4], underpinning concern that SARS-CoV-2 may be transmitted from infected (even asymptomatic) persons to others from touching common surfaces, even after the infector has departed for several hours [7][8]. Efforts to contain the coronavirus, to stem the pandemic, should therefore primarily focus on contact and droplet transmission.
Contact and droplet transmission is of concern in public transport systems taxis which convey very large transient populations is normally congested conditions, such as in trains and mini-bus taxis. Transfer of suspected or confirmed Covid-19 patients in planned transport or emergency service vehicles poses a risk since studies show that conventional decontamination procedures may be inadequat[5]. In a pandemic, and within already constrained healthcare infrastructure, overcrowding and close proximity of infectious and susceptible individuals will become highly. These conditions will amplify the risk of Covid-19 transmission.
In the South African context, the reduction of exposure to Covid-19 is a priority, in order to:
- reduce and delay occupational exposure of frontline workers especially healthcare and transport services workers;
- reduce exposure to public health risk, especially to the most vulnerable, such as PLHIV and persons with TB who are the principal users of public transport;
- contribute to the strategy of “flattening the curve”; and
- preserve and protect the healthcare service so as to ensure continued service.
This article proposes UV-C surface disinfection for reducing contact and droplet transmission of SARS-CoV-2 through the following applications:
- Portable disinfection devices for use in the transport sector (minibus taxis, trains and emergency and planned patient transport)
- Public Spaces
- Commercial and industrial occupational settings
- Decontamination of personal and respiratory protection equipment
UV-C: potential for disinfection for SARS-CoV-2
The disinfection effect of ultraviolet light has been described for over 100 years[9]. It is effective against a variety of microorganisms and has been successfully deployed for the purpose of disinfection of water, air and surfaces. Effectiveness depends on a range of variables related to the microorganism of interest, environment and application. Ultraviolet radiation in the UV-C range has been used for its germicidal properties specifically for infection prevention and control - have been demonstrated to work at laboratory scale, in ducts, as upper room irradiation and as portable devices. Safety guidelines have been established (ACGIH)[3].
There is good reason to expect that SARS-CoV-2 will be susceptible to UV-C. UV-C, when applied at the correct dose as it has been found effective against influenza viruses [10]including human coronavirus [11][12] (SARS-CoV-1).
According to Kowalski et. al. [13], Covid-19 is susceptible to existing disinfection methods such as chemicals and exposure to ultraviolet radiation in the electromagnetic range ~ 200 – 280nm (UV-C) because of the similarity of its structure to other susceptible coronaviruses such as SARS-CoV-1 and MERS.
UVGI surface disinfection has advantages over chemical disinfection because:
- There is no off-gassing of chemicals or residual chemical contamination frequently associated with chemical-based disinfection methods. Therefore, vehicles or spaces can be occupied immediately after UVGI disinfection[14];
- It has high pathogen reduction rates when compared to chemical cleaning; and
- Chemical disinfection methods are time-consuming [15].
A guideline on hospital infection control [16][17] recommends the use of both UVGI and chemical disinfection since UVGI has no penetrating power on dust, dirt and grease, which may harbour microbial contamination. Exposure to UV-C may degrade some materials.
As SARS-CoV-2 is recent and novel, UVGI efficacy has not yet been conclusively established against this particular pathogen[3]. For the reasons stated above, UVGI – the exposure of potentially contaminated contact surfaces to UV-C is identified as a measure with good prospects to reduce and delay occupational exposure of healthcare and transport services workers, as well as their clientele, and to contribute to the strategy of “flattening the curve”.
Approaches to UVGI surface disinfection
The application of UVGI for surface disinfection usually involves the use of bare UVGI lamps. Two main approaches to surface disinfection systems are via permanently installed disinfection systems and portable disinfection systems. Permanently installed systems generally consist of bare UVGI lamp fixtures mounted on ceilings or walls. Portable UVGI systems are moved into a place temporarily to decontaminate surfaces [14]. Efficacy is dependent on the intensity of irradiation emitted from the device, proximity of the device to the surface being disinfected and exposure time. The reflectivity of the materials in the vicinity of exposure can increase or decrease efficacy. Shaded items not directly exposed to UV-C irradiation may not effectively be disinfected
Case Studies
Moscow trains
In Moscow, Russia, Kostyuchenko, et. al., [15], investigated the potential of UVGI disinfection on internal surfaces of train carriages and on escalator handrails. They found that the required UV doses for effective disinfection are higher than the theoretically calculated doses.
Ambulance decontamination [3]
Respiratory Protective Equipment decontamination [3]
Elements of a successful UVGI Disinfection Program
Messaging
It is important for messaging around a UVGI Disinfection Program to detail that UVGI can be safe and effective when applied according to a defined and validated protocol
The messaging program should include the following safety aspects:
- UVGI is a form of actinic radiation which does not cause skin cancer
- UVGI/UVC is not the same as UV found in outdoor sunlight
- UVGI can cause reversible skin and eye irritation
- Skin and eye protection should be worn when the possibility of irradiation is present
- UV Lamps should not be used for skin or hand sterilisation
The messaging program should include the following efficacy aspects:
- UVGI is a supplemental surface disinfection technology
- UVGI can be used to kill the new coronavirus as well as a number of other common pathogens
Efficacy
UVGI dose
The UV-C dose required to achieve a particular pathogen reduction rate is calculated from the single-stage decay equation:
S=e-kD
where:
- S is the Survival fractional [%]
- k is the UVGI rate constant [m2/J]
- D is the UVGI exposure dose [J/m2]
- S is the Survival fractional [%]
In the absence of a specific UVGI rate constant for SARS-CoV-2, Kowalski et. al. [13] have proposed an average value for the calculation of the required dose. The average rate constant from recent Coronavirus studies is shown in the table below.
| Microbe | D90 Dose J/m2 (J/cm2) | Uv k [m2/J] |
|---|---|---|
| SARS Coronavirus CoV-P9 | 40 (0.04) | 0.05750 [18] |
| SARS Coronavirus (Hanoi) | 134 (0.134) | 0.01720 [19] |
| SARS Coronavirus (Urbani) | 241 (0.241) | 0.00955 [20] |
| Average | 138 (0.138) | 0.02808 |
The required UVGI dose for SARS-CoV-2 for a 4 log reduction (99.99% pathogen reduction rate) is calculated by expressing the single-stage decay equation as follows:
ln(S)=-k·D·ln(e)
∴D = ln 0.0001/(-0.02828) = 328 mJ/cm2 =(0.328 J/cm2)
Validation
Validation testing for UVGI surface disinfecting systems is required to ensure that the UV dose for ≥99.99% level of pathogen inactivation is achieved. As the dose rate is a function of the UV sources output and its distance to the target, the manufacturer for non-static UVGI surface disinfecting systems should specify the design minimum distance away from a surface, the UVGI intensity on the surface and the time required to achieve ≥99.99% pathogen reduction.
For disinfection that has either dynamic source or target components, repeatability and confidence studies are required to ensure that the range of variability expected does not exceed acceptable limits for efficacy and safety
Safety
Studies of personnel practising proper UVGI exposure control measures have shown no harmful effects[16], [17] . Noncompliance with safety precautions can lead to injuries [17]. The following safety issues are associated with the handling of UV equipment.
UV light exposure
UV radiation exposure present hazards to the skin and the eyes [14] [21]. The ability of UV radiation to penetrate the eyes and skin depends on the wavelength.
UV radiation eye hazards
The UV wavelength is the determining factor as to which part(s) of the eye may absorb the radiation and suffer biological effects.
The table below shows the absorption of different UV wavelengths by the human eye.
| Wavelength {nm} | Cornea | Aqueous | Lens | Vitreous |
|---|---|---|---|---|
| 100-280 | 100% | 0% | 0% | 0% |
| 300 | 92% | 6% | 2% | 0% |
| 320 | 45% | 16% | 36% | 1% |
| 340 | 37% | 14% | 48% | 1% |
| 360 | 34% | 12% | 52% | 2% |
UVGI (UV wavelengths 200 to 280nm) cumulative exposure dose greater than 6mJ/cm2 [22] can cause temporary corneal injuries (photokeratitis and conjunctivitis [14]). Symptoms of corneal injuries (extreme pain in the eyes) present after 6 -12 hours of exposure and lasts for a few days during which corneal cells will recuperate [14][17].
UV radiation skin hazards
Because of poor penetration and absorption capability [16], UVGI cannot penetrate or cause permanent harm to human skin [21]. Some skin irritation or erythema may be experienced but this will generally clear up with proper care.
UV radiation exposure guidelines
The UV radiation exposure Threshold Limit Values for the eyes and skin published by the American Conference of Governmental Industrial Hygienists (ACGIH) [22] varies according to the UV wavelength. For UVGI, cumulative exposure dose greater than 6mJ/cm2 [22] is considered harmful to eyes and skin. Since UVGI surface disinfection systems use bare lamps with dose requirements exceeding 6 mJ/cm2 , adherence to PPE is highly recommended to avoid harm.
UV control measures
Administrative controls
Prevent unauthorized personnel from entering the UV radiation area.
Personal protective equipment (PPE)
Personal protective equipment (PPE) protects the wearer from harm due to UV radiation exposure. The following PPE should be worn when operating UVGI surface disinfection systems:
- Plastic goggles with side shields;
- Head, neck and face covering opaque to UV radiation;
- Soft cotton gloves and.
- Long-sleeved, tightly woven fabrics with SPF 15 or greater.
Burn safety
UV lamps, depending on the lamp technology, may operate at up to 900°C. The UV lamps and sleeves should be allowed to properly cool down before maintenance to minimize the risk of burns. The electrical equipment (e.g., ballasts) may also become hot during operation and should be evaluated prior to maintenance [23].
Lamp breakage issues and mercury exposure
UV lamps pose two safety hazards if broken; the lamps and sleeves are constructed of quartz that, when broken, can pose a risk of serious cuts, and UV lamps contain mercury that can create an inhalation or contact hazard [23].
UV-C effects on materials
UV radiation that is incident upon a surface can be transmitted, reflected or absorbed [17]. Absorption of UV causes photodegradation that result in an alteration to the colour, texture or mechanical properties of the materials [17]. Materials with high UV absorption indicate greater potential for photodegradation while those with high reflectivity indicate protective effects [14]. All metals do not experience damage under UV exposure [14]. Some of the materials that experience photodegradation are wood, plastic, Polyvinyl chloride (PVC), fabrics, paint and glass [14].
Maintenance and monitoring
Proper maintenance and monitoring of UVGI surface disinfection systems ensure continued efficacy. Maintenance tasks and their frequencies are shown in the table below.
| Task | Frequency | Action |
|---|---|---|
| Check lamp run time values | Monthly | Change lamps if operating hours exceeded design life of 9–10 thousand hours [14] |
| Check intensity of UV lamps | Bimonthly | Replace lamps when UVGI dose is equal to or less than the validated UVGI dose after verifying that this condition is caused by low lamp output. |
| Visually inspect bulbs to ensure all bulbs are operational. | Weekly | If the bulbs show visual dust accumulation, they should be cleaned. Lamps can be wiped clean with a cloth dampened with water or a cleaning agent like dilute alcohol [14] |
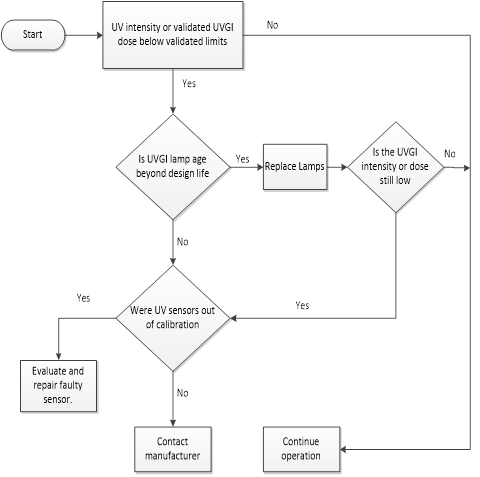
The surface UVGI system should be equipped with sensors that automatically monitor UV intensity, validated UV dose and lamps status. A decision chart for UVGI surface disinfection system monitoring is shown below.
UVGI lamps disposal
LPMV lamp contains mercury which is a toxic heavy metal which cycles through the soil, water and atmosphere in the environment. Send spent lamps to a mercury recycling facility or back to the manufacturer to prevent personal or environmental exposure.
Training
Operators designated to care for the UVGI systems should receive adequate training in both UV system theory, operation, maintenance and safety.
Sampling and Validation
Notes and References
- ↑ https://www.tb-ipcp.co.za/tools-resources/uvgi-documents/national-guidelines-abridged
- ↑ WHO 2020 Modes of transmission of the virus causing COVID-19: implications for IPC precaution recommendations https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-COVID-19-implications-for-ipc-precaution-recommendations
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Citation Needed
- ↑ 4.0 4.1 van Doremalen, N, Bushmaker, T, and Morris, DH e.tal Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New England Journal of Medicine. March 17, 2020 [1]
- ↑ 5.0 5.1 Lindsley, W.G, McLelland, T.L. and Neu, D.T. et. al. 2018. Ambulance Disinfection using Ultraviolet Germicidal Irradiation (UVGI): Effects of Fixture Location and Surface Reflectivity. [2]
- ↑ Steyn, M. (2020, April 8). Summary notes of the International Water Association (IWA) Webinar: “Covid-19: A Water Professional’s Perspective”. Infrastructure Guidance for COVID-19/Alternate Care Sites/COVID-19 A Water Professionals Perspective
- ↑ Cai et al, 2020, Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020, Emerging Infectious Diseases, 2020, https://wwwnc.cdc.gov/eid/article/26/6/20-0412_article
- ↑ Le et al, 2020, Asymptomatic and Human-to-Human Transmission of SARS-CoV-2 in a 2-Family Cluster, Xuzhou, China, Emerging Infectious Diseases, 2020, https://wwwnc.cdc.gov/eid/article/26/7/20-0718_article
- ↑ Downes, Arthur; Blunt, Thomas P. (19 December 1878). https://royalsocietypublishing.org/doi/pdf/10.1098/rspl.1878.0109
- ↑ Bean B, Moore EM, Sterner B, Peterson LR, Gerding DN, Balfour HH Jr. Survival of influenza viruses on environmental surfaces. J lnfect Dis 1982;146:47-51.
- ↑ Ijaz et al, 1985, Survival characteristics of airborne human coronavirus 229E. J Gen Virol. 1985 Dec;66 ( Pt 12):2743-8. https://www.ncbi.nlm.nih.gov/pubmed/2999318
- ↑ Lai MY, Cheng PK, Lim WW. Survival of severe acute respiratory syndrome coronavirus. Clin lnfect Dis 2005 https://www.ncbi.nlm.nih.gov/pubmed/16142653
- ↑ 13.0 13.1 13.2 Wladyslaw J. Kowalski, Thomas J Walsh, 2020. COVID-19 Coronavirus Ultraviolet Susceptibility. Technical Report · March 2020. [3]
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 14.7 14.8 14.9 Wladyslaw Kowalski, 2009. Ultraviolet Germicidal Irradiation Handbook: UVGI for Air and Surface Disinfection. New York. Springer. [4]
- ↑ 15.0 15.1 Sergey Kostyuchenko, Anna Khan, Sergey Volkov, Henk Giller, 2009. UV Disinfection in Moscow Metro Public Transport Systems. IUVA News / Vol. 11 No. 1 [5]
- ↑ 16.0 16.1 16.2 Brown IW Jr et al (1996) Toward further reducing wound infections in cardiac operations. Ann Thorac Surg 62(6):1783–1789.[6]
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 Shamim, I. A. ed., 2017. Ultraviolet Light in Human Health, Diseases and Environment. Cham, Switzerland: Springer International Publishing AG.[7]
- ↑ Duan SM, Zhao XS, Wen RF, Huang JJ, Pi GH, Zhang SX, Han J, Bi SL, Ruan L, Dong XP. (2003). Stability of SARS Coronavirus in Human Specimens and Environment and its Sensitivity to Heating and Environment and UV Irradiation. Biomed Environ Sci 16,246-255 [8]
- ↑ Liu Y, Cai Y, Zhang X. (2003). Induction of caspase-dependent apoptosis in cultured rat oligodendrocytes by murine coronavirus is mediated during cell entry and does not require virus replication. J Virol 77,11952-63. [9]
- ↑ Kariwa H, Fujii N, Takashima I. (2004). Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions, and chemical reagents. Jpn J Vet Res 52,105-112. [10]
- ↑ 21.0 21.1 21.2 Myung C. J., 2005. Ultraviolet (UV) Radiation Safety. Environmental Health and Safety University of Nevada Reno. [11]
- ↑ 22.0 22.1 22.2 American Conference of Governmental Industrial Hygienists (ACGIH), 2019. Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. ACGIH: USA [12]
- ↑ 23.0 23.1 Bolton, J.R., Cotton, C.A., 2008. The Ultraviolet Disinfection Handbook. Springer 2008. [13]