Hospital Design Principles
Contents
- 1 Policy and Service Context
- 2 Planning and Design
- 2.1 Enabling healthcare delivery
- 2.2 Hospital systems
- 2.3 Lean healthcare
- 2.4 Enabling life cycle efficacy
- 2.5 Lean design
- 2.6 Flexibility and adaptability
- 2.7 Sustainability and the environment
- 2.8 Future healthcare facilities
- 2.9 Site development
- 2.10 Master planning
- 2.11 Building design
- 2.11.1 Good design principles
- 2.11.2 Generic design
- 2.11.3 Ergonomics
- 2.11.4 Building engineering services
- 2.11.5 Direction and way-finding[15]
- 2.11.6 Inclusive environments
- 2.11.7 Safety and security
- 2.11.8 Supplies, storage and distribution
- 2.11.9 Building engineering systems
- 2.11.10 Compliance
- 2.11.11 Maintenance
- 2.11.12 Other – to be included...
- 3 Supporting Information
- 4 References
Policy and Service Context
Purpose
This document has been developed as part of a suite of guidelines, norms and standards for healthcare facility planners and designers both to indicate specific requirements to be met in the development of new and the upgrading of existing healthcare facilities for the public sector in South Africa, and to provide context for planners and designers. This document focuses on the form of the hospital and is supported and enabled, as indicated in section 2 below, by a range of other more focussed guidelines.
Overview
Hospitals provide the primary setting for the delivery of health care services. For patients the setting is important – patients expect an environment that will enable effective treatment for their condition, that will be pleasant and promote healing and that will be safe. While patient episodes of care are generally infrequent and of relatively short duration, the quality of the environment and experience can significantly influence both their physical and mental wellbeing as well as their rate of recovery. In contrast the hospital environment is the permanent place of work for staff. Their experience must ensure that they are enabled to carry out their duties in the most effective way possible. Good quality environments can positively enable delivery and lead to more effective patient outcomes while poor quality environments can lead to patient and staff frustration, both compromise service delivery and patient outcomes and increase the cost of service delivery.
This document is designed to provide a frame of reference for the planning and design of the whole hospital; at one level it provides the introduction to the suite of IUSS Guides, Norms and Standards (IUSS-GNS) for healthcare facilities, at another it synthesises the common requirements of all documents, providing the glue that links all the many clinical and support departments and services that make up the complex organism that is the hospital.
The Hospital Design Principles Guide is one of a set of 46 work packages making up the suite of IUSSGNS documents. The set of documents was structured into four broad subsets:
- Clinical and clinical support departments where there is direct contact between the patient and hospital staff
- Support departments providing administration, hospital support or facilities management services enabling the primary clinical services
- Cross cutting documents which impact many or all departments, and
- Procurement related documents including toolkits and guides impacting the planning, briefing, acquisition, commissioning, maintenance and decommissioning of healthcare facilities.
Many of these documents are interrelated and in order to avoid duplication information is located primarily in the document related to the primary function. Cross reference is made to documents where topics common to more than one department or unit are covered in more detail. For example specific requirements for infection prevention and control (IPC) will be highlighted directly where applicable, such as in the surgery or out-patient services documents but as IPC is critical across all healthcare facilities, the subject covered more thoroughly and in more detail in the IPC document.
The table below lists the full suite of documents and the key cross reference documents for the hospital design principles document.
| A: CLINICAL | Essential | Recommended | B: SUPPORT | Essential | Recommended | C: CROSS CUTTING | Essential | Recommended | D: PROCUREMENT | |||||
| A:01 | Accident and emergency | X | B:01 | Administration and related services | X | C:01 Generic room data | X | Integrated infrastructure
D:01 planning (IOPT toolkit) |
||||||
| A:02 | Critical care | X | B:02 | General hospital support services | X | Hospital design
C:02.1 principles |
D:02 Planning and briefing | x | ||||||
| A:03 | Adult in-patient services | X | B:03 | Catering services | X | C:02.2 Security | X | D:03 Space guidelines | X | |||||
| A:04 | Laboratories | X | B:04 | Laundry and linen | X | C:03 | Engineering design principles (BES) | X | D:04 Cost guidelines | X | ||||
| A:05 | Mental health services | x | B:05 | Mortuary | X | C:04 | Environment and sustainably | X | Order of Magnitude
D:04.1 (OoM) estimator |
x | ||||
| A:06 | Obstetrics & gynaecology | X | B:06 | Nursing education institutions (NEI's) | C:05 | Materials and finishes | X | Department level
D:04.2 estimator |
X | |||||
| A:07 | Oncology | X | B:07 | Health facility residential | x | C:06 | Future healthcare environments | x | D:04.3 Life cycle costing | X | ||||
| A:08 | Outpatient services | X | B:08 | Central sterile supply unit | X | C:07 | Healthcare technology | x | D:05 Procurement | |||||
| A:09 | Paediatrics and neonatology | X | B:09 | Clinical training | x | C:08 | Inclusive environments | X | D:06 Commissioning | x | ||||
| A:10 | Pharmacy | X | B:10 | Waste disposal | X | C:09 | Infection prevention and control | X | D:07 Maintenance | x | ||||
| A:11 | Primary health care | C:10 | Health informatics | x | D:08 Decommissioning | x | ||||||||
| A:12 | Diagnostic radiology | X | C:11 | Regulations | x | D:09 Capacity development | ||||||||
| A:13 | Rehabilitation & allied services | X | ||||||||||||
| A:14 | Sub-acute services | x | ||||||||||||
| A:15 | Operating theatres | X | ||||||||||||
| A:16 | TB services | X | ||||||||||||
IUSS guidelines and interdependencies table
This document outlines the policy and service context for a hospital project as well as providing detailed requirements and context for planning and design decisions that need to be considered during the development process. The document is divided into 3 main sections:
- Part A outlines the national and provincial service and policy context and briefly covers the key factors impacting on design development
- Part B covers more specific planning and design requirements through the various stages of design development and includes issues common to most hospital departments, while
- Part C includes schedules for further reading and references.
This document is designed to fulfil two primary functions:
- Firstly to act as a primer for healthcare facility planners and designers providing both background and contextual information on hospital design principles as well as references for further reading, and
- secondly to list specific requirements that the design team need to adhere to.
Sections which act as a primer are shown in normal font text, while those serving as specific requirements are highlighted in italic text and are listed under the relevant section.
Policy and service delivery context
Healthcare infrastructure and healthcare systems
The primary function of a health care system is to deliver services that will contribute towards the health and wellbeing of the community served. Facilities are part of the healthcare service system and require a set of allocated resources – including people, buildings, equipment drugs and supplies to operate effectively. The ability of the system to operate depends equally on the quality and effectiveness of the stewardship and oversight and on available and allocated funding.
The make-up of a particular facility depends on the defined service to be delivered as well as services provided from or shared with other related facilities (such as referred clinical services, breakdown and prepacking in the pharmacy for linked clinics or outsourcing laundry services). This must be defined in the project brief.
Healthcare facilities provide the environment through which healthcare services are delivered over the full life cycle of the asset. Facilities, usually with a life span of up to 50 years, are the most fixed component and therefore also potentially the most constraining aspect of the health care delivery system. Quality assets can positively enable the service; equally poor facilities can negatively impact service delivery. The more effectively the service is planned, defined and resourced the more likely that individual projects can be developed to provide an effective foil for service delivery. The better and more experienced the team deployed to a new or upgrade project, the more likely the resultant facility will be both enabling and resilient over time.
The context for service delivery for the specific facility that the professional team is tasked on, will be developed from the provincial Service Transformation Plan into the project brief.
Policy
Health service delivery in South Africa is provided under the framework of the National Health Act
Regulations
National Health Insurance (NHI)
Requirements:
A. The design of all healthcare facilities must allow for the provision of the required range of services envisaged under NHI and must be patient friendly, robust and sustainable over their planned service life.
“South Africa is in the process of introducing an innovative system of healthcare financing with far reaching consequences on the health of South Africans. The National Health Insurance commonly referred to as NHI will ensure that everyone has access to appropriate, efficient and quality health services. It will be phased-in over a period of 14 years. This will entail major changes in the service delivery structures, administrative and management systems.” (HST.org.za, 2014) In the service delivery model outlined in the NHI Green Paper (2012) NHI services will be provide through all existing healthcare facilities in South Africa supplemented where appropriate. Services will potentially be delivered from both the public and private sectors with the bulk of services continuing to be provided through the government network of facilities. Significant work will be required to ensure that all facilities can cater for the expanded range of services envisaged under NHI, to bring facilities up to the standards required and ensure that they can be readily and cost effectively managed and maintained at the required standard. Standards will be monitored by the Office of Standards Compliance.
Measuring performance
National Core Standards for Health Establishments in South Africa (NCS)
Requirements
A. Healthcare facilities must comply with the National Core Standards (NCS) set by the Office of Standards Compliance (OSC). As healthcare facilities will be assessed from time to time to review ongoing compliance as set out in the NCS, it is essential that planners and designers are acquainted with these requirements and plan and design accordingly.
The NCS (Republic of South Africa, 2011) were developed by the DoH to assist in setting the benchmark of quality healthcare against which delivery of services can be monitored. It addresses various aspects related to safety and security issues, particularly in the following two sections of the document: Domain 2: Patient Safety, Clinical Governance and Clinical Care covers how to ensure quality nursing and clinical care and ethical practice; reduce unintended harm to healthcare users or patients in identified cases of greater clinical risk; prevent or manage problems or adverse events, including healthcare associated infections; and support any affected patients or staff Domain 7: Facilities and Infrastructure covers the requirements for clean, safe and secure physical infrastructure (buildings, plant and machinery, equipment); functional, wellmanaged hospital services; and effective waste disposal (See Annexure B).
Project assessment
Requirements
A. The most significant impact on the functioning and operation of the proposed service is usually achieved through effective planning and design of the new facility or upgrade project. Generally the more quality time that is invested in project initiation and development the better the outcome will be.
Project plans and designs will be assessed during their development at the approval gates indicated in the Project Implementation Manual and as outlined in figure xx below.
Gateway process
Design assessment framework
Post occupancy evaluation
Performance monitoring
Infrastructure planning context
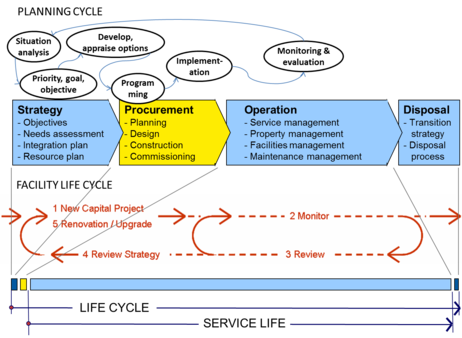
All healthcare facilities go through a life cycle starting with strategic service and project planning through to eventual decommissioning and disposal. This is illustrated in figure below.
Strategic planning
Infrastructure and service delivery
Infrastructure and healthcare service planning
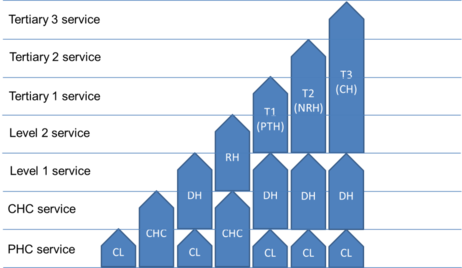
Infrastructure classification – facility classification vs levels of care
The classification of health care facilities and levels of care has been gazetted by the national Department of Health[1]. This shows types of facilities and levels of care. Some specialist services can however be provided at
Levels of care however are often shared across facility types as illustrated in figure below.
Document scope
Although many of the background and requirement design principles are similar for different types of healthcare facility, this document will focus on the design of all levels of hospitals. The design principles for clinics and Community Health Centres are covered in the IUSS-GNS document Primary Health Care.
Planning and Design
Enabling healthcare delivery
It is self-evident that hospitals and other healthcare facilities exist because of patients and the need for the delivery of appropriate and fully enabled health care services. The delivery of appropriate care requires a wide array of appropriate services, functional spaces and equipment, as defined in the brief, which provide the primary environment for clinical diagnosis, patient treatment and care. These spaces provide for and are supported by a wide range of clinical, administrative and facilities management systems and support systems that together enable the delivery of clinical care services. The delivery of appropriate care is further enabled, or impeded, by the decisions that are made around the shape, form, layout, flow, relationships, engineering systems, the selection and specification of materials and construction quality of the environment and the ability of the facility to accommodate and support the wide range of clinical, administrative and facilities management support systems that together form the hospital.
Before starting on the planning and design of a hospital project, it is important to understand those key principles that will inform the eventual design of the health care facility. The following principles focussed specifically on patient care and health service delivery are discussed in this section:
- Patient focussed care
- Evidence based design
- Salutogenesis
- Lean healthcare, and
- Hospital systems
A second set of principles, focused on enabling healthcare delivery over the service life of the facility will be addressed in the following chapter.
Patient-focussed care
Requirements:
A. Hospital planners and designers should be acquainted with the broad principles of patientfocussed care and should incorporate the principles into their designs
Patient-focussed (PFC) or patient-centred care provides a reminder that the design of a health care facility and the functioning of the healthcare service need to respond primarily to the needs of the patient. The Australian Commission on Safety and Quality in Healthcare (ACSQH) defines patientcentred care as “care that is respectful of, and responsive to, the preferences, needs and values of patients and consumers. The widely accepted dimensions of patient centred care are respect, emotional support, physical comfort, information and communication, continuity and transition, care coordination, involvement of family and carers, and access to care.”[2]
While most aspects of PFC relate to the care-giving process, these activities are either enabled or constrained by the physical environment and the two need to be seen as wholly interconnected.
ACSQH goes on to note that “research demonstrates that patient-centred care improves patient care experience and creates public value for services. When healthcare administrators, providers, patients and families work in partnership, the quality and safety of health care rise, costs decrease, and provider satisfaction increases and patient care experience improves. Patient-centred care can also positively affect business metrics such as finances, quality, safety, satisfaction and market share.”
The design focus of PFC is to identify those aspects of the physical design and equipping of the patient care environment which can be effectively controlled during planning, design and operational management of the facility.
Research papers and literature on patient focussed care can be found in section 16 of this document.
Evidence based design
Requirements:
A. Hospital planners and designers should be acquainted with the broad principles of evidence based design and should incorporate the principles into their designs
Many of the concepts and objectives highlighted in PFC are consolidated into a hospital design research framework known as evidence based design (EBD). EBD is the process of basing decisions about the built environment on credible research to achieve the best possible outcomes[3]. This concept initially researched and reported at the University of xxx by Roger Ulrich, seeks to identify all research papers related to the patient experience in hospital that are linked in some way to the physical environment and to draw from these recommendations which will assist healthcare planners and designers to create the right physical environment to support PFC.
This resulting research informed design process is seen as a deliberate process for creating hospitals and other healthcare design buildings informed by the best available evidence, with the goal of improving safety, medical, staff and financial outcomes.[4] Ulrich also notes that the state of knowledge of evidence based healthcare design has grown rapidly in recent years. The evidence indicates that well-designed physical settings play an important role in making hospitals safer and more healing for patients and better places for staff to work.[5]
Specific design requirements that come out of the PFC and EBD environment will be expanded on in later chapters on:
- Evidence based design
- Ergonomics
- Recognising specific populations
- Daylight, lighting and health
- Ventilation
- Infection control
Laura’s slides:
“Research informed design:” it refers to a
The four components of an Evidence-Based Design Process are:
- gather qualitative and quantitative intelligence
- map strategic, cultural, and research goals
- hypothesize, outcomes, innovate, and implement translational design, and
- measure and share outcomes[6]. From "
Definition:
Evidence-Based Design is the process of basing decisions about the built environment on credible research to achieve the best possible outcomes http://www.healthdesign.org/aboutus/mission/EBD_definition.php
Research papers and literature on evidence based design can be found in section 16 of this document.
Context
Background – hospitals are dangerous places, complex, interface between technology and human caring;
In a comprehensive literature study Ulrich et al searched for links between building design decisions and medical outcome through the patients stay in hospital. The study identified the following key evidence based design areas that the healthcare facility planners and designers need to address:
- Improving patient safety through environmental measures. This can be further subdivided into:
o Reducing hospital-acquired infections
o Reducing medical errors o Reducing patient falls
- Improving other patient outcomes through environmental measures, including o Reducing pain o Improving patients sleep o Reducing patient stress o Reducing depression o Reducing length of stay o Reducing patient disorientation o Improving patient privacy and confidentiality o Improving communication with patients and family members o Fostering social support o Improving patient satisfaction
- Improving staff outcomes through environmental measures o Decreasing staff injuries o Decreasing staff stress o Increasing staff effectiveness o Increasing staff satisfaction
Important to understand hospital acquired infection and possible modes of transmission – refer to IUSS-GNS document Infection prevention and control. Impact on design layout, selection and location of fittings, ventilation, selection of finishes, ...
Salutogenesis
Many of the design concepts developed from patient focussed care are also found in concept of psychosocially supported hospital design proposed by Alan Dilani in turn based on the concept of Salutogenesis (Dilani, 2009). Salutogenesis7, originally conceived by Aaron Antonovsky in the 1970’s, proposes an alternative to the disease based model of incidence based care which focuses on curative based restorative care, instead focussing on those factors that impact on the creation of health, primarily the relationship between health, stress and coping.
This approach of focusing on a positively reinforcing both the lifestyle environment and coping mechanisms can assist with inevitable stress incidences and lead to improved health. WHO defines health as “a state of complete physical, psychological and social well-being; not only the absence of illness”. This links in to the xxx Constitution xxx and the primary objective of the health care system as shown in figure 1, of enabling and support of the health and wellbeing of the population.
Factors that affect health include:
- genetics – heredity, ethnicity
- biological – sex, age, disease
- social – profession, economy, network
- life style – food, exercise, smoking, alcohol
- personality – attitudes, values, emotions, temperament
- risk factors – life events, risk behaviour, nature catastrophes, danger, violence, and
- environment – geographic place, climate, pollutions, social environment, physical environment, design
While the primary focus in healthcare facilities is on the design of the physical environment, other factors in planning include a move from curative to wellness and health promotion centres. More on this concept? In PHC (more than in L2/3?) health promoting centres could include community support services such as community
In common with the concepts outlined in chapter 6.1 on patient focused care, salutogenesis also focuses on
Factors that affect health
Creating socially supportive environments
Places for ’meeting’ and ’contemplation
Music and Health
Daylighting
Art, Culture and Health Perception and Way finding access to green areas for recreation”
Design for positive psychosocial stimuli and restoration
Restorative Environment Nature and Light
”Health is a state of complete physical, psychological and social well-being; not only the absence of llness!” WHO
Hospital systems
Requirements:
A. Hospital planners must review all systems in the specific context for their project and must define the requirements for each providing sufficient detail both for the design team to understand and create the right environment for service delivery, and for the commissioning team to enable and initiate the service
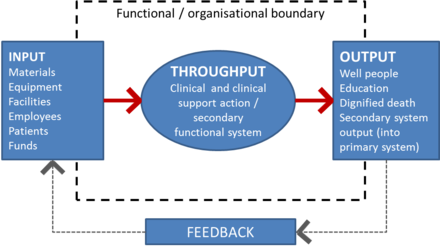
Hospitals are built around a complex interrelationship of systems that together enable the people, equipment, supplies into a defined environment at the right time to enable a specific healthcare activity to be performed and, after completion, for the space to be recycled for the next activity. These systems need to be defined and managed and require the right series of delivery, storage, process, delivery and recycling spaces and routes through the facility.
At a high level systems require four actions: input, throughput, output with a feedback loop as illustrated in figure xx below:
Hospital support systems include:
7 Derived from the Latin salus for health and the Greek genesis for origin.
8 Adapted from Sullivan & Decker, 1998. Effective Leadership & Management in Nursing.
- Catering
- Laundry and linen
- Pharmacy
- Materials handling
- Waste system
Catering system
Laundry and linen system
Pharmacy system
Pharmaceutical supplies need to be delivered directly to the pharmacy and offloaded into a security cage. Dispensed output is either directly to outpatients (close relationship to OPD essential, figure xx), delivered to point of use clinical departments – define whether top, or collected by staff from the pharmacy (e.g. ward prescriptions). High level security of the pharmacy and security on delivery routes is essential. Full details are contained in the IUSS GNS document Pharmacy.
Materials handling system
Waste system
Provision must be made for the safe collection and holding of waste at point of generation, waste collection and removal to a central holding point, and disposal from the site. Waste disposal pathways should as far as possible be separated from patient and public pathways. In larger facilities this may involve separate service corridors and lifts. Full details of waste management system options and requirements are included in the IUSS GNS document Infrastructure Design for Waste Management in Healthcare facilities.
Lean healthcare
Developed and widely applied in the industrial sector, lean thinking has more recently been applied in the health sector9. Application can be both in the delivery and management of healthcare services as well as in the planning, design and construction process for healthcare facilities. This latter will be discussed in more detail in section 8.2 following.
Simply put lean thinking means using less to do more10. Lean thinking is applied through a structured review of
9 Lean Health Care: What Can Hospitals Learn from a World-Class Automaker? Kim CS, Spahlinger DA, Kin JM, Billi
JE. Society of Hospital Medicine. Published online in Wiley InterScience. 2006.
10 Going Lean in Health Care. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2005.
Developed from the relentless dedication by Toyota towards quality improvement in everything it does, lean production is based on a programme of focused continuous improvement working through efficiency gains, waste reduction, increasing product quality and respect for people. The end result for Toyota is a learning organization that values employee contributions and continuously strives to produce products of higher quality at lower cost. These lean concepts have since been applied in many industries and more recently been brought into hospital planning, operation and management.
Lean healthcare
As indicated above hospital and clinical systems can be reviewed in terms of ‘input, throughput, output’ equation. Applied in the healthcare environment, Toyota’s Value Stream Mapping (VSM) process can be used to represent the key people, material, and information flows required to deliver a product or service in order to distinguish between value-adding and non–value-adding steps. Significant improvements reducing medical errors, containing costs and minimising the impact of staff shortages have been recorded[1]. In developing new facilities planners should review existing processes
“lean thinking”? Simply put, lean means using less to do more. (IHI p2) objective to streamline processes, reduce cost, and improve quality and timely delivery of products and services
Enabling life cycle efficacy
Affordability and life cycle
Requirements:
A. Hospital planners and designers need to develop projects which offer an optimum balance between capital cost and life cycle costing of the operation of the healthcare service. Healthcare service operation includes both the provision of the clinical service, the supporting and enabling services as well as the cost of the management and maintenance of the physical facility and healthcare technology.
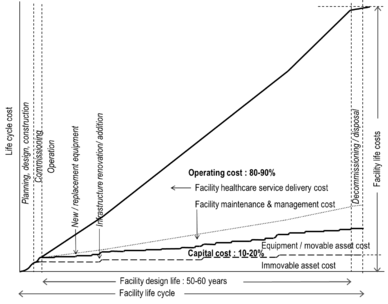
Capital projects are not an end in themselves. A key consideration during the development of a project must be the cost and ease of operation over the full life cycle of the facility. The initial capital cost over the service life of the facility plus reinvestment for upgrades and renovations amounts to some 5-10% of the total life cycle cost incurred through the asset (ref). Healthcare technology costs, while initially only some 20-50% of the capital cost of the buildings, can equal or surpass that of the buildings over the service life of the asset as replacement of clinical equipment generally occurs at a far faster rate than building components. Figure xx below highlights the cumulative costs incurred through the operation of a healthcare facility over its life cycle. The scale of the vertical axis is dependent on the size and type of facility. As a rule of thumb operational costs equal capital costs after about 3 years of service operation.
The initial planning and design phase offers a unique opportunity to create the right environment to positively enable and support health service delivery through the operational life of the facility. It is critical to ensure that adequate time and resources are assigned to the initial planning and design development process. Key planning decisions include the size and type of service....
Sound lifecycle based decisions – for both engineering systems and detailing and materials – can also significantly impact the facility maintenance and management costs through the lifecycle of the facility.
Cumulative total cost of service provision highlighting the relationship between capital and operating costs over the life cycle of the asset as well as the critical importance of the initial decision making processes in the lead in to the project on the total cost of service delivery
Lean design
Flexibility and adaptability
Requirements:
A. Hospital planners and designers need both to recognise that changes to the physical layout, structure or engineering services will happen over the service life of the facility and that adequate measures to enable such change to take place with minimum disruption to ongoing service delivery need to be taken during the initial planning and design process
Change in healthcare facilities is inevitable over time. Whether it is due to changes in the demographic or disease profile of the community served, changes in policy or level of care, changes in technology or practice, the one certainty is that reallocation of room function, minor or major refurbishment, remodelling or large scale redevelopment will occur during the service life of a facility. This may require minor or major decanting of sections of the facility.
Change is likely to occur
Time and nature of change
Location
- workplace / work environment / system or service level
Impact
- minimal - change in routine, equipment or furniture
Risk
Research undertaken at a number of hospitals in Australia highlights a number of features that have assisted to accommodate change over the service life of these facilities[1]. These included:
- “A large site with appropriate healthcare‐related zoning...
- Design around a hospital ‘street’ or spine with preferably 3‐6 storey buildings that allows expansion at either end or to various units along the spine (outward or upward)...
- Capacity to upgrade building services on a zone by zone basis..., and
- Use of a modular grid that supports a range of functions.”[2]
Site size and master planning guidelines including provision for future expansion is discussed further in sections 8.1 and 9.1 below.
Taking the need for flexibility and adaptability into account “an optimal design is one that inhibits change of function least… rather than one that fits a specific function best”.14
Refer also to Section 21 Research Literature for further references and discussion on Flexibility and Adaptability.
Sustainability and the environment
Ecopoints
Future healthcare facilities
Requirements:
A. Hospital planners and designers in developing their project designs need to take into account both the likely future trends outlined below as well as the provisions listed below which will help to facilitate inevitable change over time
Change in healthcare service delivery is inevitable over time. This may be due to changing dynamics of the community served, of the service delivery model, of technology – medical or infrastructure – or even of ? Technology changes can be very rapid – the first fully mobile cell phone, introduced less than 25 years ago, has now become ubiquitous and has the potential to impact the place and mode of health service delivery – see IUSS GNS discussion document Future Healthcare Environments. With a planned service life of half a century or more, physical buildings however provide a sea anchor to service delivery often constraining the service delivered. With a long lead-in and procurement time, coupled to rapid changes in technology and service delivery policy, many new facilities can become out-of-date by the time or shortly after they are commissioned[3].
It is important therefore to try both to understand the future drivers for change, future issues and likely future trends as well as to try to future proof designs to allow them to accommodate inevitable change over time.
Future drivers, issues and trends
Population growth will continue to focus on a few key geographical centres in South Africa (Gauteng,
Western Cape, KZN)
Consumption of scarce resources (energy and water) will continue to increase
Resource consumption pressures will increase on commodities
Demand for services and infrastructure will continue to escalate
Climate change impacts will be manifest in South Africa (severe disruption of weather patterns)
Future proofing design
While new facilities can be designed to reflect current technology and thinking and even to anticipate change, the service delivery environment, technology and particularly medical technology changes at a far greater rate and, with a long planning and procurement lead time, (Abbott et al, 2008).
Site development
Site selection
Requirements:
A. Site selection is a critical aspect of health service delivery. Sites should at once be centred on the community served, allow easy and safe access, be of sufficient size, available and suitable to build on.
B. Where possible site sizes and the potential for placing of the facility must allow both for later expansion of the service and/ or facility and for possible phased expansion or rebuilding and decanting with minimum disruption to ongoing service delivery [see 7.5 above]
Once the need for a new or upgrading health infrastructure project has been established during strategic health service planning (see section xx above) for a specific community a range of criteria need to be reviewed in terms of the existing or potential new sites. These can be grouped according to general site selection criteria and specific health service delivery requirements.
Location in relation to community served – essential for district hospital where there is a direct relationship between feeder community and facility; for regional hospitals consider both the referring hospitals, the broader community served
Site size
Suitability
Site selection
Site selection criteria
Consider the site in relation to the following criteria:
| Issue | General requirement | Comments |
| Health service delivery | Location in relation to community served | Generally central to the bulk of the catchment population for the proposed service. At primary health care level including district hospitals there is a relatively direct geographic link between community and facility; at regional and tertiary levels the link is less direct with transport and specialisation playing more direct roles |
| Location in relation to health service referral network of facilities and service delivery points | ||
| Options analysis and optimisation of service to establish best fit for service and infrastructure | IOPT Planning Toolkit enables service coverage analysis and status quo review of existing facilities and services, and of various options for changes to services and any possible new facilities | |
| Current development | Brownfield site - review suitability and potential for expansion or redevelopment | Obtain site plan showing current development, usage, coverage, site services, access points |
| Review potential for phased redevelopment (see section xx flexibility and adaptablity) | ||
| Establish demolition requirements and implications including potential for recycling and reuse of construction waste | ||
| Heritage | Establish heritage status of site and any specific buildings | Review implications in terms of suitability of site/
buildings for redevelopment and reuse; Review heritage reporting requirement |
| Geographic location and features | Site shape, slope, relationship to | |
| Suitability and impact on health service delivery of surrounding | ||
| development (industrial…) | ||
| Prevailing winds and micro climate | ||
| Geological conditions | Site preferably free of ground conditions which will require special foundations. Geological survey may be required. | Establish presence, extent and distribution of dolomite, rock outcrops, sand, landfill, etc. |
| Access | Site readily accessible from major roads to allow unimpeded
access to service by community, emergency vehicles |
|
| Suitability of location in relation to existing and proposed roads, rail, bus, taxi routes | Current services and future services | |
| Site entry and traffic control; establish need for traffic studies | ||
| Safe pedestrian access to site | ||
| Helicopter access possible | Review access flight path to site and any potential conflict with other aircraft flight paths | |
| Environmental | ||
| Availability | Site to be preferably available for use without the need for lengthy procurement processes | Establish ownership, land use rights;
Potential land acquisition costs; Establish acquisition process and potential transfer time and implications on project time programme |
| Bulk services | Availability of water, electricity, sewage services | |
| Communication | Access to telephone | |
| Etc | Etc | Etc |
More details are available from DPW...
Site size
9.2 Site planning/ zoning
Or is this master planning – omit here?
Access and traffic management
Roads, paving and parking / Roads and hard surfaces
Landscaping
Fencing
Security
Lighting
Master planning
Site and buildings
Zoning
Allow space for expansion – quadrant and empty chair – Carthey/ Gronigen – also Roger in Beijing • Design around a hospital ‘street’ or spine with preferably 3‐6 storey buildings that allows expansion at either end or to various units along the spine (outward or upward)... This strategy also facilitates the refurbishment or upgrade of various parts of the hospital without negatively impacting on the remaining parts in terms of noise or other disruption.
Building form and massing
Activity, relationships and flow
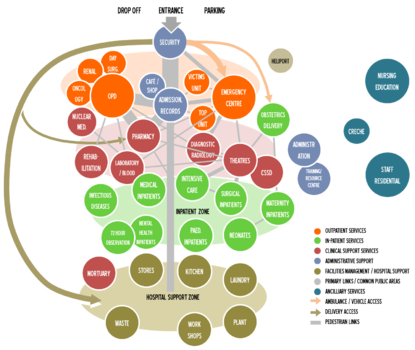
Hospitals are complex organisms with critical key relationships, linkages and circulation routes catering for the general public – including outpatients, for clinical staff, for visitors and for hospital support staff – including delivery trolleys, and for hospital technical and maintenance staff. Routes for outpatients should be direct and ideally such that progression further into the body of the hospital is limited.
Daily hospital activity
Significant numbers of people visit hospitals on a daily basis. Projections made from a study of Limpopo hospital data indicate that an average 400 bed hospital could be expected to have about 2 100 arrivals per day made up of approximately 45% OPD visits, 5% emergency, 1.5% delivery, 6% admissions, 12.5% visitors and 30% staff. Provision was made for those accompanying patients but not for peak load variations.[4] All this needs to pass through the main site entrance and security point and a significant proportion through the main entrance/ admissions point.
Relationships and flow
With the large numbers arriving at facilities those departments with high loads should be located on the entrance (generally ground) level closest to the entrance to the site (OPD) along with those where the need is greatest for rapid response (emergency). As maternity is a 24 hour service it too should be close to and ideally clearly visible from the entrance. From these small clusters of departments circulation patterns develop reflecting primary patient flow such as admissions – OPD – pharmacy – admissions and emergency – diagnostic radiology – theatres – ICU – in-patient wards. Some outpatients are also referred for rehabilitation services and for laboratory tests.
Day surgery, renal unit and oncology (chemotherapy) are all primarily outpatient functions closely linked to the OPD. Nuclear medicine (radiation therapy) is both an outpatient and inpatient service and should allow access from both zones. Some chemotherapy patients are also treated as inpatients.
The termination of pregnancy (TOP) unit, while an outpatient service, should ideally be located away from main outpatients in a quiet and inconspicuous area. This operates during normal outpatient hours.
The 24 hour victims of violence unit should be easily accessible from outside, close to emergency where emergency care can be provided if required but should also be quiet and inconspicuous and provide a secure environment.
Most hospitals need to provide for:
Figure xx below highlights primary clustering of departments within zones, primary linkages and relative volume of traffic between departments. As discussed above ideally out-patient and clinical services should be on one level. Similarly theatres/CSSD, intensive care, surgical inpatients should all be closely grouped and on the same floor.
As the hospital support or industrial zone will have heavy vehicle deliveries and is often a noisier area, it needs to be located away from other hospital clinical areas and be linked to a slip road off the main entrance. Direct deliveries are also made into a security cage linked directly to the pharmacy.
Diagram above shows primary links between departments and relative weighting of traffic volumes
Space syntax/ SA diagram of flow between departments Travel and circulation
Designing for expansion
Inclusive design
Requirements:
A. Healthcare facilities need to be designed so that all access pathways, circulation and facilities are fully enabled for those with any form of disability.
A larger proportion of those using health services than average in the normal population will be impaired in one way or another, either on a temporary or a permanent basis. It is therefore essential that access to the site, movement on the site and access to buildings is well considered to ensure the access pathways are fully enabled for both the impaired as well as the unimpaired population. Site access issues include the following:
- access routes from drop off and parking areas to hospital admission, emergency and outpatient services should be direct and as short as possible, be visibly coherent and suitably signposted with no cross over traffic
- site access pathways should be suitably graded and without steps, should have appropriate finishes to be safe for use in all weather conditions
- finishes should also be used to demarcate routes and identify gradients or ramps and any transitions where there may be potential danger, and
- access routes and parking areas need to be well lit and safe.
Inclusive design is covered in detail in the IUSS GNS document Inclusive environments.
Building design
Good design principles
Buildings, as for any product, need to be carefully considered during the design conceptualisation and development phase. Good design is characterised in that it:
- is innovative - new technology always offers new opportunity for innovation, however innovative design develops in tandem with new technology and can never be an end in itself
- makes a product useful - the building needs to satisfy certain functional, psychological, and aesthetic criteria; good design emphasizes the usefulness of the building while disregarding what could detract from it
- is aesthetic - the aesthetic quality of a building is integral to its usefulness; the aestheticusability effect tells us that the designs people find more aesthetically pleasing are easier to use than the designs they find less aesthetically pleasing.; people form quick, even instant impressions and aesthetics matter in that instant
- makes a product understandable - It clarifies the building making it self-explanatory; structure itself can explain the different parts of the whole; Information architecture; meaningful and easily understandable navigation labels to help visitors find what they want
- is unobtrusive - health buildings are not intended to be just decorative objects or works of art - design should be both neutral and restrained; focus on solid design principles – good design does not distract visitors with your design; people visit a site for its content, not the design
- is simple and direct. Focus on simplicity; don’t call attention to your design - design to call attention to the what the building’s purpose is; everything should work together in harmony to support the intentions of the building is honest...
- is long-lasting ...
- is thorough down to the last detail...
- is environmentally friendly ...
- is as little design as possible.... [EF / Dieter Rams (1985)]
Generic design
Change from ‘modular design’ heading
Pick up ‘enabling life cycle efficiency’ chapt 8 principles: change over time, flexibility, sustainability, …
3 aspects – generic spaces, standardised room sizes and use of planning grids
IUSS std room sizes are entirely random – depth and width; one possible (optimum?) enclosure for activities?
NHS now recommending set of standardised room sizes – allow for change over time; all on 300mm sub-module, either on 3,6 or 3,9 main module; guide shows two room depths for each: 3,5/4,6 for
3,6 module, 3,2/4,25 for 3,9 module
Options:
• Follow NHS – review std rooms
• Use 2 std depths, width in 300mm increments
…
Modular design can be used at building level where the full facility is designed according to a fixed grid or where individual rooms or sets of rooms are designed to fixed sizes
Health buildings, designed initially to a fixed schedule of accommodation, need also to allow for flexibility in use over time as service requirements will change and spaces or departments will need to be repurposed to provide for new functions.
There is a need to establish the right balance between a tight fit design where each space is designed to its minimum requirements with a potentially lower initial capital cost and the use of standard planning grids which accommodate a small range of standard potentially interchangeable clinical and clinical support functions allowing later reconfiguration[1].
- has proved beneficial in reconfiguration of spaces for other purposes. This is also supported by Diamond et al (2006) in their report for the NHS, and more recently in the latest version of the UK Health Building Notes which proposes a small range of room sizes (12, 16 and 32m2) that fit with standard planning grids for clinical and clinical support functions (Department of Health Gateway Reviews Estates & Facilities Division 2010, p. 1)
- Khoo Thek Puat – modular design/ room sizes
Ergonomics
Requirements:
A. Hospital design professionals need to ensure that all aspects of the building are designed and signposted so as to ensure that access routes and pathways are clear and unambiguous to all users.
Ergonomics is defined by the International Ergonomics Association as being “…the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance” (IEA, 2014).
Poorly designed recurring elements such as workstations and the layout of critical rooms have a great impact on the occupational health and safety (OHS) of staff and the welfare of users.
There are five principles to consider when designing ergonomic spaces:[13]
- Safety
- Comfort
- Ease of use
- Productivity/performance Aesthetics.
All buildings (including external spaces) are to be designed to avoid protuberances which may cause slips and falls. For example, window sashes should not open into walkways in a way that can interfere with the path of a person walking past.
All workspaces should be adaptable to the users occupying that space. Therefore they should be capable of adjustment or modification to suit that user. For instance, conventional work-surface heights for seated users are not suitable for people who use wheelchairs, and in this case dual-height surfaces should be provided. Bench heights and widths in laboratory and similar work areas should be designed taking into account the type of work to be performed in this space.[14]
Building engineering services
Infection prevention and control
Direction and way-finding[15]
Requirements:
A. Hospitals need to be designed and signposted so as to ensure that access routes and pathways are clear and unambiguous to all users.
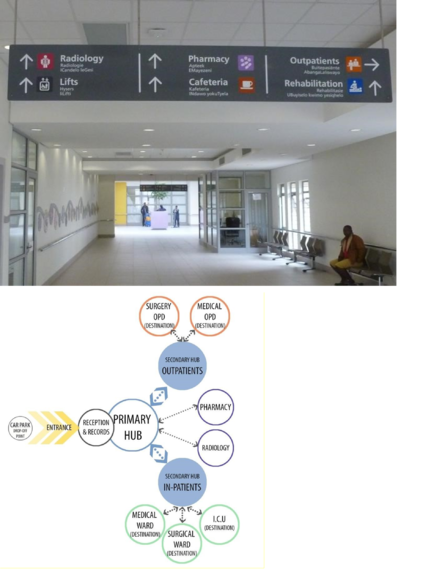
Hospitals are complex structures comprising a large number of primary and secondary destinations for a range of first time, repeat and frequent users including patients and accompanying persons, visitors, permanent and visiting clinical staff and administrators, hospital based and visiting technical, maintenance and domestic support staff. Routes leading each individual to their specific destination during normal and emergency use need to be clear and unambiguous.
As hospital buildings become larger and more complex it becomes more difficult for users to navigate their way through the building to and from their intended destination. Poor way-finding systems can increase anxiety, confusion and dissatisfaction with a person’s hospital experience.
The complexity is increased as while the majority of destinations are fixed for most of the life of the hospital, hospitals are not static systems and new departments can be added or existing departments may be altered, added to, consolidated or moved over time requiring existing pathways and destinations to be adjusted and new pathways to be identified.
Way-finding systems usually comprise:
- architectural features and design elements that provide clues as to what the function of the building is and can include landscaping, sculptural features, architectural interior design, floor covering, lighting, wall, door and window graphics
- architectural form and transparency through which users can easily orientate themselves along a particular route. This usually includes building shape and views from corridors into external areas or courtyards
- permanent signage
- digital devices (e.g. kiosks or information screens)
- human interaction (e.g. human interaction at help desks), and
- printed information (pamphlets).
Way-finding systems need to be clear and simple and should comprise a mutually reinforcing group of visual clues that enable people to make navigational decisions. Core principles should incorporate the following:
- design that includes for everyone and especially the more vulnerable such as o the first time visitor o those that are physically challenged or have other forms of impairment, and o children and the aged
- utilising ‘key hub’ destinations along a complex journey. A person is directed to a primary hub destination, then directed to a secondary hub destination from that point
- clarity of layout with external views to assist with orientation
- utilisation of standardised information systems, and
- use of standardised names, numbers and symbols.
Way-finding and signage are interrelated and must be considered from the inception of the design process.
Way finding orientation
Way-finding maps should be located at strategic points throughout the site and allow visitors to orientate themselves. The maps should be consistent with the signage and the typology needs to be clear and concise. Maps need to be located on all floors and be strategically placed at floor access nodes throughout the building. Figure below shows examples of such maps at Mitchells Plain Hospital.
Signage
Signage is a critical ‘wayshowing’ component of wayfinding. The following aspects need to be taken into account:
- information displayed on signs needs to be organised and presented in a logical, sequential layout
- directional signs should generally contain a maximum of five destinations
- key hospital hub destinations should be listed at the top of the hierarchy or highlighted as primary information
- secondary destinations should be presented lower in the information hierarchy
- destinations on signs should be grouped and ordered with logic relevant to the destinations listed; either in alphabetical order by the direction to the destination in clockwise order, or by the order of distance to destination (closer destinations first)
- connect labels (destinations) to arrows
- arrow designs should be based on the ISO arrow (ISO 7001), and
- colour-coding of floors or as a method of differentiating space may be used, however, people do not always perceive the colour use to have significance. This is worse for people that are colour blind. It is however, a useful component of the wayfinding system.
Signage should:
- use accessible terminology – common references that everybody understands
- avoid the use of acronyms and use universally understood symbols
- provide clear contrast between the information content and its surrounding environment, and
- have a finish that does not detract or obscure the signs intention.
Signposting shall clearly identify staff, patient and visitor areas, and draw attention to restricted areas.
The use of pictograms in conjunction with written names is recommended. The health team at Western Cape Department of Transport and Public Works has developed a logical and clearly understood standardised set of pictograms for use in Western Cape Provincial healthcare facilities[5]
Where possible signage should be done in an appropriate selection of the official languages of South Africa. In the Western Cape provincial policy is for signage to be in the 3 dominant languages, English, Afrikaans and isiXhosa. This three language option is more difficult to achieve in provinces where there are more than three dominant languages. Refer to local provincial policy.
Further detailed guidelines and information on wayfinding and signage is also contained in Part D of the IUSS GNS document Inclusive environments.
Inclusive environments
Site level accessibility
Buildings
Safety and security
Common public areas
Entrances
Avoiding prison-like/oppressive environment (normativeness):
Since the late 1950s it has been recognized by facility operators and specialist how debilitating the physical design of facilities can be. The recognition led to the development of a concept called “normativeness” which set as a goal the development of designs where the design of the environment was not oppressive because of its desire to be both functional and secure. This underlying concept of normativeness can be applied to the architecture of health care facilities by setting the security design goal as one that must achieve this “normativeness”. For all intent, this means the challenge put before the facility’s designers, be it for existing, new or proposed, is to find ways and means of achieving physical security without creating a prison like environment.
Supplies, storage and distribution
Building engineering systems
Building engineering systems design
Further more detailed information is included in the IUSS-GNS document Building engineering systems.
Compliance
Requirements:
A. The design must comply in all respects to the latest version of the National Building Regulations and all other legislation, regulations and standards relevant to the development of buildings for health service delivery
Compliance with the latest version of the National Building Regulations is required. Where any apparent conflict between the functional requirements and the “deemed to satisfy” guidance emerges, the rational design route to regulatory compliance would need to be followed so as not to compromise any system’s functionality.
As indicated in section 3.4.1 above the hospital must comply with the requirements set by the Office of Standards Compliance. Periodic inspections will be undertaken to ensure compliance.
Annexure xx provides a list of relevant legislation related to the provision of health services and health service facilities. Note that while this list is extensive it is not necessarily comprehensive nor fully up to date. The onus is on the design team to ensure that they acquaint themselves with all relevant current legislation.
Reference is also made in most of the IUSS GNS documents to legislation, regulations and standards specifically pertaining to that aspect of a health care facility.
Maintenance
Other – to be included...
Fire
Operational policy – impacting design – EF’s inpatient doc
Operational design header – policy, management, maintenance,
Functional design
Building
Setting design targets
Good design is the end product of a process of g
72 hour observation – ref
Supporting Information
Research literature:
The following references provide more background reading on topics covered in this guide.
Patient focussed/centred care
• What is Patient-Centred Healthcare: A Review of Definitions and Principles. International Alliance of Patients’ Organisations, London, 2007.
• Australian Commission on Safety and Quality in Healthcare Patient-centred Care: Improving quality and safety by focusing care on patients and consumers. Discussion paper, Draft for public consultation, September 2010 (ACSQH, 2010)
Evidence based design
How Hospital Gardens Help Patients Heal: Scientific American / Nature that nurtures – gardens; view - D:\1 Client & Contract\IUSS et al\1 Norms and standards\3 Cross cutting\02 Hospital design principles\Literature
Evidence-Based Healthcare Design
Evidence based design - D:\1 Client & Contract\IUSS et al\1 Norms and standards\3 Cross cutting\02 Hospital design principles\Literature\Evidence based design – Ulrich et al, 2008
Flexibility and adaptability
• Carthey, J., Chow, V. & Wong, M. 2010, Health Infrastructure Future Directions: Flexible and Adaptable Hospitals ‐ Lessons from Selected NSW Case Studies to Inform Future Health Projects, Centre for Health Assets Australasia, UNSW, Sydney
• Carthey, J., Chow, V., Jung, Y.‐M. & Mills, S. 2009, Flexibility and Adaptability Report: An International Review for the NSW Context, Centre for Health Assets Australasia, UNSW, Sydney.
• Carthey, R
16.5 Wayfinding and signage
- Growth Solutions Group: Specialist clinics wayfinding guidelines: The outpatient journey: August 2008 www.gsg.com.au
- Reading list on Wayfinding – ACHSM
- www.achsm.org.au/DownloadDocument.ashx?DocumentlD=214
- Western Cape Provincial Government, Department of Transport and Public Works (2011): Design Guidelines for Health Facilities: Way-finding and Signage.
- David Gibson:2010. The Wayfinding Handbook. Princeton Architectural Press. New York
References
- Australian Commission on Safety and Quality in Healthcare Patient-centred Care: Improving quality and safety by focussing care on patients and consumers. Discussion paper, Draft for public consultation, September 2010 (ACSQH, 2010)
- Health Systems Trust web site (publications), introduction to NHI Green Paper (HST.org.za,2014) http://www.hst.org.za/publications/green-paper-national-health-insurance-southafrica
- Dilani, A Prof. Psychosocially Supportive Design: A Salutogenic Approach to the Design of the Physical Environment. 1st International Conference on Sustainable Healthy Buildings; Seoul, Korea. 6 February 2009
- Carthey, J., Chow, V. & Wong, M. 2010, Health Infrastructure Future Directions: Flexible and
Adaptable Hospitals ‐ Lessons from Selected NSW Case Studies to Inform Future Health Projects, Centre for Health Assets Australasia, UNSW, Sydney
- Carthey, J., Chow, V., Jung, Y.‐M. & Mills, S. 2009, Flexibility and Adaptability Report: An International Review for the NSW Context, Centre for Health Assets Australasia, UNSW, Sydney.
Papers, articles
Web sites
HST.org.za, 2014 http://www.hst.org.za/publications/national-health-insurance-conferencereport-lessons-south-africa
Please help to expand this page. |